Today, I reviewed, link to, and excerpt from A Novel Method for Estimating Right Atrial Pressure With Point-of-Care Ultrasound [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Larry Istrail 1, Joseph Kiernan 2, Maria Stepanova 3. J Am Soc Echocardiogr. 2023 Mar;36(3):278-283. doi: 10.1016/j.echo.2022.12.008. Epub 2022 Dec 13.
- There are 103 similar articles in PubMed.
- Here is the link to the YouTube video, Jugular Venous Pressure (JVP) Exam using Point-of-care Ultrasound (POCUS), by the author of the above article. POCUS Med Ed. “Jan 1, 2023. With Point-of-care ultrasound (POCUS), you can measure the JVP accurately in every patient regardless of their BMI using this method. This has been validated against right heart cath right atrial pressure measurements and is within 3 mmHg in most patients.
- Validation study: https://bit.ly/3YXlH6F
- The Pocus Manifesto: https://amzn.to/3EZoEu5
- For more on POCUS see https://www.pocusmeded.com/
- The above article has been cited by
- Seeing beneath the surface: Harnessing point-of-care ultrasound for internal jugular vein evaluation.
- Chayapinun V, Koratala A, Assavapokee T.World J Cardiol. 2024 Feb 26;16(2):73-79. doi: 10.4330/wjc.v16.i2.73.PMID: 38456073 Free PMC article. Review.
- Evaluation of an artificial intelligence-based system for echocardiographic estimation of right atrial pressure.
- Int JCardiovasc Imaging. 2023 Dec;39(12):2437-2450. doi: 10.1007/s10554-023-02941-8. Epub 2023 Sep 8.PMID: 37682418 Free PMC article.
- Int JCardiovasc Imaging. 2023 Dec;39(12):2437-2450. doi: 10.1007/s10554-023-02941-8. Epub 2023 Sep 8.PMID: 37682418 Free PMC article.
- Seeing beneath the surface: Harnessing point-of-care ultrasound for internal jugular vein evaluation.
All that follows is from the above resource.
Highlights
• Current noninvasive RAP measurements are inaccurate.
• Inaccuracies are due in part to the belief that RAD is 5 cm below the sternum.
• We propose a novel method to measure RAD with POCUS.
• This method predicted actual RAP within 3 mm Hg 74% of the time.
Background
Current noninvasive estimation of right atrial pressure (RAP) by either bedside jugular venous pressure exam or inferior vena cava measurement during a comprehensive echocardiogram offers imprecise estimates of actual RAP.
Methods
We enrolled 41 patients in a prospective, blinded study to validate a novel point-of-care ultrasound method using direct right atrial depth (RAD) measurement and jugular venous ultrasound to estimate RAP. Two subjects were excluded, and 39 were included in the final analysis. A parasternal long-axis view was obtained, and the depth of the noncoronary cusp attachment to the posterior left ventricular outflow tract was recorded as the RAD. This was added to an estimate of the jugular venous pressure obtained during a jugular vein ultrasound to calculate an estimated RAP (RAPUS). The RAPUS was compared to the RAP measurement during right heart catheterization (RAPcath) both as measured and as corrected for where the catheter was zeroed.
Results
The correlation coefficient between RAPcath and RAPUS was +0.75; regression R2, 0.56; and bias, –0.49 mm Hg (95% CI, −1.42 to +0.43 mm Hg), with the limits of agreement −5.56 to +7.24 mm Hg and accuracy of 3 mm Hg or less in 29 (74%) of the subjects. For the RAPUS corrected for the catheter zero point, the correlation coefficient between RAPcath and RAPUS was +0.72; regression R2, 0.52; and bias, –0.60 mm Hg (95% CI, −1.60 to +0.39 mm Hg), with the limits of agreement −5.56 to +7.24 mm Hg and accuracy of 3 mm Hg or less in 26 (67%) of the subjects.
Conclusion
This simple ultrasound evaluation of RAD and the right jugular vein correlates well with actual RAP and can accurately estimate RAP within 3 mm Hg in most patients. This has the potential to improve our bedside volume status exam, as well as improve the accuracy of RAP estimation during comprehensive echocardiogram.
Keywords
Abbreviations:
AP (Anterior-posterior), IJV (Internal jugular vein), IVC (Inferior vena cava), JVD (Jugular venous distention), LVOT (Left ventricular outflow tract), POCUS (Point-of-care ultrasound), RAD (Right atrial depth), RAP (Right atrial pressure), RHC (Right heart catheterization)
Noninvasive estimation of right atrial pressure (RAP) is currently done by either bedside jugular venous pressure exam or by measuring inferior vena cava (IVC) diameter and collapsibility during a comprehensive echocardiogram. However, both of these measures offer imprecise estimates of actual RAP. The visual inspection of the jugular vein first described by Sir Thomas Lewis in 1930 has been the basis of our volume exam.1 The principle used to measure the pressure is based on the fact that in a semiupright position, the internal jugular vein (IJV) is partially filled with blood and collapses above the level that blood reaches up to.2 When the blood reaches above the clavicle, this collapse point can often be visualized through the skin on the lateral portion of the neck. The vertical distance from the sternal angle to this collapse point can be measured and used to estimate the jugular venous pressure.
However, this method has many limitations that result in poor sensitivity and low diagnostic accuracy, such as the inability to visualize the jugular vein in patients with thick necks or who are obese.3, 4, 5, 6, 7, 8, 9 This method also assumes the right atrium is 5 cm below the sternum based on data from a 1946 study using chest x-rays,10 when in fact it can vary from 5 to 15 cm.11, 12
Echocardiographic IVC measurement to estimate RAP is the current noninvasive gold standard; however, it only offers a very weak correlation to actual RAP. In a blinded, prospective study, Magnino et al.13 found that both IVC diameter and collapsibility had an R2 of 0.19 or less and were within 2.5 mm Hg of the actual value only 34% of the time.13 These inaccuracies lead to overestimations in pulmonary pressures, can misguide diuretic treatment choices, and ultimately lead to clinical uncertainty and invasive right heart catheterizations (RHCs) to make the final determination of volume status.14 Point-of-care ultrasound (POCUS) offers alternative methods for estimating RAP at the bedside. It can overcome the anatomical limitations present in visually inspecting the jugular vein and can also measure the right atrial depth (RAD) in each patient. Taken together, these 2 measurements may provide a more accurate, noninvasive, and quantitative measurement of RAP.Methods
A prospective, blinded study was completed to compare the ability of a novel IJV ultrasound technique to estimate RAP as compared to the RAP obtained from an RHC. Patients undergoing an RHC were recruited for this study if they were 21 years old or over and required RHC for any purpose. Patients were excluded from the study based on the following: (1) right IJV catheter present, due to the fact that the catheter and bandage prevent full visualization of the right IJV with ultrasound; (2) intubated or on positive pressure ventilation; (3) congenital heart disease history; (4) unable to visualize the posterior left ventricular outflow tract (LVOT) in the parasternal long-axis view. All patients provided written informed consent before enrollment in the study. The study was approved by the Institutional Review Board.
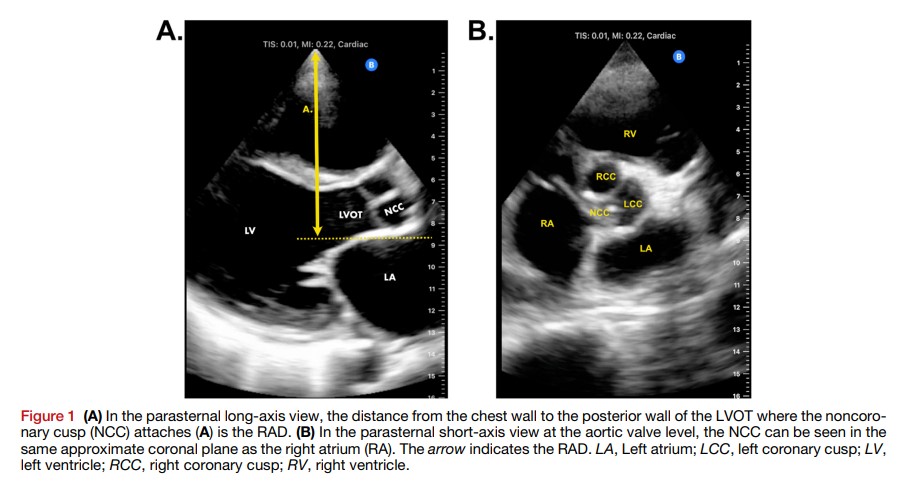
Within 2 hours prior to the RHC, the patient’s head of the bed was placed at 45°, and one physician certified in POCUS by the Society of Hospital Medicine and CHEST with 5 years of POCUS experience (L.I.) performed the ultrasound exam. A Butterfly IQ+ (manufactured by Butterfly Network) probe was placed along the left sternal border, and a cardiac parasternal long-axis view was acquired. The distance from the chest wall down to where the noncoronary cusp of the aortic valve attaches to the posterior wall of the LVOT was measured (Figure 1A). This landmark was chosen as a surrogate for the center of the right atrium because it sits in the same approximate coronal plane as seen in the parasternal short-axis view at the aortic valve level (Figure 1B) and is easily detectable in a supine patient. This distance was recorded as the RAD.
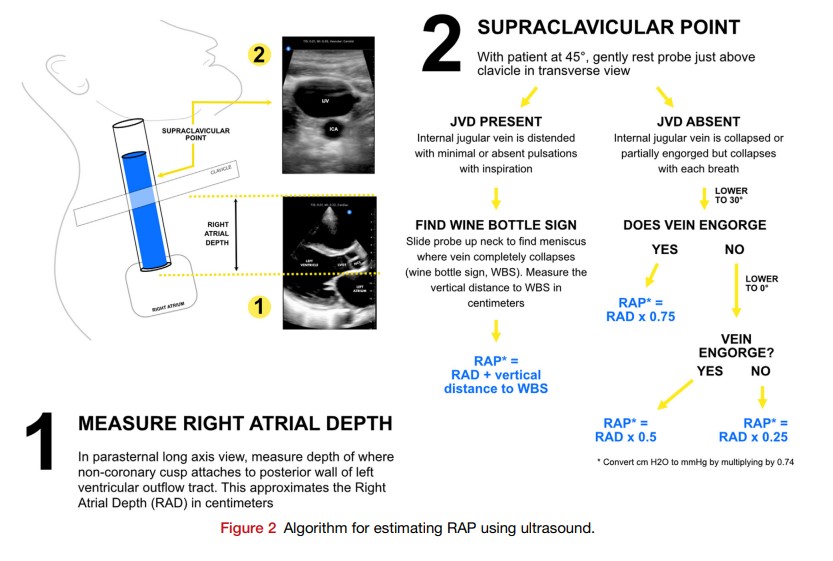
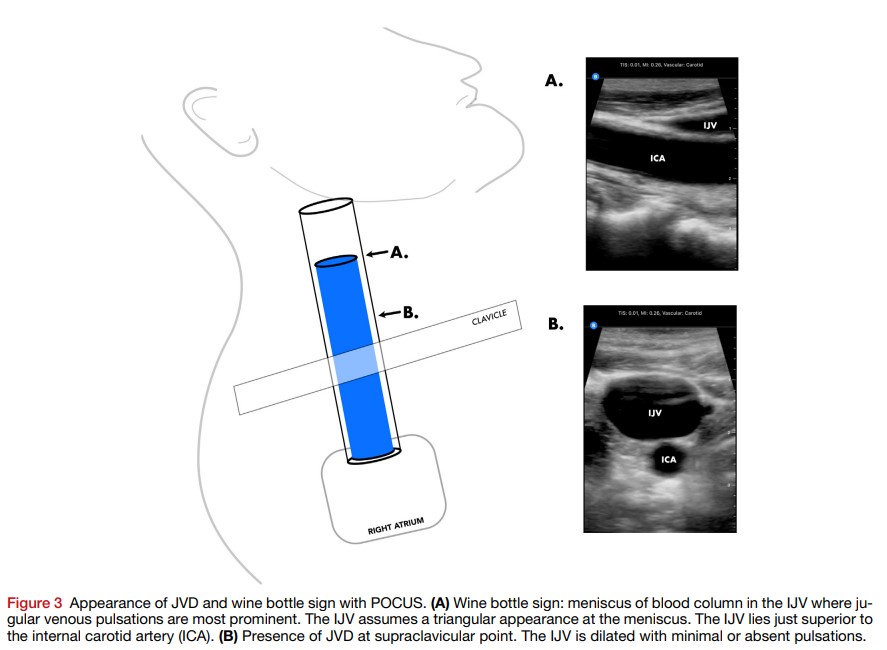
The probe was then gently placed just superior to the clavicle at what we arbitrarily called the supraclavicular point. In the transverse view, the right IJV was visualized, and a clip at this point was recorded. The IJV shape was characterized as oval, triangular, or circular, and degree of collapsibility was characterized as completely collapsed, partially filled with respiratory variation, or distended without respiratory variation. If the IJV was distended without respiratory variation at the supraclavicular point, jugular venous distention (JVD) was considered present. If the IJV collapsed with normal respiration, then the JVD was deemed absent.
If the IJV at the supraclavicular point was completely collapsing with normal inspiration with the head of the bed at 45°, then JVD was deemed absent. To estimate the pressure in this case, the angle of the head of the bed was lowered to allow for more blood to fill the IJV to determine at what angle the vein engorges. The head of bed was first lowered to 30°, and the IJV was assessed for partial or full engorgement greater than that seen at 45°. If the vein did not engorge to a greater degree than at the 45° position, then the head of the bed was dropped further to 0°, and the presence of partial or full engorgement was recorded.
If the vein engorged at 30°, then the RAPUS in cmH2O was hypothesized to be RAD × 0.75. If the IJV engorged at 0°, then the RAP was hypothesized to be RAD × 0.5. If the vein still did not engorge at 0°, then the RAP was hypothesized to be RAD × 0.25. These pressure correction factors are estimates based on clinical experience with engorgement of the IJV as the head of the bed is lowered. The pressure in cmH2O was then converted to mmHg by multiplying by 0.735. Immediately prior to the RHC, the interventional cardiologist then measured the anterior-posterior (AP) diameter of the chest and zeroed the catheter at the mid-AP diameter. The estimated RAPUS was then recorded using the RAD measured with ultrasound (Figure 2), as was the RAPUS corrected for the mid-AP diameter to correspond with the RHC zero point. This was done to determine whether correcting the RAD for the mid-AP diameter of the chest where the RHC catheter was zeroed would impact the final pressure estimate. Both values were then entered into the REDCap database prior to the RHC.
Discussion
Right atrial pressure offers insight into the right-sided pressures and overall volume status. Accurate estimation is important for a bedside clinical examination, as well as for estimating volume status and pulmonary pressures from a comprehensive echocardiogram. Inferior vena cava diameter and collapsibility are used to estimate RAP as low, intermediate, or high. Since this is a qualitative estimate, it cannot provide an actual value and has been shown to be inaccurate.13, 16The main finding of this study is that a measurement of RAD coupled with jugular venous ultrasound exam can accurately estimate RAP. This method offers multiple potential improvements over the current gold standard of using IVC diameter and collapsibility. The IJV visibility is not limited by body habitus or presence of bowel gas and is therefore easier to visualize than the IVC. It is also a quantitative estimate of actual RAP rather than a qualitative measurement. It can be performed during a bedside examination as well as to measure RAP during a comprehensive echocardiogram.
In summary, we believe this method could offer a simple and reliable noninvasive RAP estimate, which would have a profound impact on bedside medicine, diuretic use, need for RHC in patients with unclear volume status, and accuracy of volume status and pulmonary pressures during comprehensive echocardiograms.