Today, I review, link to, and excerpt from Critical care ultrasound in cardiac arrest. Technological requirements for performing the SESAME-protocol–a holistic approach [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Daniel Lichtenstein, Manu L N G Malbrain. Anaesthesiol Intensive Ther. 2015;47(5):471-81. doi: 10.5603/AIT.a2015.0072. Epub 2015 Nov 18.
There are 117 similar articles in PubMed.
The above article has been cited by 18 articles in PubMed.
All that follows is from the above resource.
Abstract
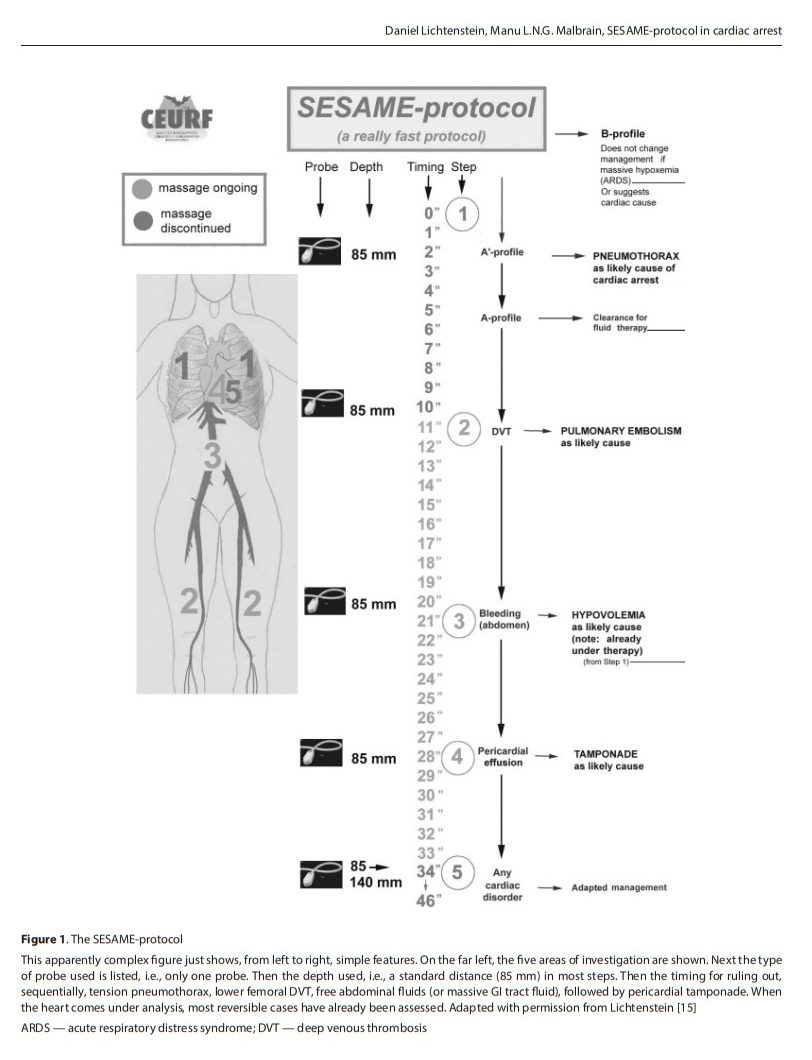
The use of ultrasound has gained its place in critical care as part of our day-to-day monitoring tools. A better understanding of ultrasound techniques and recent publications including protocols for the lungs, the abdomen and the blood vessels has introduced ultrasound to the bedside of our ICU patients. However, we will prove in this paper that early machines, dating back more than 25 years, were perfectly able to do the job as compared to modern laptop machines with more features but few additional advantages. Ultrasound is not only a diagnostic tool, but should also be seen as an extension of the traditional physical examination. This paper will focus on the use of the SESAME-protocol in cardiac arrest. The SESAME-protocol suggests starting with a lung scan to rule out possible causes leading to cardiac arrest. Firstly, pneumothorax needs to be ruled out. Secondly, a partial diagnosis of pulmonary embolism is done following the BLUE-protocol. Thirdly, fluid therapy can be guided, following the FALLS-protocol. The SESAME-protocol continues by scanning the lower femoral veins to check for signs of deep venous thrombosis, followed by (or before, in case of trauma) the abdomen to detect massive bleeding. Next comes the pericardium, to exclude pericardial tamponade. Finally, a transthoracic cardiac ultrasound is performed to check for other (cardiac) causes leading to cardiac arrest. The emphasis is on a holistic approach, where ultrasound can be seen as the modern stethoscope needed by clinicians to complete the full physiological examination of their critically ill unstable patients.
Keywords: SESAME-protocol; cardiac arrest; ultrasound.
This paper will deal with the most “critical” application of critical care ultrasound, namely patients in cardiac arrest. . . . Although there is no time at all for any traditional test (X-rays, CT scan, laboratory evaluation etc.), ultrasound is readily available [9]. Thus, to expedite the diagnosis of reversible causes
of cardiac arrest, (shockable rhythms excluded), is the full
domain of critical care ultrasound [2, 10].The emphasis is on a holistic approach, where ultrasound can be seen as the modern stethoscope needed by clinicians to complete the full physiological examination of their critically ill unstable patients.
THE ROLE OF ULTRASOUND IN CARDIAC ARREST
The SESAME-protocol is an abbreviation of the mnemotechnic SESAMOOSSIC, which stands for “Sequential
Echographic Scanning Assessing Mechanism Or Origin of
Severe Shock of Indistinct Cause”. This indicates that the
clinician following this protocol takes into account both the
mechanism and cause, according to which comes first in
the sequential SESAME screening.IDEAL ULTRASOUND EQUIPMENT SPECIFICATIONS
We will now explain the philosophy of the SESAMEprotocol in 5 simple steps that can be used when one is confronted with a cardiac arrest patient.
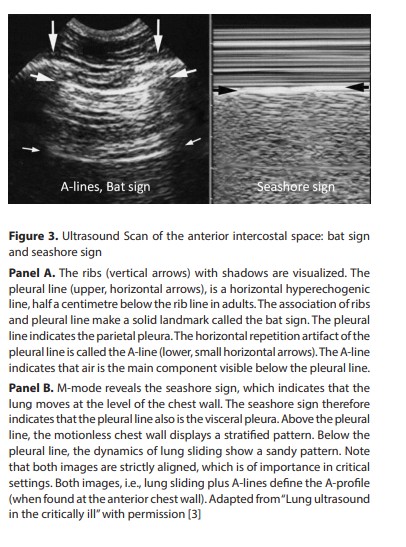
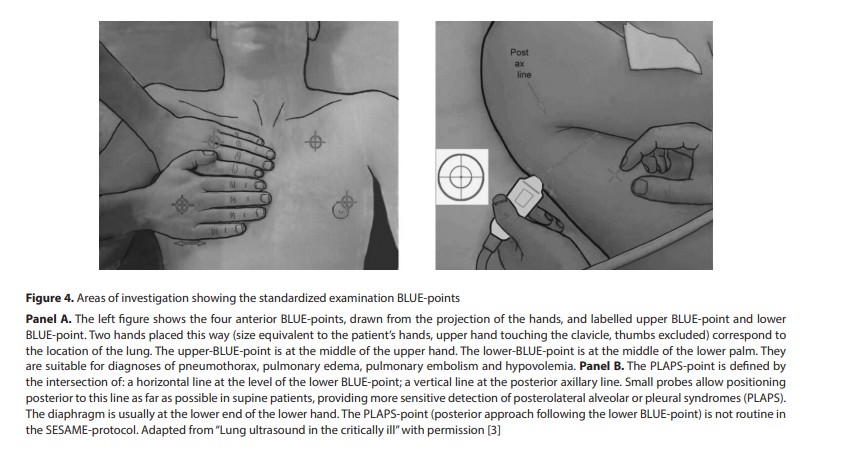
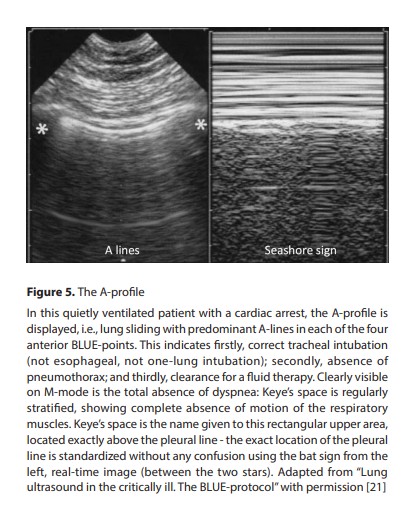
STEP 1. RULING OUT PNEUMOTHORAX: LUNG ULTRASOUND
The SESAME-protocol is a sequential protocol which
first scans the lungs, mainly for ruling out pneumothorax
[4, 11−13].. Thirdly, as pneumothorax with cardiac arrest
is usually large that it can be detected regardless of where
the probe is applied on the anterior thorax (Fig. 4).Fourthly, as only less than two seconds are needed for detecting
the characteristics of lung sliding and/or B-lines [4]. Fifthly, because the diagnosis is particularly easy as the patient is
in quiet breathing via manual bag ventilation, i.e., enough
dynamics and no interference due to dyspnea, i.e., the best conditions.Finally, because the detection of the A-profile (as illustrated in Figure 5) with the BLUE-protocol will be an argument for fluid therapy, if one subsequently follows the logic of the FALLS-protocol [4, 5].