In this post I link to and excerpt from Emergency Medicine Cases‘ Episode 101 GI Bleed Emergencies Part 1. Helman, A, Swaminathan, A, Rezaie, S, Callum, J. GI Bleed Emergencies Part 1. Emergency Medicine Cases. October, 2017. Accessed 6-12-2020.
Note to myself: I made this post just to remind me of the excellent EMC GI Bleed post. Be sure and reread the entire show notes as my excerpts are very abreviated.
Here are excerpts:
How to distinguish LGIB from UGIB
Distinguishing LGIB from UBIB is not always obvious clinically.
STEP 1: Is the patient hemodynamically unstable?
As a general rule, if a patient is hemodynamically unstable, assume UGIB because UGIB is more prevalent and is associated with a higher mortality.
STEP 2: Is there bright red blood per rectum (BRBPR) with clots or hematemesis?
BRBPR with clots can be considered almost pathognomonic for a LGIB while hematemesis can be for an UGIB source.
Note that LGIB can manifest as melena [black tarry stool] and conversely, brisk upper GI bleed can manifest as hematochezia [the passage of fresh blood per anus, usually in or with stools} (without clots) in about 15% of cases. Melena on history was found to have an 80% sensitivity for UGIB with a +LR = 5.9 in a large systematic review in JAMA 2012 [1].
STEP 3: Calculate the BUN: Creatinine Ratio and consider the patient’s age.
The same JAMA systematic review found that a BUN:Cr ratio >30 is 93% specific for UGIB, with a +LR = 7.5. Note the units are mg/dL as used in the U.S. For other countries first divide the Creatinine by 88.42 (or roughly 100) before calculating the ratio.
Age less than 50 years has a specificity of 92% and +LR = 2.5 for UGIB source.
A study examining ED predictors of UGIB without hematemesis in 2006 found that 3 factors independently predict an UGIB source [2]:
- Melena
- BUN:creatinine ratio >30
- Age < 50 years
Value of FOBT for detecting lower GI bleed emergencies
In a large population based study of asymptomatic adults out of Taiwan in 2011 the sensitivity of fecal occult blood testing for predicting a LGIB source of bleeding was only 24.3%, the specificity 89.0%, the +LR = 2.22, the -LR = 0.85 and the accuracy 73.4%. While these were not ED patients with suspected GI bleed, the results give us a general idea of the limitations of FOBT [3].
Airway Pearls & Pitfalls in GI bleed emergencies – See Show Notes For Details.
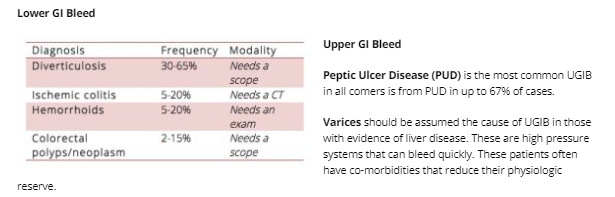
Differential diagnosis of GI bleed emergencies
Aorto-enteric fistulae cause rapid and severe bleeding that is rarely indolent. Look for surgical scars. These patients die quickly.
Initial fluid management in massive GI bleed emergencies
Avoid excessive crystalloid resuscitation. While there is no literature to guide us specifically in this patient population a general rule of thumb is that hemodynamically unstable bleeding patients need blood products. Practically speaking, there are often delays in obtaining blood products, so our experts recommend giving a minimum amount of fluid to maintain MAP > 60 mm Hg.
Transfusion management in GI bleed emergencies
General principles of transfusion management in GI bleed emergencies
Hemodynamic instability: Transfuse regardless of hemoglobin level
Shock index: A shock index (HR/SBP) of >1 should trigger consideration for massive transfusion
Don’t trust the Hb: Hemoglobin often lags behind bleeding, so trend it by repeating the hemoglobin in an hour or two.
Consider clinical factors: Presyncopal patient, high volume blood loss or brisk bleeding should trigger consideration for red cell transfusion.
Be flexible: Lower your threshold to transfuse in patients with co-morbidities such as coronary artery disease or coagulopathy.
Most GI bleed patients can tolerate low hemoglobins: Stable patients with a chronic GI bleed of small volume can generally tolerate low hemoglobins.
Portal bleeding: Restitution of blood volume may be associated with recurrence of portal bleeding.
While there is no specific literature for hemoglobin transfusion thresholds for LGIB a landmark study out of NEJM in 2013 in patients with stable UGIB suggested that a hemoglobin threshold of 7 for red cell transfusion [6].
Stable UGIB patients in the liberal transfusion arm (Hb<9) had increased bleeding, higher mortality, increased need for surgery and increased length of stay when compared to the restricted transfusion group (Hb<7). Note that this study was conducted in a highly controlled environment with rapid access to endoscopy and therefore, may not be applicable to resource limited settings.
There is much more to review in the excellent show notes. I placed this post just to remind me of the great resource.