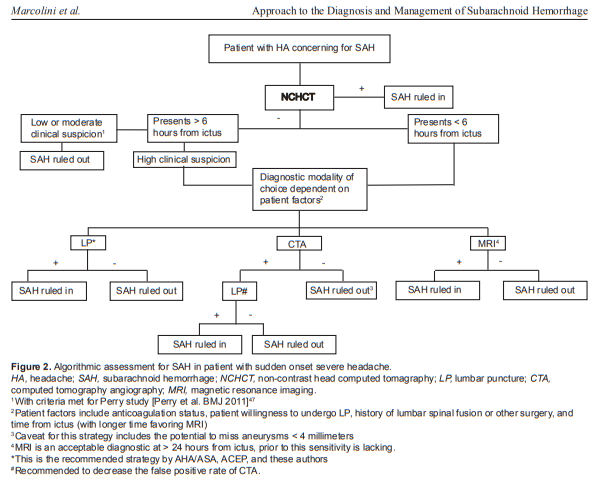
In this post I link to and excerpt from the excellent “Approach to the Diagnosis and Management of Subarachnoid Hemorrhage” [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Evie Marcolini, MD and Jason Hine, MD. West J Emerg Med. 2019 Mar; 20(2): 203–211.
Abstract
Headache is one of the most common reasons for presentation to the emergency department (ED), seen in up to 2% of patients.1 Most are benign, but it is imperative to understand and discern the life-threatening causes of headache when they present. Headache caused by a subarachnoid hemorrhage (SAH) from a ruptured aneurysm is one of the most deadly, with a median case-fatality of 27–44%.2 Fortunately, it is also rare, comprising only 1% of all headaches presenting to the ED.3 On initial presentation, the one-year mortality of untreated SAH is up to 65%.4 With appropriate diagnosis and treatment, mortality can be reduced to 18%.5 The implications are profound: Our careful assessment leading to the detection of a SAH as the cause of headache can significantly decrease our patients’ mortality. If this were an easy task, the 12% reported rate of missed diagnosis would not exist.6 We have multiple tools and strategies to evaluate the patient with severe headache and must understand the strengths and limitations of each tool. Herein we will describe the available strategies, as well as the ED management of the patient with SAH.
Pathophysiology
Eighty-five percent of cases of atraumatic SAH result
from a ruptured aneurysm.7 Alternate etiologies include
perimesencephalic hemorrhage, which has a benign course, as
well as arteriovenous malformations, dural arteriovenous fistula, arterial dissection, mycotic aneurysm, and cocaine abuse. The prevalence of aneurysms in the general population is roughly 2-5%,8 greater in those with family history of aneurysms, and/or personal history of Ehlers-Danlos or polycystic kidney disease.Aneurysms typically present at cerebral artery bifurcation
points in both anterior or posterior regions.Diagnosis
The diagnosis of SAH should be considered in any patient
with a severe and sudden onset or rapidly escalating headache.
With such a large number of patients presenting to the ED
with a chief complaint of headache, differentiating those with
a benign cause from those with an emergent etiology such
as SAH can be difficult. Deciding which patients require a
workup for SAH is often the most challenging part of the
emergency physician’s care, in part due to the low frequency
and high acuity of the illness.Diagnostic Tools
Computed Tomography
When a clinical suspicion for SAH exists based on history and physical exam, non-contrast computed tomography (CT) is the first diagnostic tool. It is also valuable in excluding other pathologies such as intracranial hemorrhage, malignancy, or abscess.
Timing of Computed Tomography
At the onset of the bleed, subarachnoid blood is the most readily visible on CT, but it becomes more difficult to appreciate as red blood cell (RBC) degradation progresses. Advances in neuroimaging have increased the sensitivity of non-contrast CT, raising questions regarding the need for lumbar puncture (LP) in the face of a negative CT.
Lumbar Puncture
If non-contrast head CT is not definitive (time to study, patient
elements [i.e., severe anemia], interpretation limitations [i.e.,
trainee radiologist, motion artifact], etc) the next recommended
diagnostic tool is the LP. In these instances the LP is looking for
two elements that raise the concern for SAH: 1) RBCs; and 2)
xanthochromia (bilirubin in cerebrospinal fluid [CSF]).Given the sensitivity of the CT discussed above, shared
decision-making should be conducted with regard to LP.
In particular, with sensitivity of near 99% for an adequate
study if completed within six hours, and meeting the criteria
outlined above (Dubosh), patients should be made aware of
the low diagnostic utility of LP if completed after a CT.19 In
this setting, risks (adverse events and false positives) generally
outweigh benefits and LP is advised against.Computed Tomography Angiography
Over the last decade, CTA of the brain has become part of
the discussion in ruling out SAH. As a non-invasive means of
highlighting vascular anatomy and detecting aneurysms, CTA has many advantages. Much like non-contrast head CT, advances in neuroimaging have shown CTA to have a sensitivity of up to 98% and a specificity of 100% for aneurysms in patients with known SAH. These statistics are derived from a small data set (n= 65) where CTA results were compared to gold standards of digital subtraction angiography or surgical findings.30,31Some propose CTA as an alternative to LP after a negative
non-contrast CT.19,31 With the prevalence of aneurysms estimated to be ~2-5% in the general population,8
there is a concern for incidental findings and false positives. An aneurysm found on CTA may be incidental and unrelated to the cause of headache.[There are many factors to consider in using the CTA for subarachnoid hemorrhage rule out. Please review entire section of the paper.]