Here are links to additional resources on heart failure.
- treatment of acute and chronic heart failure ESC Clinical Practice Guidelines
25 Aug 2023 - 2023 ACC Expert Consensus Decision Pathway on Management of Heart Failure With Preserved Ejection Fraction: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2023 May, 81 (18) 1835–1878
- 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Originally published1 Apr 2022 https://doi.org/10.1161/CIR.0000000000001063Circulation. 2022;145:e895–e1032 [PubMed Abstract] [Full-TextHTML] [Full-Text PDF].
- 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e876-e894. doi: 10.1161/CIR.0000000000001062. Epub 2022 Apr 1. [PubMed Abstract] [Full-Text HTML] [Full-Text PDF].
Today, I review, link to, and excerpt from Up-titrating heart failure medicines: A practical guide from NPS MedicineWise. Accessed 2/12/2024.
All that follows is from the above resource.
Key points
- People with HFrEF should be prescribed a combination of an ACE inhibitor (or ARB if not tolerated), a heart failure beta blocker and an MRA, up-titrated to target or maximum tolerated doses, to help improve quality of life, reduce hospitalisations and save lives.
- GPs play a vital role in starting and optimising doses of guideline medicines for patients with HFrEF.
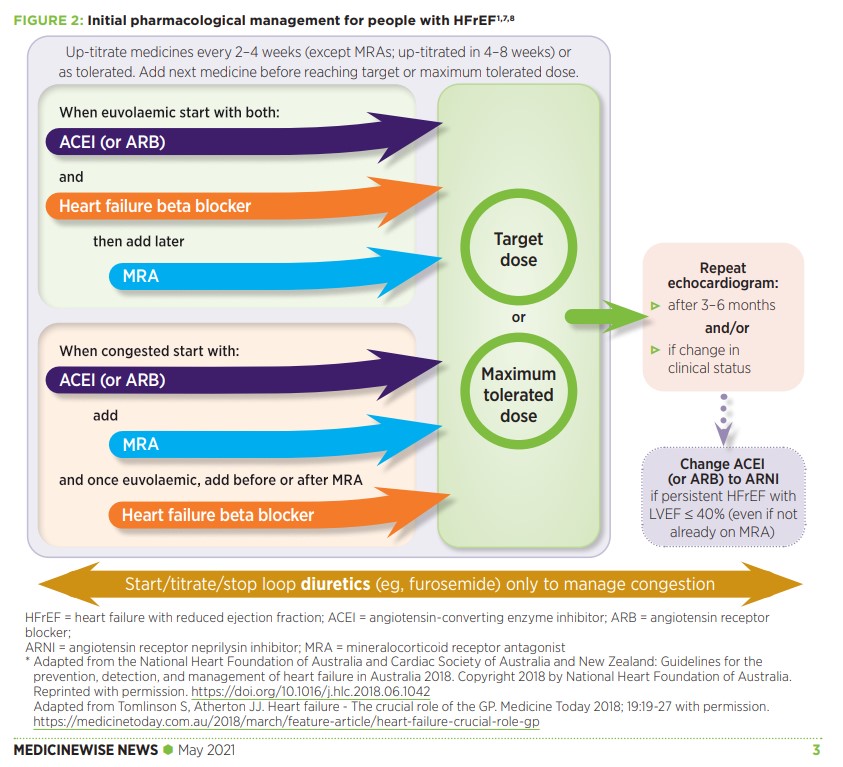
- Up-titration guidance includes: start heart failure medicines at low doses, double the dose one medicine at a time every 2–4 weeks (except MRAs, up-titrated in 4–8 weeks) and add the next medicine before reaching target or maximum tolerated dose of the previous medicine.
- Monitor patients closely with a review 1–2 weeks after each medicine initiation and dose increase, and make variations to up-titration when required in response to adverse effects.
- Asymptomatic or mild changes in blood pressure, heart rate or renal function during up-titration do not usually require dose reduction.
A practical guide for up-titrating heart failure medicines
Australian heart failure guidelines are clear on the goal of pharmacological management for people who have heart failure with reduced ejection fraction (HFrEF).
That goal is to prescribe a combination of:1
- an angiotensin-converting enzyme (ACE) inhibitor, or if not tolerated, angiotensin receptor blocker (ARB) and
- a heart failure beta blocker and
- a mineralocorticoid receptor antagonist (MRA)
all at target or maximum tolerated doses.
The guidelines, developed by the National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand, also describe how to up-titrate these three medicines to reach the target or maximum tolerated doses.1
However GPs can find it challenging to put up-titration into practice.2,3
This article provides a practical guide to assist GPs with the up-titration of heart failure medicines for people with HFrEF.
Evidence for a combination of heart failure medicines
The recommendation to prescribe a combination of an ACE inhibitor (or ARB if not tolerated), a heart failure beta blocker and an MRA at target or maximum tolerated doses is based on evidence that these medicines together can help improve quality of life, reduce hospitalisations and save lives for people with HFrEF.1,4
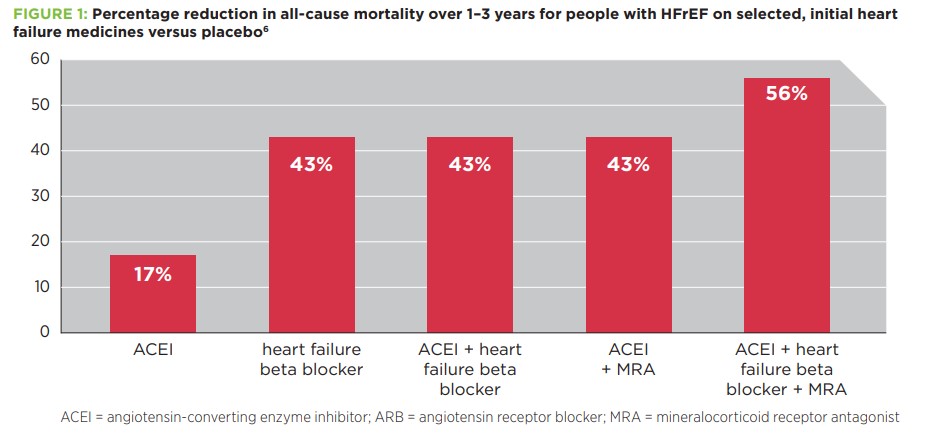
A 2017 meta-analysis found that people with HFrEF who were prescribed a combination of ACE inhibitor, heart failure beta blocker and MRA at target doses had a 56% reduction in all-cause mortality over 1–3 years, compared to placebo. This combination was much more effective than an ACE inhibitor or heart failure beta blocker alone, or a combination of two out of three medicines.6 See Figure 1.
Up-titration guidance
The process of up-titration recommended by Australian guidelines to reach the goal of a combination of heart failure medicines is to:1,4
- start each medicine at a low dose and
- gradually up-titrate them to target or maximum tolerated doses.
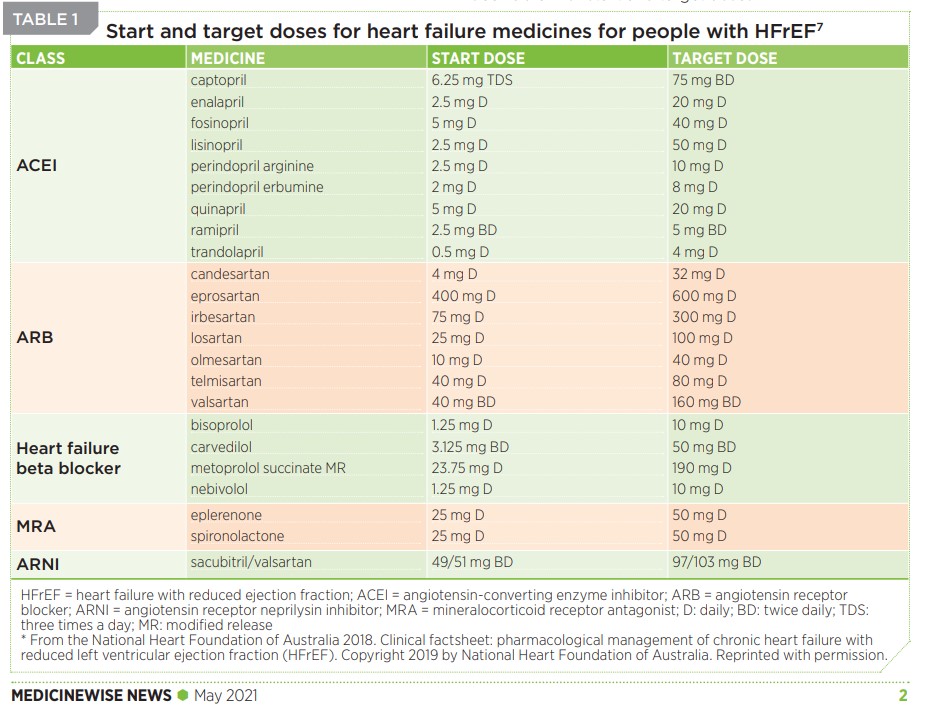
See Table 1 for start and target doses.
Table 1: Start and target doses for heart failure medicines for people with HFrEF7
* From the National Heart Foundation of Australia 2018. Clinical factsheet: pharmacological management of chronic heart failure with reduced left ventricular ejection fraction (HFrEF). Copyright 2019 by National Heart Foundation of Australia. Reprinted with permission.
However rather than a single up-titration pathway to reach this goal, there are two pathways that are differentiated by the patient’s volume status when starting pharmacological management; euvolaemic or congested.1 See Figure 2.
- 2023 Focused Update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure ESC Clinical Practice Guidelines
25 Aug 2023 - 2023 ACC Expert Consensus Decision Pathway on Management of Heart Failure With Preserved Ejection Fraction: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2023 May, 81 (18) 1835–1878
- 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Originally published1 Apr 2022 https://doi.org/10.1161/CIR.0000000000001063Circulation. 2022;145:e895–e1032 [PubMed Abstract] [Full-TextHTML] [Full-Text PDF].
- 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e876-e894. doi: 10.1161/CIR.0000000000001062. Epub 2022 Apr 1. [PubMed Abstract] [Full-Text HTML] [Full-Text PDF].