In this post I link to and excerpt from the Curbsiders‘ [Link is to the episode list] podcast and show notes, “#221 Interstitial Lung Disease with Erin Narewski DO,” of JUNE 22, 2020 By DR PAUL WILLIAMS:
Summary
Throw out your down pillows and join The Curbsiders for this lively discussion on interstitial lung disease. While the hundreds of interstitial lung disease types make this topic a bit overwhelming, breathe easy knowing that pulmonologist, Dr. Erin Narewski @erinnarewski (Temple), can boil things down to an easy to approach framework in less time than it takes to complete a few 6-minute walk tests. In this episode, we walk through the classification, relevant patient history, workup, and management of interstitial lung disease.
And here are excerpts:
Time Stamps
- 0:00 Sponsor – Join the ACP community! Be IM Proud Visit acponline.org/member and use the code ACPDISCOUNT
- 00:30 Intro, disclaimer, guest bio
- 03:14 Guest one-liner, career advice, favorite failure, Picks of the Week*: The Strain, FX Horror TV Show; One Hundred Years of Solitude (book) by Gabriel Garcia Marquez; Hypoallergenic pillows; Peanut butter whiskey
- 10:02 Sponsor – Join the ACP community! Be IM Proud Visit acponline.org/member and use the code ACPDISCOUNT
- 11:00 Case from Kashlak, Definitions
- 16:40 Buckets of ILD
- 32:06 Discussion of testing ILD: Labs and Imaging
- 44:20 Imaging findings in ILD
- 49:44 Basic Management of ILD
- 61:00 Take home points and Outro
Two questionnaires Dr. Narewski recommends for the evaluation of possible Interstitial Lung Disease (ILD):
Interstitial Lung Disease Pearls
- Interstitial lung disease (ILD) is a relatively uncommon cause of dyspnea, but due to its severity, ILD should always be on the back of your differential.
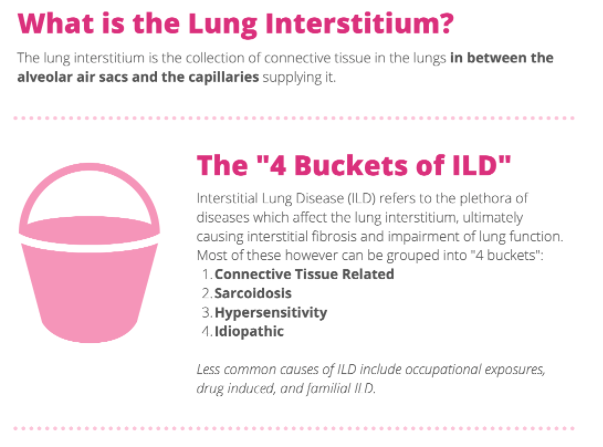
- ILD comprises a diverse family of illnesses that fall into four main buckets: connective tissue disease, sarcoidosis related disease, hypersensitivity pneumonitis, and idiopathic pulmonary fibrosis.
- Not all ILD patients report dyspnea, cough, or have restrictive characteristics on pulmonary function tests.
- Be careful when evaluating dyspnea; some patients adjust activity for lung function and may not feel short of breath.
- Some patients may not know that they received amiodarone while hospitalized for a cardiac condition, so it can be useful to ask about a history of cardiac surgery, arrest, or arrhythmia.
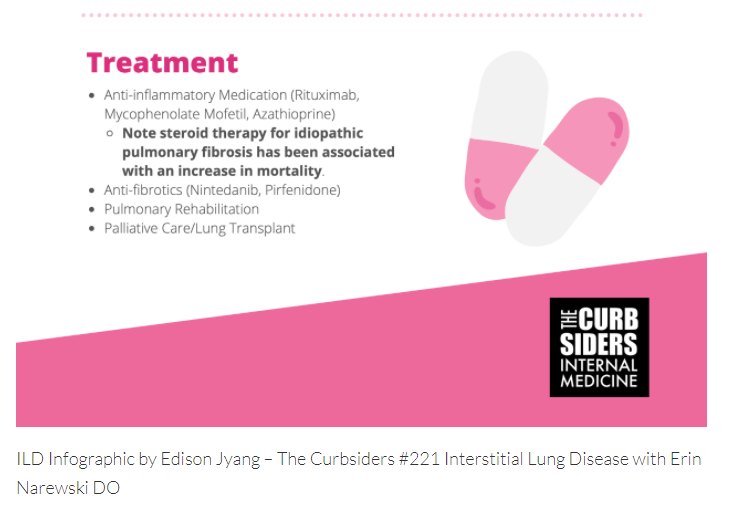
- Corticosteroids in idiopathic pulmonary fibrosis are associated with an increase in mortality, so it is important to understand the etiology of ILD before prescribing this medication class (PANTHER-IPF 2012).
- The adult oxygen saturation goal is >94%, and too much oxygen can be harmful (Chu et al. 2018).
Does My Patient Have Interstitial Lung Disease?
History for ILD
A comprehensive patient history is the key to unlocking an ILD diagnosis. Questions can be focused on each of the causes of ILD. For a potential connective tissue etiology, questions about changes in skin, hair, dry eyes, or dry mouth can indicate the underlying pathology. Presence of arthropathy or fatigue could indicate sarcoidosis. Hypersensitivity to antigens could be assessed with questions about wheezing or squeaking sounds in the chest, birds, down products, house age or a history of water damage at home or work. Possible occupational exposures can be assessed by asking the patient where they work or if they are required to wear ppe at work. Additionally, the Dyspnea 12 Questionnaire can be used to quantify symptomatology. Be careful when evaluating dyspnea; some patients adjust activity for lung function and may not feel short of breath.
MEDICATIONS
The CHEST ILD questionnaire covers many medications linked to ILD, but additional history focused on medications can be useful. Some patients may not know that they received amiodarone while hospitalized for a cardiac condition, so it can be useful to ask about a history of cardiac surgery, arrest, or arrhythmia. If the patient has an extensive history of urinary tract infections, they may not remember the name of the medication they took, but nitrofurantoin could be a cause. A cancer history could indicate exposure to chemotherapy or radiation. Methotrexate has also been linked with ILD (Fragoulis et al 2019).