Jaundice (a yellow tint of the skin and whites of the eyes) in newborns is due to buildup of the chemical bilirubin in the blood and tissues. A low level of bilirubin in newborns is common in many newborns. However, if the blood level of the bilirubin becomes too high it can cause serious brain damage called kernicterus. It is to attempt to prevent this dangerous buildup that we doctors will monitor the bilirubin level with either a blood test or a skin test (the transcutaneous bilirubin monitor).
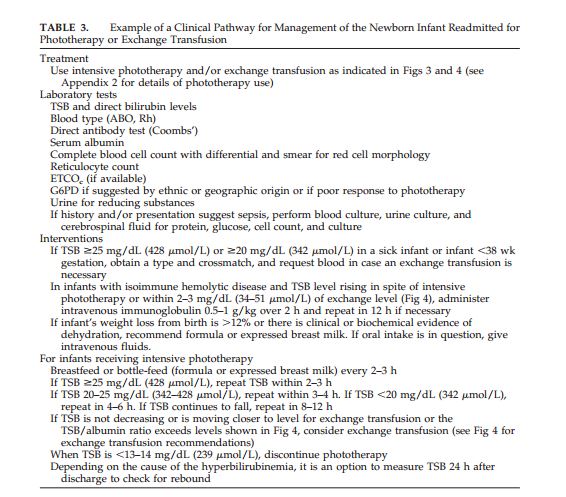
The American Academy of Pediatrics Guidelines Update for Neonatal Hyperbilirubinemia (1) in 2009 and the earlier 2004 Guidelines for Neonatal Hyperbilirubinemia (2) provide guidance on when and how to treat high bilirubin levels in newborns.
Reference 3 is the 2011 technical report guideline on providing phototherapy to prevent severe neonatal hyperbiliruninemia. And the article states that “The clinical impact of phototherapy should be evident within 4 to 6 hours of initiation with an anticipated decrease of more than 2 mg/dL in serum bilirubin concentration.”
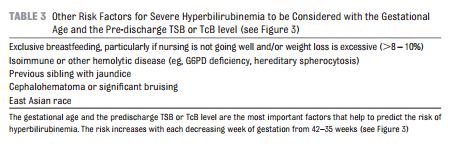
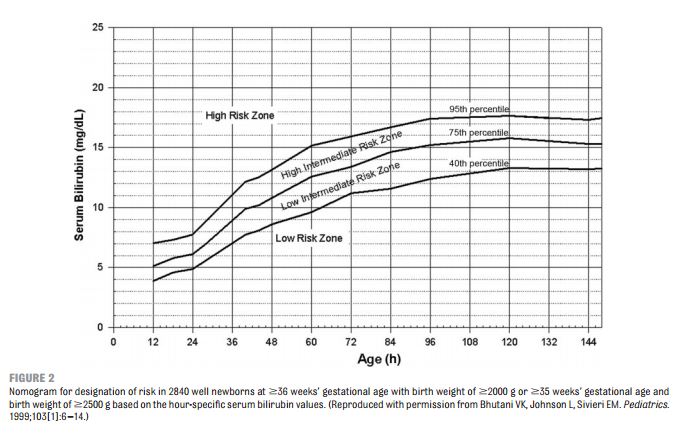
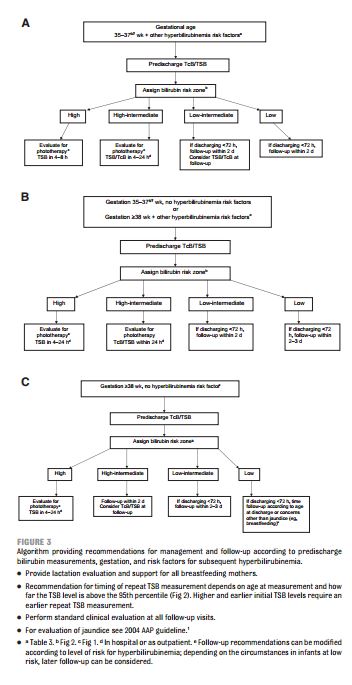
The figures and tables that follow are from the 2009 Update (1):
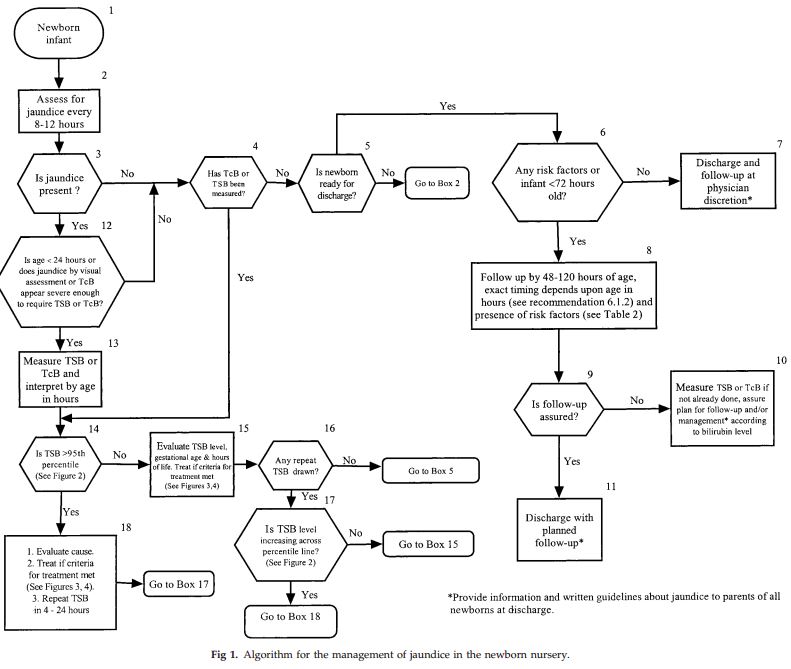
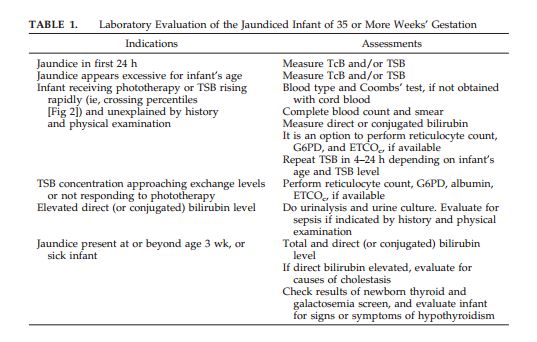
The following are from 2004 Guideline
The AAP Jaundice (hyperbilirubinemia) guideline has the following important points (2):
Measure the bilirubin level in any baby who appears jaundiced in the first twenty four hours. Don’t do visual estimate of jaundice—it leads to errors. Interpret the bilirubin level according to the infant’s age in hours. Infants less than 38 weeks gestation at birth and especially if they are breast fed are at high risk of dangerous levels of bilirubin. Perform a risk assessment (assess for risk factors that place the newborn at increased risk of dangerous levels after discharge). Make sure you provide a specific time for mother and to come back for retest of the bilirubin (based on the baby’s level at discharge and on the baby’s risk factors. Treat the newborn, when indicated by guideline and risk factors, with phototherapy or exchange transfusion.
Every baby needs a bilirubin level drawn prior to discharge and also needs a formal risk factor assessment.
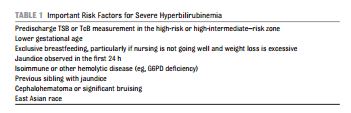
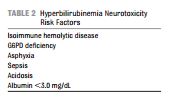
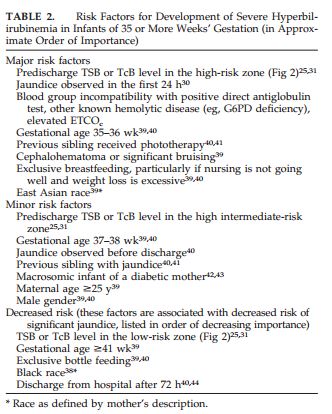
In the 2009 Guideline Update (3) the authors point out that there are two kinds of risk factors:
Important risk factors for hyperbilirubinemia–Predischarge TSB or TcB measurement in the high-risk or high-intermediate–risk zone; Lower gestational age; Exclusive breastfeeding, particularly if nursing is not going well and weight loss is excessive; Jaundice observed in the first 24 h; Isoimmune or other hemolytic disease (eg, G6PD deficiency) Previous sibling with jaundice; Cephalohematoma or significant bruising; East Asian race.
And risk factors that increase the risk of hyperbilirubinemia neurotoxicity [at a given bilirubin level]–Isoimmune hemolytic disease; G6PD deficiency; Asphyxia; Sepsis; Acidosis; Albumin < 3.0 mg/d.
The authors point out that even with a low predischarge bilirubin level, the risk of serious hyperbilirubinemia is not zero. That is why all newborns discharged at less than 72 hours need to be seen within 2 days of discharge.
Hemolysis (increased destruction of red blood cells) increases the risk of neurotoxicity and is likely “if the [bilirubin level] is crossing percentiles on the nomogram and suggests the need for further testing and follow-up (see Table 1 in the 2004 AAP guideline.” (4)
Finally, reference 1 is a great article on the technical aspects of providing phototherapy. And the article states that “The clinical impact of phototherapy should be evident within 4 to 6 hours of initiation with an anticipated decrease of more than 2 mg/dL in
serum bilirubin concentration.”
(1) Hyperbilirubinemia in the Newborn Infant 35 Weeks’ Gestation: An Update With Clarifications. American Academy of Pediatrics. Pediatrics 2009;124;1193.
(2) Management of Hyperbilirubinemia in the Newborn Infant 35 or More Weeks of Gestation. American Academy of Pediatrics. Pediatrics 2004;114;297 .
(3) Phototherapy to Prevent Severe Neonatal Hyperbilirubinemia in the Newborn Infant 35 or More Weeks of Gestation. American Academy of Pediatrics. 2011 available at
https://aappolicy.aappublications.org/cgi/reprint/pediatrics;128/4/e1046.pdf.
(4) BiliTool—A quality improvement tool for newborn bilirubin management available at https://bilitool.org/.
(6) BiliTool Page 2—A useful listing of AAP resources with links to the guideline and directly to relevant parts of the guideline including an hour specific nomogram, risk factors for the development of severe hyperbilirubinemia, and an hour specific nomogram of when to begin phototherapy available at
https://bilitool.org/?page_id=2.