In addition to today’s resource, consider:
- Bronchiolitis in children: diagnosis and management
[HTML Version] [PDF Version]NICE Guideline, No. 9. London: National Institute for Health and Care Excellence (NICE); 2021 Aug 9.
ISBN-13: 978-1-4731-1162-2 - Patient Safety Alert: Risk of harm from inappropriate placement of
pulse oximeter probes. 18 December 2018 - Bronchiolitis: A Scenario-Based Primer from The Children’s Hospital Of Philadelphia [accessed 11-26-2023]
- Emergency Department Clinical Pathway for Evaluation/Treatment of Children with Bronchiolitis from The Children’s Hospital Of Philadelphia [accessed 11-26-2023]
- Inpatient Clinical Pathway for Evaluation/Treatment of Children with Bronchiolitis from The Children’s Hospital Of Philadelphia [accessed 11-26-2023]
- Emergency Department and Inpatient Clinical Pathway for Oral or Enteral Feeding in Children with Bronchiolitis from The Children’s Hospital Of Philadelphia [accessed 11-26-2023]
- Additional Treatment Considerations [in Bronchiolitis]May be considered in infants with significant respiratory distress that is not alleviated sufficiently by supportive care interventions from The Children’s Hospital Of Philadelphia [accessed 11-26-2023]
- Something Is Changing in Viral Infant Bronchiolitis Approach. MINI REVIEW article. Front. Pediatr., 14 April 2022. Sec. Pediatric Pulmonology
Volume 10 – 2022 | https://doi.org/10.3389/fped.2022.865977 - Dr Mellick’s YouTube Video “Treating Bronchiolitis in the Outpatient Setting”-The 2014 AAP Bronchiolitis Guidelines Are Wrong
Posted on May 25, 2022 by Tom Wade MD
Dr. Alverson, in the podcast below, recommends that parents use the Frida Baby NoseFrida Nasal Aspirator* for nasal suctioning of the infant with bronchiolitis.
This link to the Target website is not an affiliate link.
For me, the big key for admission, besides the determination of sick or not sick*, is the infant dehydrated or becoming dehydrated.
*When seeing a pediatric patient, the doctor is first trying to decide: sick (worrisome-meaning potentially in immediate danger.) or not sick (meaning not worrisome-not in immediate danger).
Today, I reviewed and linked to the Cribsiders’ #2:Go with the High Flow: Bronchiolitis with Dr. Brian Alverson*.
* Link is to the Cribsiders’ website show notes.
Alverson B, Kelly J, Chui C, Berk J. “Go with the High Flow: Bronchiolitis with Dr. Brian Alverson”. The Cribsiders Pediatric Podcast. https://thecurbisiders.com/thecribsiders/2.
Note to myself: I could not get the podcast to play on The Cribsider’s website. I just used that for the show notes.
Go to The Cribsiders’ Apple Podcasts‘* #2: Go with the High Flow: Bronchiolitis with Dr. Brian Alverson and play the podcast there.
*This link is to a list of all of The Cribsiders podcasts that you can listen to on Apple podcasts.
All that follows is from the show notes of the above resources.
Summary
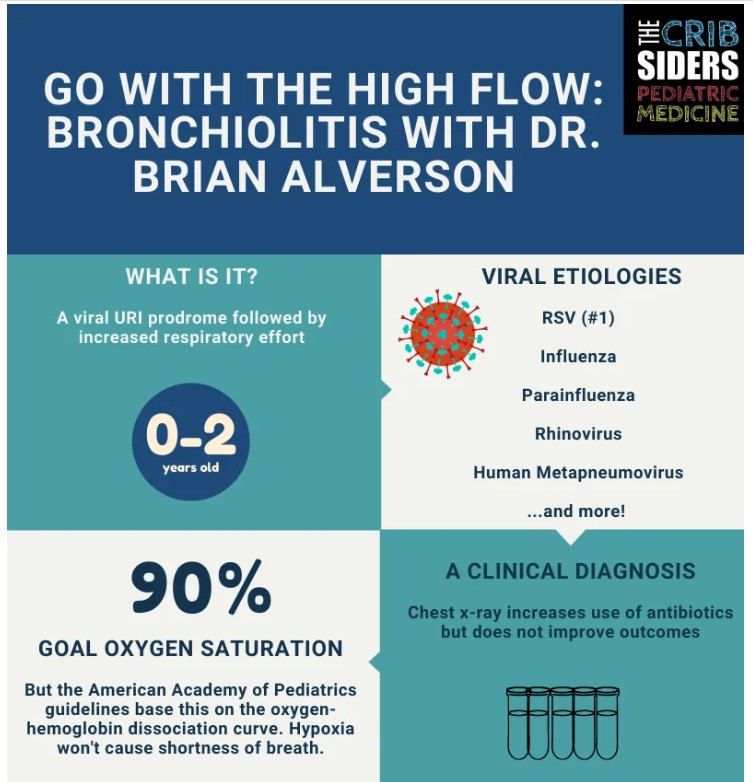
Dive into one of the most common pediatric problems, bronchiolitis, with our guest Dr. Brian Alverson, director of the Division of Hospital Medicine at Hasbro Children’s Hospital. In this episode, we review the workup of bronchiolitis, including the role of the chest x-ray, RPP, CBC, and more. We also discuss the evidence behind treatments such as albuterol, steroids, and high flow nasal cannula. Listen to hear more about this breathtaking topic.
Time Stamps
- Intro 4:00
- Diagnosis of bronchiolitis 7:40
- Oxygenation in Bronchiolitis 10:55
- Appearance and Work of breathing 15:15
- Work-up of Bronchiolitis 16:40
- Future of testing (procalcitonin) 22:30
- The febrile child with bronchiolitis 24:00
- Medical management of bronchiolitis 26:45
- Discussion of critical care and HFNC 37:10
- Admission Criteria 46:45
- Nasal Suctioning 47:40
- Rapid-fire questions (NGT vs IV, readmissions, asthma correlation, viral causes) 49:25
- Final pearls 53:30
Bronchiolitis Pearls
- Transient hypoxemia is not dangerous and is well tolerated in infants.
- In kids who have viral symptoms, chest x-ray increases use of antibiotics but does not improve outcomes.
- Bronchiolitis is a waxing and weaning disease.
- Less frequent superficial nasal suctioning is associated with longer hospitalizations.*
- Readmission rates are associated with living closer to the hospital, young age, and low income zip code.
*Frida Baby Nasal Aspirator NoseFrida the Snotsucker with 24 Extra Hygiene Filters [This is NOT an affiliate link. I just wanted readers to have access.]
Approach to Diagnosis
- Bronchiolitis is a viral infection that is present in the nose and causes mucus production and then progresses to the small areas of the lungs, which makes it hard for babies to breathe.
- Expert opinion: Presume infants with a URI prodrome followed by increased respiratory effort have bronchiolitis to avoid over-testing and over-treating which can cause harm to the patient. Think broader and formulate a differential diagnosis as time passes or the child gets sicker.
Respiratory Assessment
Bronchiolitis versus bronchitis
- Bronchiolitis and bronchitis can both be caused by viruses.
- Editor’s note: Acute bronchitis involves the large airways (bronchi) compared to bronchiolitis which involves the small bronchi and bronchioles.
Hypoxemia in Bronchiolitis
- Transient hypoxemia is not dangerous in infants. Children can tolerate hypoxemia, as they do not have comorbidities like adults (e.g., atherosclerosis).
- Healthy children on a trekking trip to 1700m had an average overnight SpO2 of 86% (Scrase et al. Arch Dis Child. 2009).
- Hypoxia does not make people feel short of breath, so giving oxygen will not make children more comfortable.
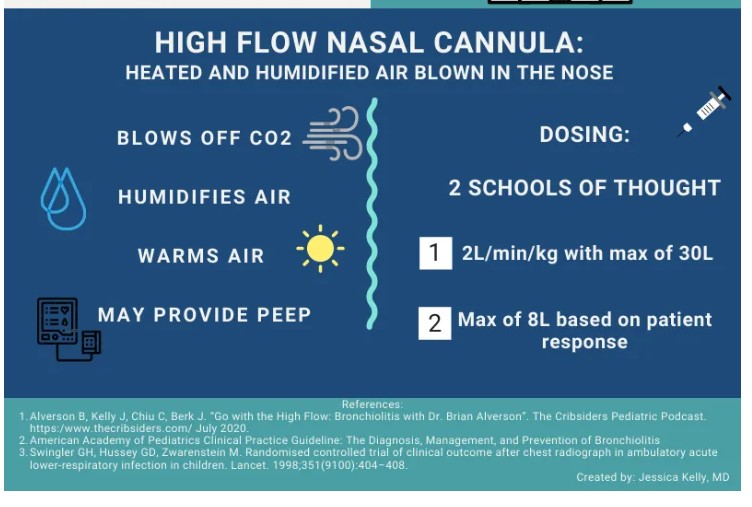
- Bronchiolitis is an issue of CO2 retention more than oxygenation.
Respiratory Status
- Work of breathing can be assessed with retractions
- Retractions are the result of non-compliant lung due to mucus which prevents the lung from expanding and contracting normally
- Children deteriorate when work of breathing exhausts respiratory muscles.
- Expert Opinion: A patient’s respiratory status is more concerning than mild hypoxemia. Practitioner gestalt of the patient, beyond the work of breathing, often plays a role in noticing when a child is in distress.
Diagnostic Workup
- Recommend no testing in the initial workup as per AAP guidelines. Wait and see how the child does with standard therapy for bronchiolitis.
CBC
- Not sensitive or specific in kids for bacterial versus bacterial illness (Virkki et al. Thorax. 2002).
Chem7 / BMP
- Expert opinion: History is a better way to assess hydration status. If worried about significant hydration, consider getting a sodium.
Blood Culture
- After 2 months of age, the utility of the blood culture is low, as false positive rates are greater than true positives (Herz et al. Pediatr Infect Dis J. 2006)
- Expert Opinion: If a patient is septic, very ill, or is premature (higher risk for group B strep), consider a blood culture.
Chest X-ray
- Minimize use of chest x-ray, especially for patients who are relatively well appearing and going to the general wards, as the chest x-ray can cause harm (AAP guidelines).
- In kids with viral symptoms, chest x-ray increases use of antibiotics but does not improve outcomes (Swingler et al. Lancet 1998 and Schuh et al. J Pediatr. 2007).
- Expert Opinion: If a child looks profoundly sick, goes to the ICU, or is intubated, a chest x-ray may be appropriate and you can expand your differential diagnosis.
Future Tests
- In pneumonia, CRP and procalcitonin are better than WBC in distinguishing between bacterial and viral illness (Virkki et al. Thorax. 2002 and Moulin et al. Arch Dis Child. 2001).
The Febrile Bronchiolitic
To Tap or Not to Tap
- Given how ubiquitous RSV is, an infant could have RSV and bacterial meningitis.
- Expert opinion: In febrile infants less than one month, do the full rule out sepsis with blood, urine, and CSF studies.
- Editor’s Note: Audio states the prevalence of meningitis is 0.4% in the first month of life. A recent systematic review of febrile infants found the risk of meningitis is 1% in the first month and 0.4% in the second month of life (Biondi et al. JAMA Netw Open. 2019)
- One study tried to determine if having RSV lowered the risk of having meningitis, but it was not powered to detect a statistically significant difference (Levine et al. Pediatrics. 2004).
- Delay in antibiotics for meningitis is associated with loss in IQ, seizure, and death (Pruitt et al. J Pediatr. 2018 and Bodilsen et al. BMC Infect Dis. 2016).
- Editor’s note: See “Things we do for No Reason: Lumbar Puncture in Low-Risk Febrile Infants with Bronchiolitis” for more.
Management
- Expert opinion: Be suspicious of management bronchiolitis. One study respiratory scored children with bronchiolitis. There was no intervention (except the passage of time) and then re-scored the children. Several patients got dramatically better and several got worse (Fernandes et al. Pediatrics. 2015). Bronchiolitis is a dynamic, waxing and weaning disease.
- We are designed to make connections that might not necessarily be there (see: Cecil Adams and the street lamp phenomenon).
Oxygen
- Oxygen goal: AAP guidelines say 90%. Data is based on oxygen-hemoglobin dissociation curve and not on clinical outcomes.
- Expert Opinion: Don’t fear hypoxemia and be less focused on the pulse ox number.
- Artificially increasing the pulse ox value of patients makes them less likely to be admitted to the hospital but has no differences in outcomes (Schuh et al. JAMA. 2014).
- Editor’s Note: Audio states the pulse ox was decreased but it was artificially increased.
- Infants with bronchiolitis were discharged home with a pulse ox and the majority had desaturations overnight without adverse outcomes (Principi et al. JAMA Pediatr. 2016)
- Editor’s Note: Continuous pulse ox is not necessary per the AAP guidelines. Despite this, almost half of admitted children (not on supplemental oxygen or nasal cannula) are placed on continuous pulse ox (Bonafide et al. JAMA. 2020).
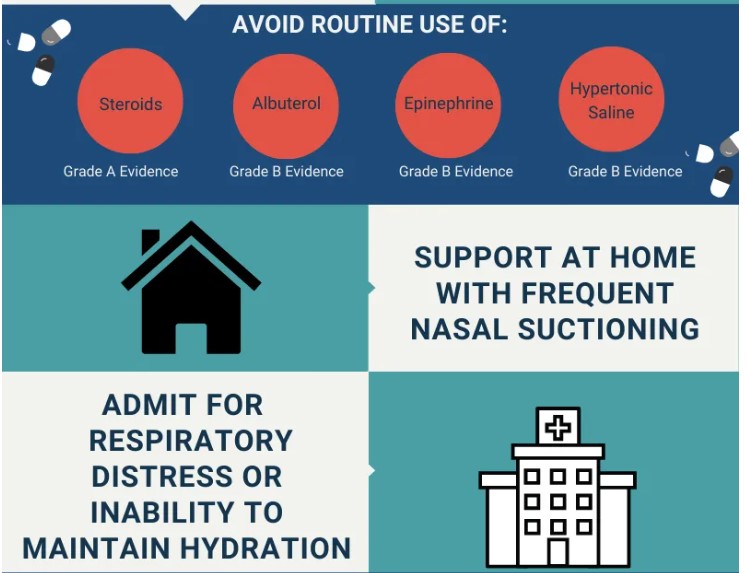
Albuterol*
- AAP guidelines: Clinicians should not use albuterol in inpatient or outpatient settings. Albuterol improves clinical symptom scores but does not affect hospitalization rates or length of stay.
- Expert Opinion: May consider it on a case-to-case basis, including if a child is getting worse or older/atopic infants.
- Albuterol makes babies irritable.
*Please see and review:
-
-
-
-
- Something Is Changing in Viral Infant Bronchiolitis Approach. MINI REVIEW article. Front. Pediatr., 14 April 2022. Sec. Pediatric Pulmonology
Volume 10 – 2022 | https://doi.org/10.3389/fped.2022.865977 - Dr Mellick’s YouTube Video “Treating Bronchiolitis in the Outpatient Setting”-The 2014 AAP Bronchiolitis Guidelines Are Wrong
Posted on May 25, 2022 by Tom Wade MD
- Something Is Changing in Viral Infant Bronchiolitis Approach. MINI REVIEW article. Front. Pediatr., 14 April 2022. Sec. Pediatric Pulmonology
-
-
-
Steroids
- AAP guidelines: Clinicians should not administer systemic corticosteroids to infants with a diagnosis of bronchiolitis in any setting (the only guide line with evidence quality A).
- Many adverse effects of steroids, including growth suppression
- One study gave dexamethasone daily for 5 days, and patients went home 9 hours sooner with no other significant outcomes (Alansari et al. Pediatrics. 2013).
Hypertonic Saline
- AAP guidelines: Not recommended.
- Does not decrease length of stay (Wu et al. JAMA Pediatr. 2014).
Hospital Level of Care
- Mortality is rare in bronchiolitis in healthy kids (Doucette et al. PLoS One. 2016)
- Expert Opinion: When you need to escalate care, remember no medication will make bronchiolitis better. Open up your differential diagnosis (e.g., sepsis, pneumonia, or spontaneous pneumothorax) and consider further work-up (e.g., chest x-ray, blood gas, or blood culture).
Admission criteria
- Respiratory distress: Can be hard to define, but if you’re concerned about a patient, send them into the hospital to be evaluated.
- Hydration status*: Assess with a good history. If a patient is making good wet diapers, they are likely well hydrated.
*Please review:
-
-
-
- Emergency Department Clinical Pathway for Healthy Children with Gastroenteritis/ Dehydration from The Children’s Hospital Of Philadelphia [accessed 11-26-2023]
- Emergency Department and Inpatient Clinical Pathway for Oral or Enteral Feeding in Children with Bronchiolitis from The Children’s Hospital Of Philadelphia [accessed 11-26-2023]
-
-
Outpatient Management
Things to Do at Home
- Expert opinion: Nasal suctioning: parent-activated nasal suctioning device (ex. Nose Frida). Spray saline and then the parent sucks the mucus out (there is a filter so it does not go in the parent’s mouth). Works better than the little blue bulb. Suction every few hours, especially before feeds.
- One study showed both deep suctioning and lapses of greater than 4 hours in nasal suctioning were associated with longer LOS (Mussman et al. JAMA Pediatr. 2013).
A few last pearls…
Hydration: NG Tube vs IV fluids?
- Expert opinion: Prefer NG tube. Involve parents in the decision
- In older kids who can rip out NGT, may want to choose IV
Readmission rates
- More likely to be readmitted if you live close to the hospital (Riese. Hosp Pediatr. 2014)
- Editor’s note: Young age and low income zip code also were associated with readmission.
Is Bronchiolitis Associated with Developing Asthma Later on in Life?
- Some studies argue that RSV infection in infancy increases risk of asthma (Jartti et al. Semin Immunopathol. 2020)
- Expert opinion: Maybe. It is unclear. It is possible that there is some underlying lung parenchymal response that causes kids to react badly to RSV and develop asthma later. The vast majority of kids who have bronchitis do not develop asthma
Typical Age for Bronchiolitis
- Kids under 2
- Can happen up to age 4, but is more rare. These kids get a bigger work up.
- One theory for bronchiolitis happening in the younger age group: these kids don’t have Pores of Khan and Canals of Lambert.
The Respiratory Viral Panel
- Many viruses cause bronchiolitis: RSV, flu, human metapneumovirus, rhinovirus, parainfluenza virus.
Expert opinion: Ok to get it if you promise yourself it will change management. Remember the cost (~$100). Reasonable (at this time) to test for COVID-19 in hospitalized patients.