My takeaway from this excellent post is that there are persons walking around with undiagnosed, unrecognized pulmonary hypertension. And these patients can appear in the ED sick but not that sick. If they need intubation, they can unexpectedly arrest during or following a rapid sequence intubation.
The podcast has excellent information on when to suspect undiagnosed pulmonary hypertension in an undifferentiated sick ED patient.
And the podcast and show notes are full of what you need to know and do for a patient requiring intubation whom you know or suspect has pulmonary hypertension.
The reason I reviewed this podcast again at this time is that I just listened to Dr. Weingart’s post EMCrit RACC Podcast 216 – The Hemodynamically Neutral Intubation
January 22, 2018.
And when forced to intubate a patient with pulmonary hypertension, you should be afraid (really meaning just very thoughtful and very careful) and this is one of the patients that would clearly benefit from the Hemodynamically Neutral Intubation of Podcast 216 if you are forced to intubate the patient.
The show notes for this podcast are outstanding and should be reviewed before or after listening to the podcast because they are full to the brim with clinical pearls.
But the podcast itself is so full of clinical pearls that I’ve listened to it several times and embedded a link to remind myself to listen again:
Here is Podcast 181:
Because the show notes are so perfect, I just need to review the complete show notes [as this blog is simply my peripheral brain]. What I’ve done below is to transcribe just the first six minutes of this 26 minute podcast.
Dr. Weingart leads off by saying:
[Pulmonary hypertension] is an unrecognized disease, an unrecognized syndrome. It can easily cause a clean kill-the patient who came in talking and goes out dead. So it is definitely a topic we need to cover on EMCrit.
Dr. Wilcox has written the outstanding article cited as Resource (2). She became interested in the topic because
When I was an attending a couple of years ago a patient came in [and] she got all the textbook perfect quote-unquote medical care and she died. She coded and died.
In retrospect, she had RV failure from severe chronic pulmonary hypertension.
And so all the things that we did to resuscitate her killed her.
So giving her big fluid boluses, intubating her, etc, etc. That was exactly what you shouldn’t have done.
And so that [case] was what prompted me to write the article.
Dr. Weingart observes:
This [disease, Pulmonary Hypertension,] is scary because these people are walking around among us unidentified; just acting as ticking time bombs.
So my first question to you is Who should I suspect it in? How do identify this disease?
What would make me think, in an undifferentiated ED patient who just comes in sick, actually is a pulmonary hypertension patient.
Dr. Wilcox says:
That is one of the scariest parts. You often don’t know [that this is a patient with (undiagnosed) pulmonary hypertension. Looking at the literature it is extremely under reported even when we have all of the data in front of us.
And so the most common cause of pulmonary hypertension in the United States is from left sided heart failure leading to Group II pulmonary hypertension.
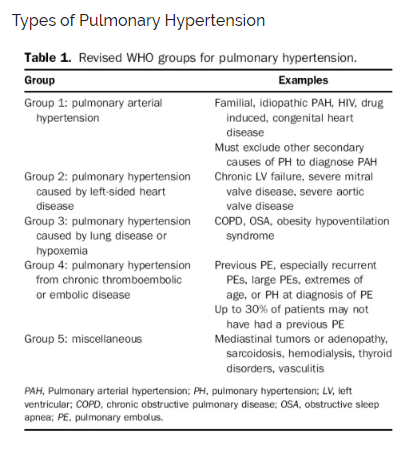
Dr. Weingart then goes through the types of pulmonary hypertension:
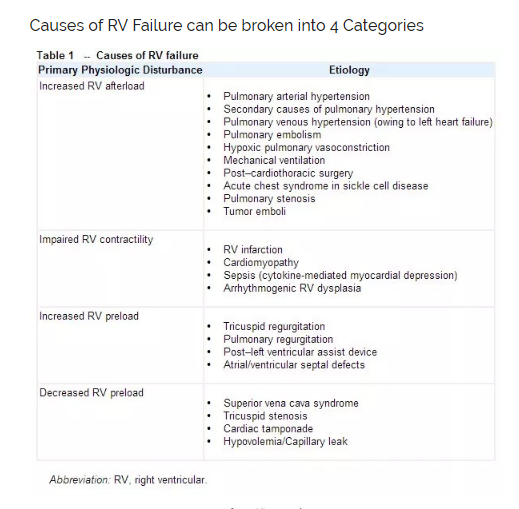
And here are the causes of RV failure:
Dr. Wilcox continues:
And so anybody who has left-sided heart failure is especially at risk.
But then the next most common causes are from the hypoxemic causes like COPD is another one of the most comon causes. And obstructive sleep apnea is an increasingly common cause.
And so anybody who has any sort of underlying respiratory problems like COPD, any sort of interstitial lung disease and some of the rheumatologic diseases (like lupus, sarcoidosis, etc.). Those kinds of conditions really predispose people to pulmonary hypertension.
So those are the ones where I already have a high index of suspision just from knowing a little bit about their history.
The other ones that are probably the patients that are under-recognized are the people who keep coming in with dyspnea without a clear cause.
And so there is a little bit of data that those patients might have pulmonary hypertension that no one has picked up on. It has been documented that it can take up to two years for people to diagnose someone correctly with pulmonary hypertension.
And for those patients who keep coming back and no one can find a clear diagnosis those are definitely patients where I would worry that that patient has have undiagnosed pulmonary hypertension or maybe even some element of RV failure.
Dr. Weingart reminds us that Dr. Wilcox in her article, Pulmonary Hypertension and Right Ventricular Failure in Emergency Medicine
You made a point a couple of times to point out that if some one comes in with dyspnea on exertion, syncope, or the combination of both [then] that is a group that we should again have a high index of suspicion [of pulmonary hypertension]. Is that true?
Dr. Wilcox replies:
Oh yeah. Absolutely. And I think that in reading a lot as I was studying this and getting ready to write this article, I really changed my own practice.
Because previously a patient comes in with syncope or dyspnea with exertion you do all of the right things. You get the EKG, you check the troponin. You may even get a BNP, the chest x-ray; maybe even a CT scan to look for a PE.
When all of that stuff comes back reassuring I always felt good; we’re done. You’ve given them a good workup and everything looks fine.
Now I’m realizing that we should be more worried, certainly with a patient that might have pulmonary hypertension and syncope.
And even our patients that have a good workup, I’ll now refer to echocardiogram as an outpatient.
Dr Weingart asks say we have a suspicion of pulmonary hypertension, how do we screen in the ED. And the talk continues from there.
Resources:
(1) Podcast 181 – Pulmonary Hypertension and Right Ventricular Failure with Susan Wilcox September 5, 2016 by Dr. Scott Weingart.
(2) Pulmonary Hypertension and Right Ventricular Failure in Emergency Medicine [PubMed Abstract] [Full Text PDF]. Ann Emerg Med. 2015 Dec;66(6):619-28. doi: 10.1016/j.annemergmed.2015.07.525. Epub 2015 Sep 3.
(3) EMCrit RACC Podcast 216 – The Hemodynamically Neutral Intubation
January 22, 2018 by Dr. Scott Weingart