The following are excerpts from Resource (1), Ketogenic diet for obesity: friend or foe?:
1. Introduction
Obesity is a rapidly growing epidemic worldwide [1] that has nearly doubled since 1980.
Regarding obesity interventions, diet is one of the more controversial issues and many different types have been advocated for weight loss, but there is little scientific evidence to recommend one diet over another. As a matter of fact there are
still no definitive data on what dietary protocols are most effective in both the short and long term [6], or even what is the correct nutritional approach in general [7].[The problem is that regardless of the type of diet prescribed most people who begin a diet fail to lose weight because they can’t stick to it. And of those who do lose weight almost all of them regain the weight subsequent to resume a more normal diet. It is thought that dieting reduces the resting metabolic rate so that the person must eat many fewer calories after the weight loss diet to maintain the weight gain]
As a consequence of the debatable efficacy of [any of] these types of diet, there has been increased interest in recent years in very lowcarbohydrate ketogenic diets (VLCKDs) or simply ketogenic diets (KDs).
2. Ketogenic Diets in the Clinic
Even though the ketogenic diet may be useful as part of the treatment of various diseases (see Paoli et al. [11]), especially in pediatric pharmacoresistant epilepsy [12], the more common
situation for the general practitioner is the use of KD by patients in order to lose weight. KDs have undoubtedly been shown to be effective, at least in the short to medium term, as a tool to fight
obesity [13], hyperlipidemia and some cardiovascular risk factors [14–16], but ketogenic diets also raise some concerns among physicians [17]. Many of the concerns about the use of ketogenic diet as therapeutic tools could be attributed to a broad lack of knowledge about the physiological mechanisms
involved. Ketogenic diets induce a metabolic condition named “physiological ketosis” by Hans Krebs, to distinguish it from the pathological diabetic ketosis [18].3. The Physiology of Ketosis
After a few days of fasting or a drastically reduced carbohydrate diet (below 20 g per day), the body’s glucose reserves become insufficient for the production of oxaloacetate for normal fat oxidation in the Krebs cycle and for the supply of glucose to the central nervous system (CNS) [19–22]. Regarding the first issue, oxaloacetate is relatively unstable at body temperature, thus it is necessary (a minimal amount of oxaloacetate is required for an optimal functioning of the Krebs cycle) to supply the tricarboxylic acid cycle with oxaloacetate derived from glucose through ATP dependent carboxylation of pyruvic acid by pyruvate carboxylase [23].
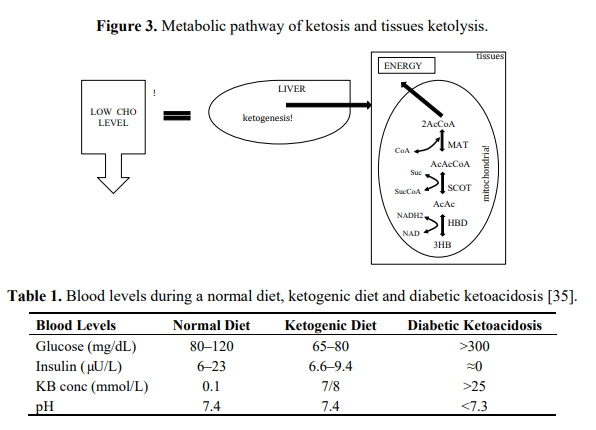
Regarding the second issue, the CNS cannot use fatty acids as an energy source (because they do not cross the blood-brain barrier), thus glucose is ordinarily the sole fuel for the human brain [24]. After 3–4 days of fasting or a very low carbohydrate diet the CNS needs an alternative energy source [19–22] and this is derived from the overproduction of acetyl-CoA which leads to the production of so-called ketone bodies (KB): acetoacetate (AcAc), β-hydroxybutyric acid (BHB) and acetone (Figures 1 and 2). This process is called ketogenesis and occurs principally in the mitochondrial matrix in the liver [25]. It is important to underline that the liver produces ketone bodies, but is unable to utilize them because the absence of the enzyme 3-ketoacyl CoA transferase required to convert acetoacetate into acetoacetyl-CoA.
After a few days of fasting or a drastically reduced carbohydrate diet (below 20 g per day), the body’s glucose reserves become insufficient for the production of oxaloacetate for normal fat oxidation in the Krebs cycle and for the supply of glucose to the central nervous system (CNS) [19–22].
[But the concetration of ketones in the blood rises to the point that the brain can use ketones for energy production – see below]
Even though the main ketone body produced in the liver is acetoacetate, the primary circulating ketone is β-hydroxybutyrate that is not, strictly speaking, a ketone body because the ketone moiety has been reduced to a hydroxyl group.
Under normal conditions the concentration of ketone bodies is very low (<0.3 mmol/L) compared to glucose (approx. 4 mmol) and, since glucose and ketone bodies have a similar Km (or Michaelis-Menten constant) for glucose transport to the brain, the ketone bodies begin to be utilised as an energy source by the CNS when they reach a concentration of about 4 mmol/L [27] which is close to the Km for the monocarboxylate transporter [28].
[And ketone bodies become an important energy source. With ongoing ketosis, glucose is still produced. Although serum blood glucose is reduced it remains within physiologic levels.]
In fact glucose is formed from two sources: glucogenic amino
acids and from glycerol liberated via lysis from triglycerides [32,33]. The importance of the second source increases progressively during the ketosis condition. In the first days of a ketogenic diet the main source of glucose is via neoglucogenesis from amino acids (AA), as the days goes by, the contribution of AA decreases whilst the amount of glucose derived from glycerol increases.As a matter of fact glycerol (released from triglyceride hydrolysis) can produce more than 16% of glucose in the liver during a KD and about 60% after a few days of complete fasting [32]. According to Bortz (1972) of the new glucose formed from protein and glycerol 38% is derived from glycerol in the
lean and 79% in the obese [34].During physiological ketosis ketonemia reaches maximum levels of 7/8 mmol/L with no change in pH while in uncontrolled diabetic ketoacidosis it can exceed 20 mmol/L with a concomitant lowering of blood pH [11] (Table 1). Blood levels of ketone bodies in healthy people do not exceed 8 mmol/L precisely because the central nervous system (CNS) efficiently uses these molecules for energy in place of glucose.
4. Do Ketogenic Diet Work?
The main questions that could be raised are:
(1) Do ketogenic diets works?
(2) Is there a yo-yo effect?
(3) Is a KD safe for obese subjects?There is no doubt that there is strong supportive evidence that the use of ketogenic diets in weight loss therapy is effective [13], however the mechanisms underlying the effects of KDs on weight loss is still a subject of debate.
5. Other Beneficial Effects in Obesity
[See the article]
6. Is There a Yo-Yo Effect?
While there are many studies which demonstrate that a ketogenic diet, at least in the short-term, results in greater weight loss than low-fat diets [13], from a long term perspective the success of a nutritional approach is defined by the amount of weight regain [64]. From this point of view, fewer data are available [41], in particular regarding so-called weight cycling or yo-yo effect [65,66]. [Successful weight loss maintenance is reasonably defined as] “individuals who have intentionally lost at least 10% of their body weight and kept it off at least one
year” [67]. . . . Recently Sumitharn and colleagues have
demonstrated that the increases in circulating ghrelin and in subjective appetite which accompanied a hypocaloric diet were reduced with a ketogenic approach [41]. Moreover we have very recently demonstrated that two brief periods of ketogenic diet separated by longer periods of maintenance of Mediterranean diet, led to successful long term weight loss and improvements in health risk factors without weight regain effect [Resource (2) below].7. It Is Safe for Obese Subjects?
[The ketogenic diet is not a high protein diet] because the state of the art KDs are normoproteic thus the daily amount of protein is
about 1.2–1.5 g of protein per Kg of body weight [44,78,79]. With regard to possible acidosis during VLCKD since the concentration of ketone bodies never rises above 8 mmol/L this risk is virtually non-existent in subjects with normal insulin function [80].8. Conclusions
A period of low carbohydrate ketogenic diet may help to control hunger and may improve fat oxidative metabolism and therefore reduce body weight. Furthermore new kinds of ketogenic diets using meals that mimic carbohydrate rich foods could improve the compliance to the diet [78]. Attention should be paid to patient’s renal function and to the transition phase from ketogenic diet to a normal diet that should be gradual and well controlled [69]. The duration of ketogenic diet may range
from a minimum (to induce the physiological ketosis) of 2–3 weeks to a maximum (following a general precautionary principle) of many months (6–12 months). Correctly understood the ketogenic diet can be a useful tool to treat obesity in the hands of the physician.
Resources:
(1) Ketogenic diet for obesity: friend or foe? [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Int J Environ Res Public Health. 2014 Feb 19;11(2):2092-107. doi: 10.3390/ijerph110202092.
(2) Long term successful weight loss with a combination biphasic ketogenic mediterranean diet and mediterranean diet maintenance protocol [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Nutrients 2013, 5, 5205–5217.