In this post I link to and excerpt from POCUS Cases 1: Pulmonary Embolism and Right Heart Strain [Link is to the video] from POCUS Cases Videos from Emergency Medicine Cases:
Here are excerpts [Comments in brackets are my thoughts]:
Summary And Pearls
- Wheezes do not always mean Asthma/COPD
- Approximately 10% of acute PEs present with wheezing.
- POCUS can help you narrow your differential diagnosis in shortness of breath.
- POCUS can help distinguish acute PE from chronic conditions of RV strain.
- RVOT excursion on POCUS is a specific sign of PE.
Case
63 yo female with a PMH of breast cancer treated with chemotherapy with her last chemo was one month ago and a history of COPD for which she takes two inhalers.
Her chief complaint is shortness of breath.
Vital Signs
Temperature is 36.8 Heart Rate is 120. Respiratory rate is 23. Oxgen saturation was low at 84% on room air, but at 6 liters she is at 94%. Blood pressure is 120/89.
History and Physical
She has shortness of breath that has been severe over the last few days. It occurs with limited excertion and at rest. There has been no cough at any time, no chest pain, no fevers, and no leg swelling.
She has had little to no relief with her puffers.
On physical exam she has normal heart sounds with no murmur. Wheezes bilaterally. Her abdoman is soft and non tender. There is no leg edema or calf tenderness.
The wheezes bilaterally stand out. That might help to determine the diagnosis.
Working Through The Case
My resident indicated that this was probably an exacerbation of COPD which he wants to treat with back to back salbutomol atrovent and masks as well as steroids.
The resident indicates that Pulmonary Embolus is a Can’t Miss Diagnosis that he would want to rule out in this case.
What Are Our Options In This Case
- We can treat as a COPD exacerbation and gauge the outcome.
- We can perform a chest x-ray to see if there is an alternative diagnosis in this case.
- We can obtain a D-dimer to see if it is elevated to pull the trigger to get a CT scan.
- Or we can use our Point-of-Care Ultrasound to distinguish the two diagnoses.
- [We should also check an ECG, basic labs, and troponin, it seems to me.]
We elected to start with POCUS [and the rest of the video goes through the ultrasound findings of PE]
Fig 2 Text
Fig 3 Text
Fig 4 Text
Fig 5 Text
Fig 6 Text
Fig 7 Text
So Don’t All of the Above Confirm Pulmonary Embolus – The Right Ventricle Is Bigger Than The Left Ventricle.
No, not in this case. This case is a little more complicated because of the patient’s comorbidities.
If I was presented a case of a 20 year old who was previously healthy who has PE risk factors such as just started an oral contraceptive pill and comes in tachycardic with pleuritic chest pain. And you get these images, then it is a slam dunk – it is obviously a PE in this case.
But our case is a little more complicated.
What we have shown in these videos is that this patient has right ventricular heart strain.
RV Strain Differential Diagnosis
- Pulmonary hypertension
- Mitral stenosis
- Pulmonary embolism
- Chronic lung diseases causing Cor Pulmonale
- Congenital heart disease, e.g.
- Tetralogy of Fallot
- pulmonary stenosis
- Arrythmogenic Right Ventricular Dysplasia (ARVD)*
- * Link is to the ARVD information page from The Genetics Home Reference of The National Library of Medicine.
- *The above link is an excellent resource for both clinicians and patients.
- Clinical Diagnosis, Imaging, and Genetics of Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia: JACC State-of-the-Art Review [PubMed Abstract] [Full Text HTML] [Full Text PDF]. J Am Coll Cardiol. 2018 Aug 14;72(7):784-804
Common Findings Of Pulmonary Embolus On Bedside Ultrasound
- The RV to LV Ratio
- Is your right ventricle dilated compared to the left ventricle?
- If yes, that could be a point to PE
- Is there a D sign present?
- Is there a [decreased] TAPSE (Tricuspid Annular Plane Systolic Excursion)?*
- *Tricuspid annular plane systolic excursion (TAPSE) predicts poor outcome in patients undergoing acute pulmonary embolectomy [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Heart Lung Vessel. 2015; 7(2): 151–158.
- Is there a McConnell sign?
- [The McConnell’s sign [Link is to Radiopedia] describes a regional pattern of acute right ventriculardysfunction on transthoracic echocardiography first observed in a cohort of patients with acute pulmonary thromboembolism. In contrast to the global wall motion abnormalities observed in chronic right ventricular dysfunction, this sign refers to the coexistence of akinesia of the mid-free right ventricular wall with preserved apical contractility 1.
Subsequent studies have demonstrated a consistently low sensitivity; in the presence of high pretest probability, it may serve as a useful rule-in parameter at the bedside 2,3.
Even though we think of all of the above as findings in Pulmonary Embolus, they are all also found in Pulmonary Hypertension.
Let’s go through [videos of] each of the signs and what they look like on ultrasound.
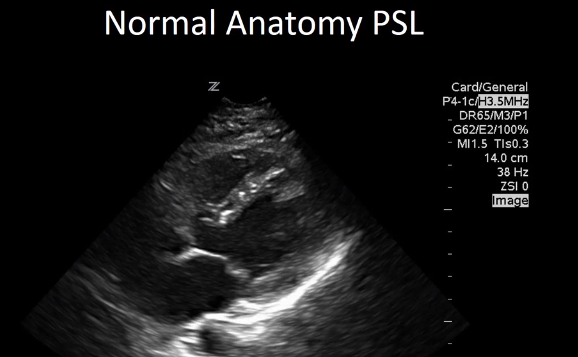
First let’s talk of RV to LV ratio.
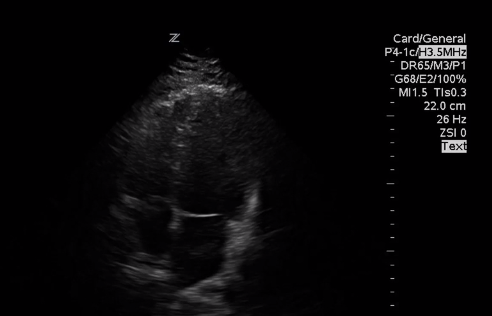
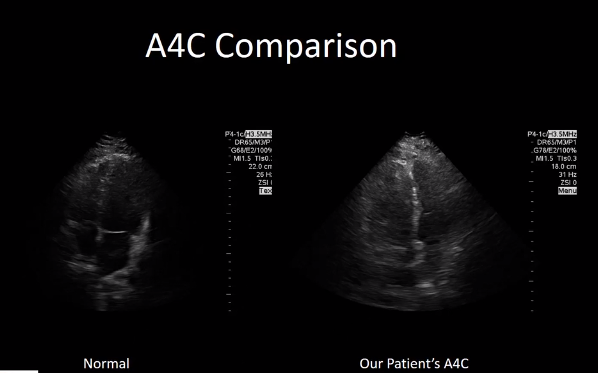
Here is a view of the Apical 4 chamber
Here is a video of our patient [from 7:05 – 7:38]. As we’ve shown when we looked at the normal anatomy, [normally the RV is 2/3rds the size of the LV. In this case the RV is clearly enlarged compared to the LV].
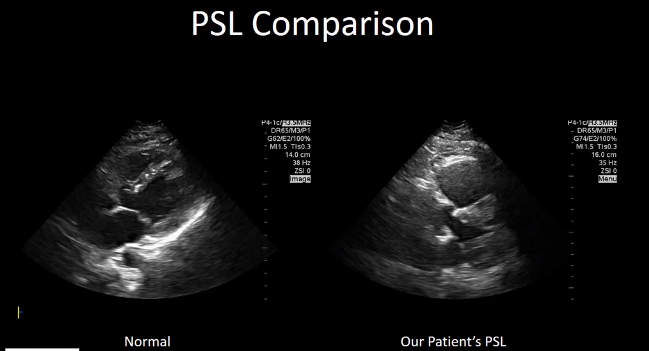
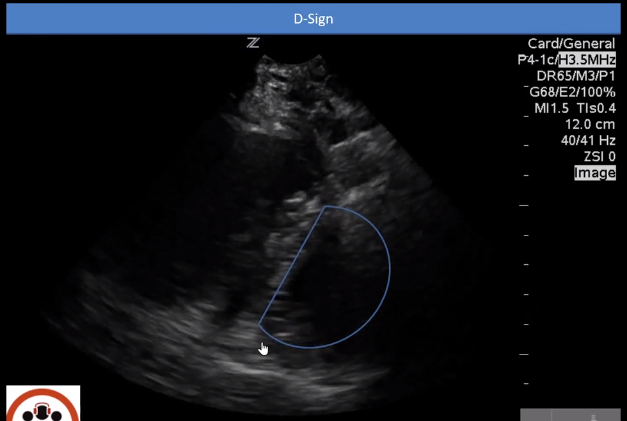
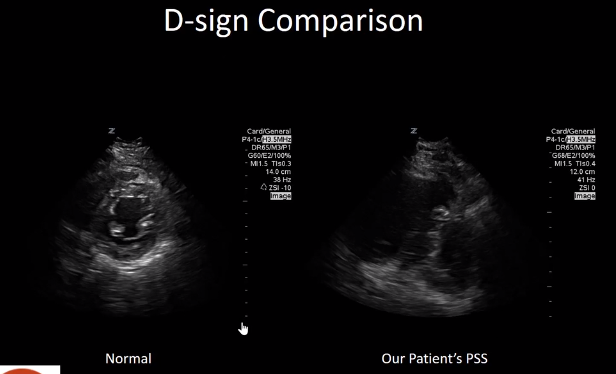
Here is a view of the Parasternal Short Axis
This video [from 7:38 – 8:16] is showing what D-sign looks like. The D-sign occurs when the right ventricle has such high pressures that it pushes the interventricular septum into the left ventricle. The left ventricle instead of being that circular donut, looks like the letter D.
And here is a comparison of a normal left ventricle on a parasternal short axis where it is nice and circular getting bigger and smaller.
And here’s our patient’s parasternal short view. As you can see, the letter D is being made when the heart beats.
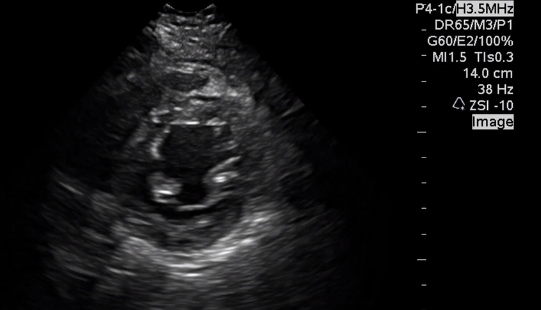
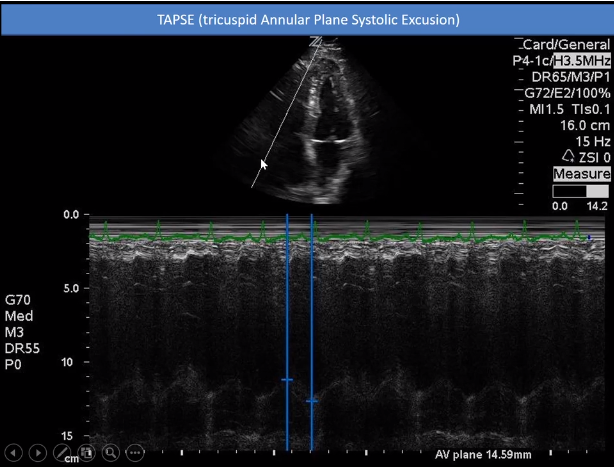
Next We’ll Talk about TAPSE (Tricuspid Annular Plane Systolic Excursion)
TAPSE [8:19 – 9:35] is another measurement that can help you in determining one of the findings for acute PE. The way to do it is to use M-mode. As we can see as time goes by you can detect the movements of the object that the [M-mode] line is on.
In this case we have the line over the lateral annulus. By doing so we can measure its motion and see that the lateral annulus is moving up and down.
For TAPSE we can measure the systolic excursion. And in this case, when we measure it, we are getting a value of 14.59 mm.
Now I find that everyone I ask has a different value for TAPSE. Some people use 18 mm. And some people use very specific numbers like 20.1 mm.
Regardless, our number of 14.59 mm is less than both of these numbers. This informs us that there is definitely some dysfunction of the right ventricle and points us in the direction that this might be a PE.
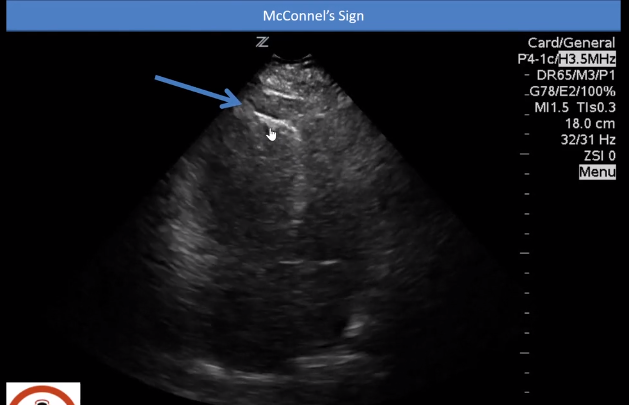
McConnell’s Sign
McConnell’s sign [9:36 – 10:10] is one of the more specific signs that points to PE [although it is not sensitive].
McConnell’s sign is when there is limited movement of the free wall of the right ventricle but there is apical sparing.
[Apical sparing means] that the apex is going to look like it is moving quite a bit compared to the rest of the right ventricle.
When I play this video, you’ll see that the right ventricle barely moves. But if you look where the apex is – the apex looks like it is bouncing up and down compared to how much the rest of the ventricle is moving.
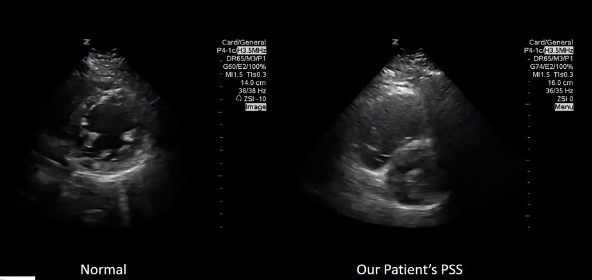
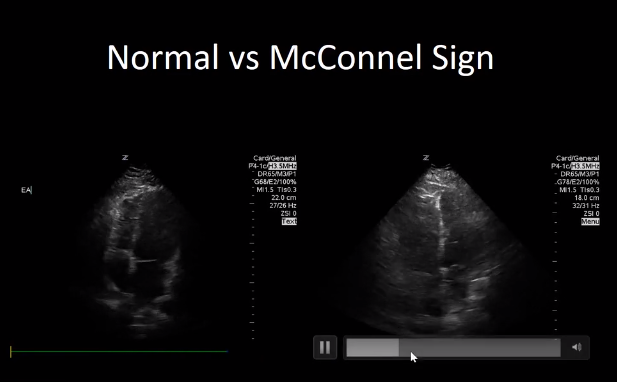
Normal versus McConnell’s Sign
Let’s compare that side by side with normal and with our patient’s [McConnell’s sign] [10:13 – 10:41]
When we look at the normal [on the left side] we see the entire right ventricular wall is moving symmetrically. Each part of the wall moves in and out about the same amount.
In our patient [on the right side] it appears that the apex is moving up and down a lot more than the right ventricle free wall. In fact the right ventricle free wall is barely moving in and out at all but the apex is moving up and down.
This is a positive McConnell’s sign in this case.
Right Ventricular Systolic Excursion: A Distinguishing Echocardiographic Finding in Acute Pulmonary Embolism [PubMed Abstract]. Echocardiography. 2013 Jul;30(6):649-57.
This study tried to look for very specific findings that you can use for acute PE. And what it showed was that although positive McConnell’s sign was seen quite frequently in acute PE (60%), it was also seen in some cases of chronic pulmonary hypertension (∼ 15%).
So although a very useful sign to determine if PE is present, McConnell’s sign is not perfect.
In fact, when this study looked at all of the features in terms of which are most specific for PE, it found that right ventricular outflow tract systolic excursion was one of the most specific findings.
In fact, when present, it most likely points towards PE.
And if you plug your values into this complicated looking formula, you can actually measure right ventricular systolic excursion.
And although this formula looks quite complicated, it is not actually complicated at all.
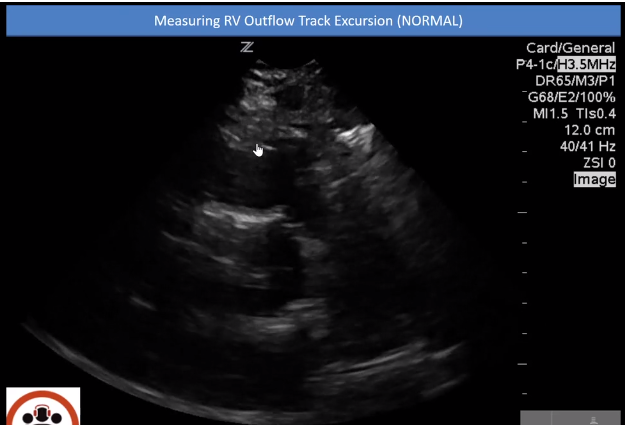
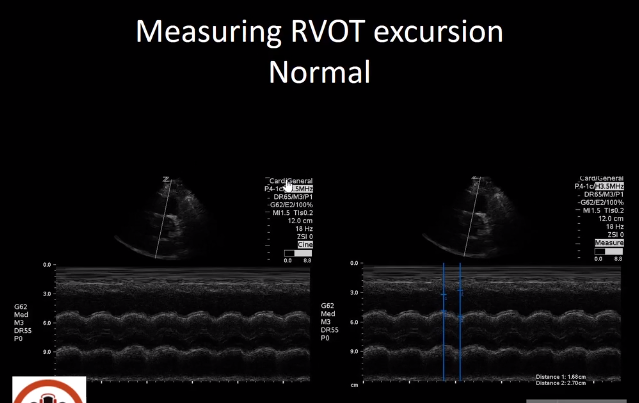
Lets look at how to Measure RVOT Systolic Excursion [11:38 – 13:10]
In this normal video of normal we are in the parasternal short axis at the level of the aortic valve.
Point your eyes to this here [where the little hand is] which is the free wall of the right ventricle.
And as it contracts it [the free wall] gets closer to the valve [where the little hand is now].
We can measure this distance between the valve [and the free wall] by measuring the distance with M-mode. We measure the distance between where the right ventricular free wall and the aortic valve when they are closest together and farthest apart.
If you plug them into the formula:
RVOT Excursion: [(2.70 – 1.68)/2.70] x 100 = 37.8%
In the article, it showed that if you have chronic severe pulmonary hypertension, the values they were receiving on average were 31%.
However, if you had acute pulmonary embolism, the number was quite a bit lower, closer to 17%.
In our case, where the patient had an acute pulmonary embolism, the excursion was quit low, indicating in this case that it was a PE.
Resolution of the Case
So based on these POCUS findings, puffers and steroids were not started. The patient was expedited for CT scan to confirm a PE. Heparin was started. And a discussion of goals of care with the patient was had. And lytics were at the bedside in case the patient was to have a cardiac arrest.
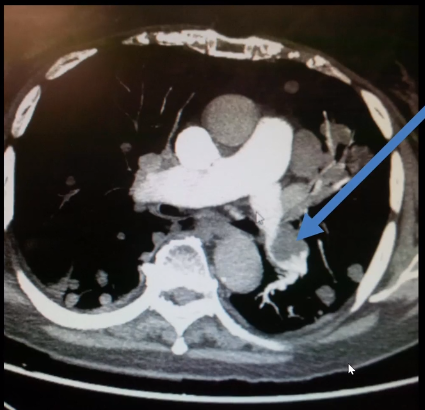
So what happened when we took this patient to the CT scanner?
Well, unfortunately she was diagnosed with a large blood clot and right ventricular heart strain was seen.
Summary And Pearls
- Wheezes do not always mean Asthma/COPD
- Approximately 10% of acute PEs present with wheezing.
- POCUS can help you narrow your differential diagnosis in shortness of breath.
- POCUS can help distinguish acute PE from chronic conditions of RV strain.
- RVOT excursion on POCUS is a specific sign of PE.
Findings such as McConnell’s sign, D sign, TAPSE are all quite good. However, they are not as specific as Right Ventricular Outflow Tract Excursion on POCUS.
Right Ventricular Outflow Tract Excursion on POCUS is a very specific that the patient has an acute pulmonary embolus.
Finally, A Caution
A normal POCUS does not mean that there is no PE. POCUS can only detect pulmonary embolisms that cause right ventricular strain.
Many patients can have PE that have no right ventricular strain.
Only massive and submassive PE tend to have right ventricular strain.
Thus POCUS is specific for PE but POCUS has a very poor sensitivity for PE.
So just remember that you can have a completely normal cardiac ultrasound and the patient can have a PE.
The ones we’re more worried about in the emergency department, however, are the ones that have right ventricular heart strain that can cause the patient to have a cardiac arrest.
These ones are generally picked up on ultrasound as we can see the changes in the heart caused by the pulmonary embolism.