It is important to remember that the majority of patients with sexually transmitted diseases are asymptomatic.
Therefore, taking a sexual history can be very important. Please see my post How To Take A Sexual History – Help From The Centers For Disease Control And Prevention (CDC)
Posted on November 29, 2018 by Tom Wade MD.
The above post contains a script from the CDC that you can use to take your sexual history.
So the first question in asymptomatic patients is: Who should we screen for STDs?
What follows are excerpts from the outstanding Syphilis – CDC Fact Sheet (Detailed):
[Syphilis in Pregnant Women And In Infants born to Mothers Positive For Syphilis
Special note: Because untreated syphilis in a pregnant woman can infect and possibly kill her developing baby, every pregnant woman should have a blood test for syphilis. All women should be screened at their first prenatal visit. For patients who belong to communities and populations with high prevalence of syphilis and for patients at high risk, blood tests should also be performed during the third trimester (at 28–32 weeks) and at delivery. For further information on screening guidelines, please refer to the 2015 STD Treatment Guidelines. 3
All infants born to mothers who have reactive nontreponemal and treponemal test results should be evaluated for congenital syphilis. A quantitative nontreponemal test should be performed on infant serum and, if reactive, the infant should be examined thoroughly for evidence of congenital syphilis. Suspicious lesions, body fluids, or tissues (e.g., umbilical cord, placenta) should be examined by darkfield microscopy, PCR testing, and/or special stains. Other recommended evaluations may include analysis of cerebrospinal fluid by VDRL, cell count and protein, CBC with differential and platelet count, and long-bone radiographs. For further guidance on evaluation of infants for congenital syphilis, please refer to the 2015 STD Treatment Guidelines. 3
Who should be tested for syphilis?
Any person with signs or symptoms suggestive of syphilis should be tested for syphilis. Also, anyone with an oral, anal, or vaginal sex partner who has been recently diagnosed with syphilis should be tested for syphilis.
Some people should be tested (screened) for syphilis even if they do not have symptoms or know of a sex partner who has syphilis. Anyone who is sexually active should discuss his or her risk factors with a health care provider and ask whether he or she should be tested for syphilis or other STDs.
In addition, providers should routinely test for syphilis in persons who
- are pregnant;
- are sexually active men who have sex with men (MSM);
- are living with HIV and are sexually active;
- are taking PrEP for HIV prevention.
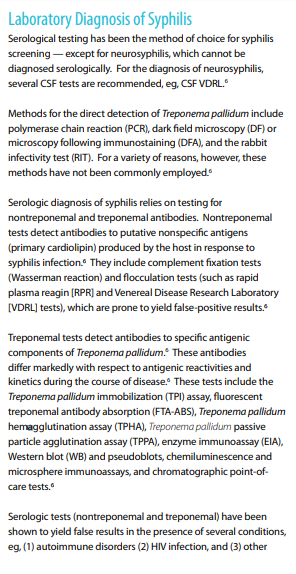
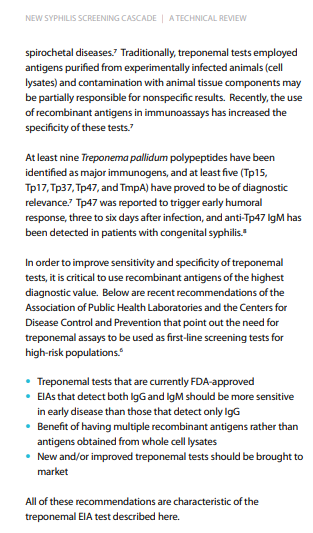
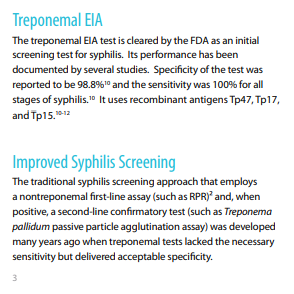
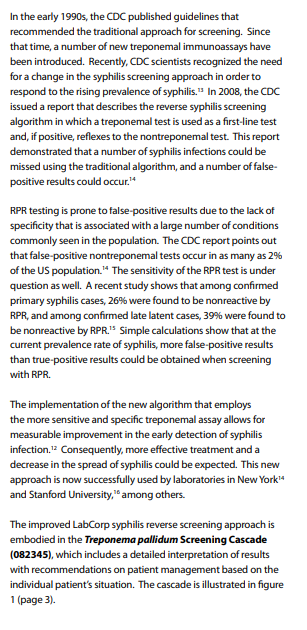
The second question is: How Do We Make A Laboratory Diagnosis Of Syphilis
The following are excerpts on laboratory diagnosis of Syphilis diagnosis from LabCorp‘s Improved Syphilis Reverse Screening Cascade: Earlier Detection With Fewer Ambiguous Results:
And the third question is: What symptoms should lead us to consider a diagnosis of possible syphilis and order the appropriate tests?
And the following reference will help us answer that question.
#127 STIs Syphilis, Gonorrhea and Chlamydia
NOVEMBER 26, 2018 By MATTHEW WATTO, MD
And here are excerpts from the above reference.
STI – Clinical Pearls
- Make the sexual history routine. Get comfortable with a common script that you ask your patients, and do not be deterred by an initial vague answer.
- Leave the “screening door open”. Tell the patient “if anything ever changes” they can come to you.
- Most people with any STI you can name have no symptoms. A basic principle is that many carriers of these pathogens are asymptomatic even while spreading to others.
- We are currently in a syphilis epidemic, particularly in men who have sex with men (MSM). That said, we must consider syphilis in heterosexual men and women with risk factors including: new or multiple partners, and commercial sex work.
- Syphilis really is “The Great Pretender”. It can mimic other dermatologic or systemic disease (see DDx below). Patients may develop diverse manifestations of secondary and late syphilis without recalling or presenting to care for an earlier stage of infection.
- Gonorrhea and chlamydia NAAT testing: Test at all sites exposed! Send urine for men. Send endocervical or vaginal swabs for women (the latter can be self collected). Send throat or rectal swabs if oral or anal receptive intercourse.NOTE: Urine NAAT less sensitive than vaginal swab for women.
- Routine STI panel: Chlamydia, gonorrhea, HIV, syphilis (either RPR or treponemal antibody), Hep B, Hep C, +/- herpes antibody.
- Don’t forget to report diagnoses of sexually transmitted infections, including syphilis, gonorrhea, and chlamydia.
Syphilis
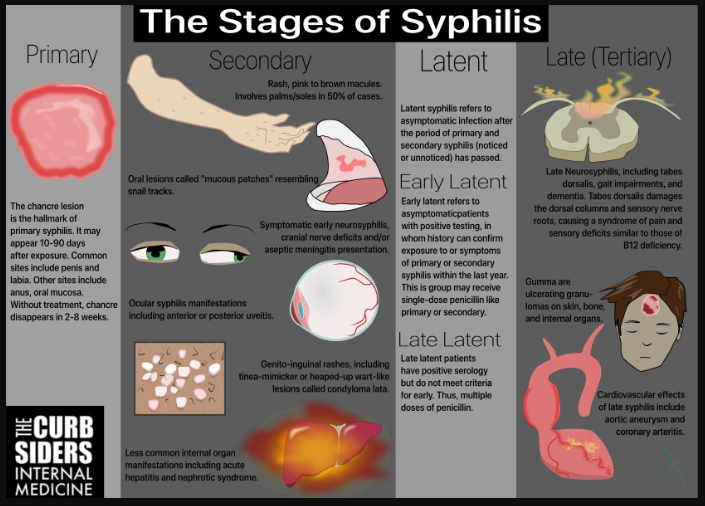
Primary syphilis
TRANSMISSION/INCUBATION
After contact with an infectious lesion on an infected individual, there is a 30% likelihood that the exposed person will contract syphilis. The average incubation from contact to the chancre is about 30 days, but ranges from 10 to 90.
CHANCRE
Primary syphilis presents classically with a solitary lesion called a chancre. The chancre starts as a papule at site of inoculation. This usually occurs on mucous membranes, with common sites including the lower third of labia and penile shaft. Chancres can also form in the anus in those exposed through anal receptive intercourse, and can also occur in the mouth after receptive oral intercourse. There are case reports of lesions on the breast and hands, but these are rarer. A chancre will disappear without any treatment in 2-8 weeks.
CHANCRE VS CHANCROID
Over time, the initial papule ulcerates, yet is classically painless. It is sometimes referred to the “hard chancre,” because it is firm if squeezed. This firmness and painlessness are attributable to T. pallidum’s ability to produce a more limited immune response, with some plasma cells, lymphocytes, and the deposition of collagen. In Dr. Dunne’s words, it does not make “much of a ruckus.” A mimicking condition caused by a Haemophilus species called “chancroid” is softer, painful, and more purulent, which are attributable to the more robust immune response this organism creates compared to syphilis.
Secondary syphilis
Spirochetes then replicate again and disseminate hematogenously. Collectively, the manifestations of this spread to distant sites are termed secondary syphilis.
DERMATOLOGIC MANIFESTATIONS OF SECONDARY SYPHILIS
One key, typical symptom of secondary syphilis is a rash. This rash can be found diffusely over the body or in more limited distributions, sometimes only a few macules. Importantly, this rash can involve the palms and soles, though only does so about half the time. In other words, involvement of the palms and soles in a host with risk factors should generate a high positive predictive value for syphilis, though the absence of this finding may not fully exclude the possibility. The typical lesions of this rash are copper-colored macules, though can appear more hyperpigmented in people of darker skin. In Dr. Dunne’s experience, these macules seem to be more hyperkeratotic in patients with HIV. The dry lesions on the palms are not high yield for seeing organisms on dark field. Thus, Dr. Dunne would not be concerned about shaking hands in the context of these lesions, and there has not been a signal identified for nosocomial spread via this route.
ORAL LESIONS
Oral lesions may also be noted in secondary syphilis (note that this is regardless of whether direct exposure or chancre formation occurred in the mouth). “Mucus patches” are lesions found often on the lips, tonsils, or posterior pharyngeal wall, which may have the appearance of “snail tracks” crawling over the area. These lesions can be subtle in appearance, yet are highly infectious.
OTHER DERMATOLOGIC MANIFESTATIONS
In the scrotum, secondary lesions can form which initially may be subtle. They may initially mimic tinea cruris or eczema, and thus be easy to miss. Eventually, some patient develop heaped up lesions in intertriginous areas under breast, groin, gluteal cleft known as Condylomata lata. These are whiter, flat-topped, and may resemble warts. These are particularly teeming with organisms and thus infectious.
Alopecia areata, a form of patchy hair loss, may also be seen.
NON-DERMATOLOGIC MANIFESTATIONS OF SECONDARY SYPHILIS
In addition to mucocutaneous manifestations, secondary syphilis may also impact other organ systems.
Symptomatic early neurosyphilis
Secondary syphilis affecting the nervous system is referred to as “symptomatic early neurosyphilis.” This may include various cranial nerve palsies, including sensorineural hearing loss with or without vertigo. Aseptic meningitis may also occur. In Dr. Dunne’s experience, some such patients may experience mild constitutional symptoms like malaise and adenopathy. Consequently, patients may attribute their symptoms to a respiratory virus and not present for care.
Ocular syphilis
Ocular syphilis may manifest as anterior or posterior uveitis. Do not forget to consider syphilis in an at-risk host. Take a sexual history when a patient presents with an ocular concern.
Syphilitic hepatitis
Syphilitic hepatitis may develop, which classically presents with an alkaline phosphatase elevation out of proportion to transaminase elevation.
Nephrotic syndrome
Nephrotic syndrome may also occur!
Latent Syphilis
Latent syphilis refers to those people infected beyond the period of primary and secondary infection. In other words, these patients will have diagnostic tests consistent with ongoing infection, have not been previously treated, and will not have symptoms consistent with primary or secondary syphilis.
Early latent syphilis
Early latent syphilis is a term for patients who meet criteria for latent syphilis, but are within one year of initial infection. The reason for making this delineation is the effect on treatment. These patients can be treated with a single dose of penicillin identical to the regimen for primary or secondary syphilis. The onus is on the provider to become confident that the patient is within this window, either via documented seroconversion (i.e. negative a year or less ago and now found to be positive), documented or confidently reported prior symptoms that have since resolved (e.g. “I had a chancre six months ago”; “I had a syphilis infection in my eye three months ago and now I have no symptoms”).
For any patients for whom the time since infection has been longer than one year or the timing is unknown, they are presumed to have late latent syphilis, and thus would require the full regimen e.g. once weekly doses of penicillin for three weeks.
Late Syphilis
Of those with latent syphilis, 25% will go on to have late syphilis. Manifestations include:
- Tabes dorsalis
- General paresis
- [Optic Atrophy]
- Cardiovascular – aortic root dilation, coronary arteritis
- Gummatous disease: formation of ulcerative granulomas in the skin, bone, and internal organs.
NOTE: Patients with late syphilis should be referred to an infectious diseases specialist.
Differential diagnosis for syphilis
Acute HIV could also manifest as rash with vague constitutional symptoms in a host with similar risk factors.
Disseminated gonococcus may also cause rash, and has similar risk factors. Rather than the often-diffuse, more symmetrically distributed rash of syphilis, disseminated gonococcus usually causes tender pustules with a few peripheral lesions.
Rocky Mountain Spotted Fever is on the differential, particularly as another cause of rash involving the palms and soles. Host factors that should increase pretest probability include tick bites, or hiking. Of note, RMSF is not commonest near the Rocky Mountains, but rather in the mid-Atlantic states and in states around the Mississippi River Valley.
Atypical Measles is another syndrome of rash and fever, myalgias, and headache that may resemble the above, but is rare in the era of modern immunization programs.
#121 HIV Care for the Internist
OCTOBER 22, 2018 By MATTHEW WATTO, MD
#41: HIV, PrEP, and STI screening
MAY 29, 2017 By MATTHEW WATTO, MD