In addition to today’s resource, please see and review:
- Imaging protocols for CT chest: A recommendation [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Indian J Radiol Imaging. Jul-Sep 2019;29(3):236-246
- Diagnostic Imaging Pathways – Dyspnoea (Chronic). Date Reviewed: 2012
- Diagnostic Imaging Pathways – Bronchiectasis. Date reviewed: May 2018.
- Diagnostic Imaging Pathways-Common Procedures: High Resolution Computed Tomography (HRCT) From Diagnostic Imaging Pathways. Date reviewed: July 2019
- Diagnostic Imaging Pathways – High Resolution Computed Tomography (HRCT) of the Lung. Date Reviewed: May 2011.
In this post, I link to and excerpt from The Curbsiders‘ [Link is to the Complete Episode List] “#306 Bronchiectasis and Non-Tuberculous Mycobacterium“, By
All that follows is from this outstanding podcast and show notes:
Show Segments
- Intro, disclaimer, guest bio
- Guest introduction and recommendations
- Case from Kashlak – Part I: The Basics
- What is bronchiectasis, how do we define it?
- Symptoms and history
- Why does it matter?
- What should you ask, how do you work this up?
- A brief discussion on antibiotics
- Case from Kashlak – Part II: Getting into the Management
- Airway Clearance
- Case from Kashlak – Part III: The Sputum (Plot) Thickens
- What is a bronchiectasis exacerbation?
- Pitfall and pearls regarding exacerbation management
- Case from Kashlak – Part IV: The Sputum (Plot) Thickens Even Further!
- Non-tuberculous Mycobacterial Infections – the basics
- Triple Drug Therapy for MAC
- The new kid on the block: Liposomal Inhaled Amikacin for refractory MAC
- Summary and take home points from Dr. McShane
- Outro
Bronchiectasis Pearls
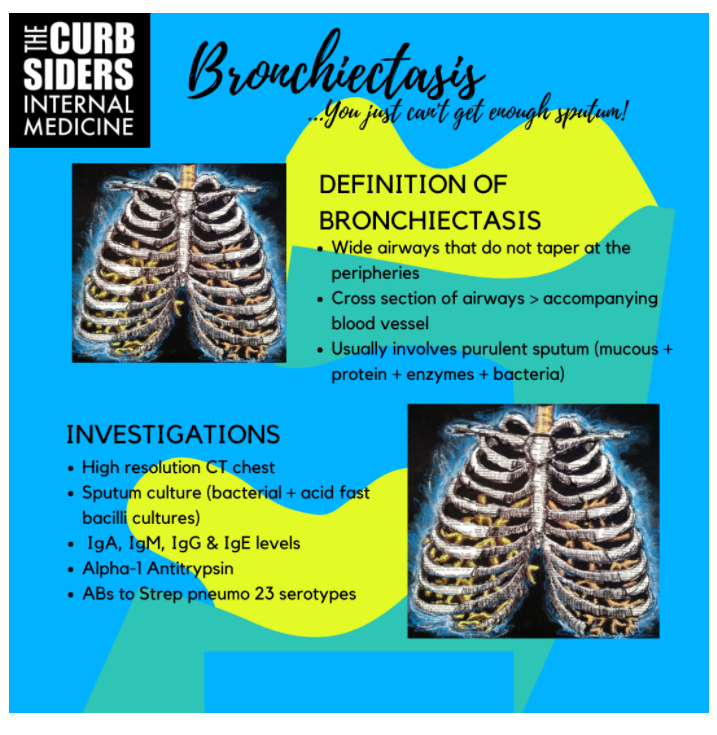
- Bronchiectasis definition: airway widening on CT imaging (larger airway than accompanying vessel); symptoms: usually include purulent sputum, dyspnea/exercise intolerance, cough and potentially malaise and/or hemoptysis.
- Consider eval for bronchiectasis (CT chest) for patients treated for “non-resolving” pneumonia/COPD exacerbations, or, those with obstructive PFTs without a smoking history- especially those encountered in their 5th or 6th decade of life.
- Sputum sampling is incredibly helpful to identify pathogenic organisms that, in the event of an exacerbation, can be targeted for treatment.
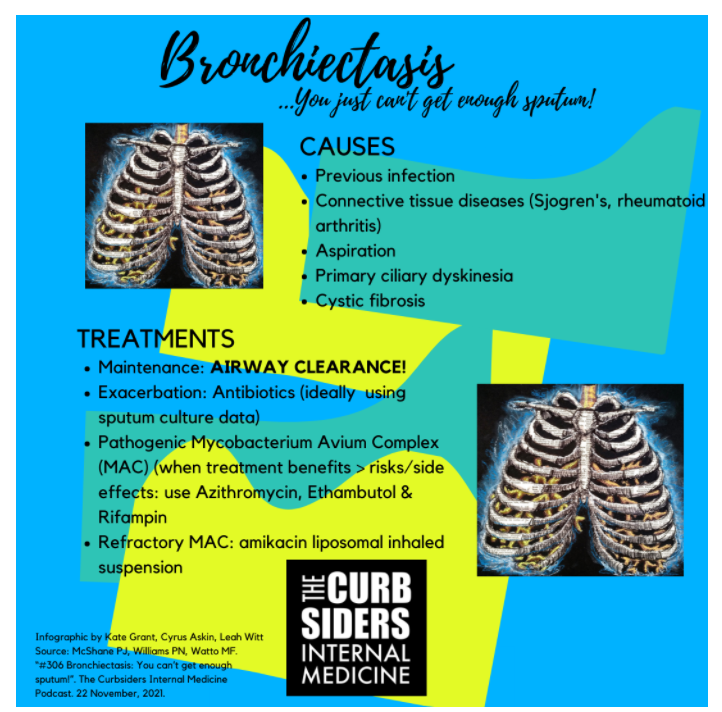
- In stable bronchiectasis, airway clearance (+/- hypertonic saline + active cycle breathing maneuvers + some form of vibrating positive pressure device) forms the cornerstone of therapy.
- Bronchiectasis exacerbation definition: 48+ hours of worsening symptoms (3 or more of the hallmark symptoms) plus a clinician’s decision to change/add therapy based upon the clinical presentation.
- Non-tuberculosis mycobacteria (NTM) are environmental pathogens that normally don’t cause disease in immunocompetent patients with normal lung architecture, common agents include Mycobacterium Avium Complex (MAC), M. abscessus and M. kansasii.
- When treatment benefits outweigh risks/adverse events, treatment for MAC in bronchiectasis is a multi-month triple-drug regimen that includes a macrolide (usually azithromycin) + ethambutol + rifamycin.
- In patients that are refractory to the aforementioned treatment, the addition of amikacin liposomal inhalation suspension (“ALIS”) has been demonstrated to increase conversion of positive sputum samples to negative.
Note to myself: When I review this post, I also need to go to #306 show notes and review them as they are outstanding.
See my posts on High Resolution Chest CT – coming soon.