In this post I review emergency management of a Can’t Miss Diagnosis: Acute Glomerulonephritis.
First I review two relevant diagnostic schemas from the Clinical Problem Solvers.
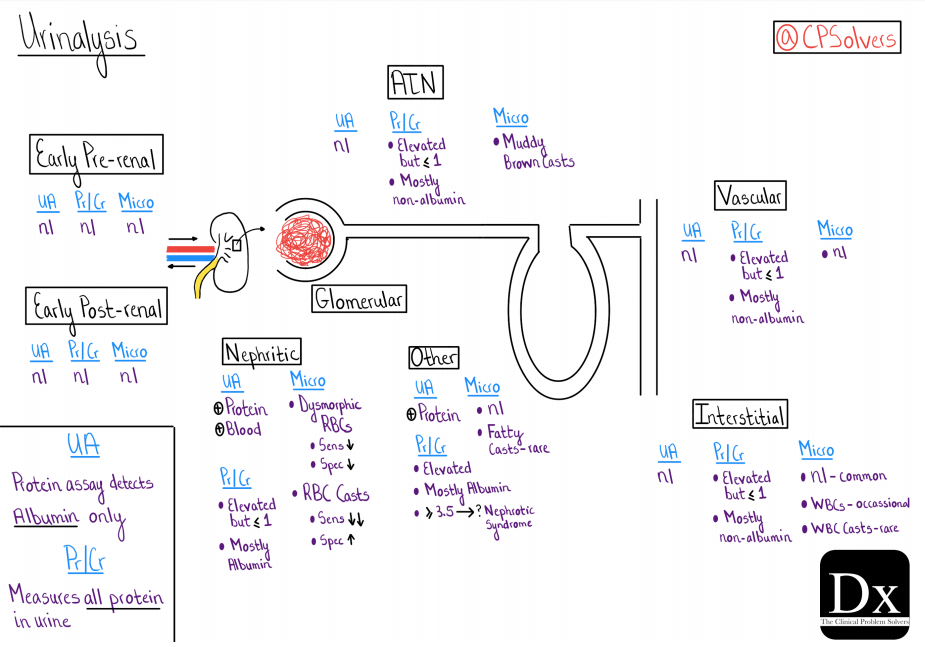
The first is the Diagnostic Schema for Urinalysis [link is to the PDF] from the Clinical Problem Solvers‘ Episode 21 – Intrarenal Acute Kidney Injury with Dr. Restrepo:
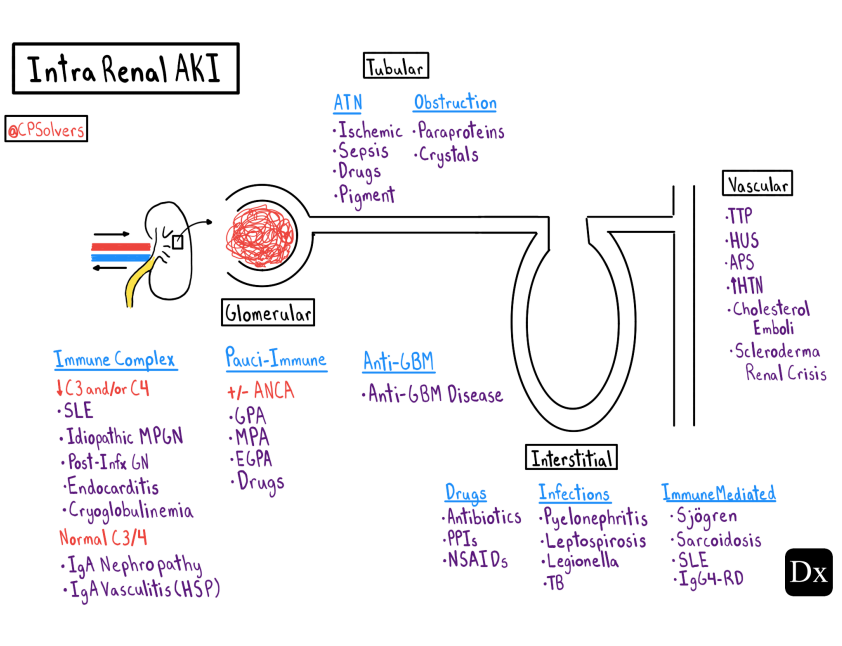
Here is the Diagnostic Schema for Intrarenal Kidney Injury [Link is to the PDF] from the Clinical Problem Solvers‘ Episode 21 – Intrarenal Acute Kidney Injury with Dr. Restrepo:
Here are excerpts from the Medscape article, Emergent Management of Acute Glomerulonephritis:
Overview
This article concentrates on the emergency management of acute glomerulonephritis. For more detailed information, refer to Acute Glomerulonephritis.
The emergency physician must consider acute glomerulonephritis in the differential diagnosis for patients that present with hypertension, hematuria, proteinuria, peripheral edema, and/or acute pulmonary edema. Acute glomerulonephritis is defined as inflammation and subsequent damage of the glomeruli leading to hematuria, proteinuria, and azotemia; it may be caused by primary renal disease or systemic conditions. The glomerular filtration rate is decreased, leading to activation of the renin-aldosterone system and subsequent salt and water retention, resulting in edema and hypertension.
A urinalysis must be included in the workup for these patients, because if acute glomerulonephritis is not considered, the diagnosis will be missed. Some patients may require intubation or noninvasive ventilation in cases of severe pulmonary edema.
The prevalence of poststreptococcal glomerulonephritis (PSGN) is decreasing worldwide, but it is still the leading cause of glomerulonephritis in children.
Systemic lupus erythematous (SLE) is an important cause of kidney disease, including acute glomerulonephritis. SLE must be considered in a patient who presents with any of the following symptoms: arthralgias, malar rash, photosensitive rash, pleurisy, or oral and nasal ulcers.
Henoch-Schönlein purpura (HSP) may present with purpuric rash on the legs, arthralgias, and abdominal pain. HSP is small-vessel vasculitis that most commonly presents in patients younger than 20 years. Renal involvement may not be present initially, but the likelihood increases with time and is more likely in patients with persistent rash and abdominal pain. [1] For further information, refer to Henoch-Schonlein Purpura
[Formerly known as] Wegener granulomatosis [but now called Granulomatosis With Polyangitis] should be considered in any patient with nonspecific complaints, such as weight loss, malaise, arthritis, and upper and/or lower respiratory tract complaints (from sinusitis to pulmonary hemorrhage). There may be cavitating lung lesions seen on chest radiographs. Wegener granulomatosis most commonly occurs in patients in their sixth to seventh decade, with equal distribution among men and women.
Consultations
Any patient suspected of having acute glomerulonephritis should have their urinary sediment evaluated by a skilled nephrologist. [8] Further urine and serum studies will likely be recommended by the nephrology service to help determine etiology. Urgent nephrology consultation is required if patient requires emergent hemodialysis*.
*Please see Indications for Dialysis: A Mnemonic And Explanation. August 1, 2012 . By: Neal Shah, Co-Editor-in-Chief from St. John’s University College of Pharmacy and Health Sciences.
If a patient is suspected to have acute glomerulonephritis or renal disease from systemic lupus erythematous (SLE), consultation with a rheumatologist is warranted. These patients may benefit from therapy with high-dose steroids (ie, pulse therapy).
Disposition
Definitive diagnosis of glomerulonephritis caused by intrinsic renal disease can only be made after biopsy has been performed. Patient suspected of having acute glomerulonephritis should be admitted for further workup and possible renal biopsy, as delay in diagnosis can lead to significant morbidity.Patients who present with hematuria only, without renal impairment, severe hypertension, fluid overload, hemoptysis, or any other concerning symptoms can be sent home with thorough follow-up instructions and close follow-up with a nephrologist.