For non-intensivist clinicians called upon to pitch in during the current COVID-19 crisis, the article referenced below is an outstanding resource.
In this post I link to and excerpt from “Clinical management of pressure control ventilation: An algorithmic method of patient ventilatory management to address “forgotten but important variables” [PubMed Abstract] [Full Text HTML] [Download Full Text PDF]. J Crit Care. 2018 Feb;43:169-182.
Here are excerpts:
1. Introduction
Pressure control as a mode of ventilation was developed in the
1980’s as an option to treat Acute Respiratory Distress Syndrome (ARDS) [1].Pressure Control Ventilation (PCV), typically available as
Pressure control–continuous mandatory ventilation (PC-CMV) or Pressure control-intermittent mandatory ventilation (PC-IMV), was designed to deliver mechanical breaths at a set inspiratory pressure—allowing clinicians to control the amount of distending pressure applied to airways and subsequently, to the alveoli.Because the amount of driving pressure applied to the airway is preset, the delivered volume is variable and dependent upon the patient’s inspiratory effort, pulmonary mechanics (i.e. pulmonary compliance, airway resistance and AutoPEEP) and to a lesser extent, other ventilator settings, including
rise time and inspiratory time.This article does not attempt to dictate a management approach; rather, the goal of this article is to first provide a brief overview of how PC-CMV differs from modes of volume ventilation, then to highlight the detailed nature of the relationships between pulmonary mechanics and PC-CMV settings and finally, to suggest a broad, yet systematic, algorithmic approach to managing patients in the Intensive Care Unit who are ventilated using PC-CMV.
2. Pressure and Volume Controlled Modes Of Ventilation
Pressure-controlled ventilation (PCV) is a pressure-targeted, timecycled mode of ventilation. During inspiration, the ventilator adjusts the flowrate to keep the airway pressure at the set level.
The clinician sets the peak inspiratory pressure (PIP), respiratory rate (f), inspiratory time (TI), positive end expiratory pressure (PEEP) and fraction of inspired oxygen (FIO2). The clinician also sets how quickly the PIP will
be reached with a control usually named slope, rise time or ramp, depending upon the brand of the ventilator.The most common mode of PCV is pressure-targeted assist-control (PC-CMV), in which a minimum respiratory rate is set, but the patient is allowed to trigger additional breaths. Each breath, whether it is delivered at the set respiratory rate or an additional breath triggered by the patient, is delivered at the set
PIP and the set TI.Volume-controlled ventilation (VCV) is a volume-targeted mode in which the tidal volume, respiratory rate (f), PEEP, inspiratory flowrate, flow waveform, inspiratory pause time and inspiratory time are controlled.
The most common mode of VCV is volume-targeted assist-control (VC-CMV), in which a minimum f is set, but the patient is allowed to trigger additional breaths. Each breath, regardless of whether it is patient or machine-triggered, will be delivered at the set tidal volume; however, the airway pressure may vary as the patient’s airway resistance (Raw), compliance (C) and effort change.
3. Patient-ventilator synchrony during VC-CMV and PC-CMV
Although VC-CMV guarantees tidal volume, which appears to be an ideal mode for “lung protective strategy”, many clinicians prefer PCCMV to VC-CMV. The main reason for the preference is probably the superiority in patient-ventilator synchrony and thus patient comfort during PC-CMV. To meet the respiratory demands of a patient, the ventilator’s flow and pressure delivery must synchronize with the patient’s respiratory demands. The fact that a patient is able to control inspiratory flowrate is the most important aspect of PC-CMV in terms of patient-ventilator synchrony.
[In PC-CMV, the patient’s] inspiratory flow rate is set by the clinician. When the patient’s flow demand is not met in VC-CMV, it is common that the demand for tidal volume is not met. As a result, flow asynchrony is frequently accompanied by cycle asynchrony and double triggering.
4. Comparing VC-CMV to PC-CMV in the literature
[Review this section in page 171 of the PDF.]
5. Prerequisite physiological knowledge regarding inspiratory time, expiratory time and inspiratory pressure before using PC-CMV
5.1. Time constant and autoPEEP
The time constant (TC) is a mathematical relationship between the airway resistance and static compliance, and is related to the time it takes to get gas into and out of the lung.
The following two examples demonstrate a difference in the time
constant for two patients:In a patient with COPD who is intubated and mechanically ventilated, the airway resistance may be 25 cm H2O/l/s and the compliance may be 0.04 l/cm H2O. The expiratory resistance will be higher than the inspiratory resistance in these patients, which results in a longer expiratory time constant [5]. In this case the inspiratory time constant would be 1.0 s (25 cm H2O/l/s × 0.04 l/cm H2O).
In a patient with ARDS who is intubated and mechanically ventilated, the airway resistance may be 12 cm H2O/l/s and the compliance may be 0.02 l/cm H2O. In this case the time constant would be 0.24 s (12 cm H2O/l/s × 0.02 l/cm H2O).
The inspiratory time constant refers to the amount of inspiratory time required for the alveolar pressure to reach the set pressure during PC-CMV
The inspiratory time must be equal to at least three and as long as five time constants for the alveolar pressure to approximate the set inspiratory pressure [5,6,7].
If the airway resistance or compliance increases, the inspiratory time constant will increase, and more time
will be required for the alveolar pressure to reach the set pressureIf airway resistance or pulmonary compliance decreases, the inspiratory time constant will decrease and it will take less time for the alveolar pressure to reach the set pressure.
The expiratory time constant influences the amount of expiratory time required for the patient to passively exhale to the PEEP level and prevent AutoPEEP.
The expiratory time must be equal to at least three to five expiratory time constants for the patient to exhale and minimize or prevent AutoPEEP [6,7].
If the airway resistance or compliance increases, the expiratory time constant will increase, and more time will
be required for complete exhalation and to prevent AutoPEEP.If airway resistance or pulmonary compliance decreases, the expiratory time constant will decrease and it will take less time for complete exhalation to prevent AutoPEEP.
6. Inspiratory pressure on PC-CMV
During PC-CMV, the manner in which the clinician sets the inspiratory pressure (PI) varies depending upon the specific ventilator used. [See the rest of this paragraph for details. And consult your ventilator’s operations manual.]
The average alveolar pressure is estimated as the plateau pressure (Pplat) during a 0.5–2.0 s inspiratory hold.
It is recommended to monitor and keep the Pplat <25–30 cm H2O in all ventilated patients in traditional “lung protective strategy”.
In addition to monitoring the absolute number of Pplat, increasing evidence is being published emphasizing the
importance of targeting a Pplat – PEEP (ΔP) of <16 cm H2O, especially in patients with severe ARDS.It has been shown that if the ΔP is >16 cm H2O in patients with severe ARDS, the relative risk of death increases [8].
Thus, permitting a low tidal volume, even <6 ml/kg, to keep
ΔP <16 cm H2O as long as pH is acceptable, seems a reasonable practice.When a patient has an increased inspiratory effort, the pleural pressure (Ppl) becomes more negative. Clinically, we can estimate the pleural pressure by monitoring the esophageal pressure (Pes) [with an esophageal balloon placed in the distal third of the esophagus].
A value that is sometimes used clinically is referred to as the
transpulmonary pressure (PL).The transpulmonary pressure is the average alveolar pressure minus the pleural pressure (Ppl), and is reflective of the amount of strain on the lung.
Care should be taken to not allow the patient in PC-CMV to breathe with a strong inspiratory effort as the transpulmonary pressure will increase.
During PC-CMV without spontaneous breathing, if Pplat – PEEP (ΔP) remains constant, as compliance decreases, exhaled tidal volume will decrease. Similarly, as compliance increases, exhaled tidal volume will increase.
7. Initial ventilator settings when beginning PC-CMV
When initiating PC-CMV, although the settings below are frequently used, it is very important to individualize patients by evaluating the VTE, Pplat, SpO2 and graphic waveforms soon after initiating PC-CMV. Even though the tidal volume is not set directly, it is important to consider the milliliters per kilogram (ml/kg) of tidal volume in relation to the predicted body weight (PBW). Current recommendations are to keep tidal volume no >6–8 ml/kg PBW, unless the patient has ARDS, in which case the recommended tidal volume should be 4–6 ml/kg PBW.
Arterial blood gasses (ABGs) should be drawn and evaluated. Ventilator changes to achieve a target PaCO2 are described below.Mode: PC-CMV
PI: 5–10 cm H2O
TI: 0.7–1.0 s
f: 10–20 BPM
FIO2: 0.5
PEEP: 5–10 cm H2O8. Understanding the basic ventilator graphics to guide decisions
An understanding of the use of graphic analysis during mechanical ventilation is a key in managing patients receiving ventilatory support. The importance of evaluating the pressure-versus-time and the flow-versus-time waveforms will be discussed in depth below.
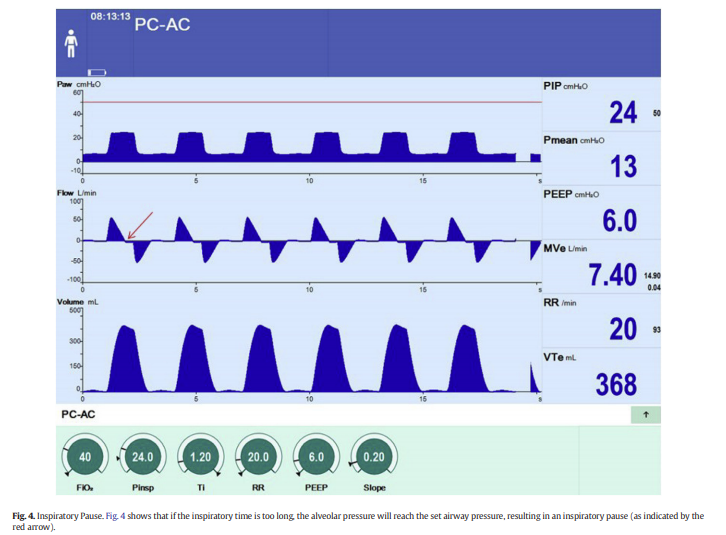
8.1. Pressure versus time waveform
Fig. 1 is an example of a typical waveform of a patient ventilated in PC-CMV. In this example, PIP 24 cm H2O, TI 0.9 s, f 20/min, PEEP 6.0 cm H2O, Slope 0.20 s. The pressure-versus-time waveform (Fig. 1, Top Waveform) shows that at the beginning of inspiration, the ventilator increases the airway pressure from the PEEP level of 6 cm H2O up to the set PIP of 24 cm H2O; the time to reach this PIP is set with the slope and in this case, it is set at 0.20 s. Inspiration continues until the set inspiratory time of 0.90 s has been reached. At that time, inspiration ends
and the patient is allowed to exhale back to the PEEP level of 6 cm H2O.8.2. Flow versus time waveform
On a typical flow-versus-time graphic display, inspiratory flow is demarcated above the horizontal baseline and expiratory flow is noted below that baseline. When looking at the flow-versus-time waveform (Fig. 1, Middle Waveform) the flowrate increases immediately at the beginning of inspiration and then gradually decreases throughout inspiration. Generally, the flow-versus-time waveform will be decelerating during PC-CMV. At the end of inspiration, the inspiratory valve closes
and the expiratory valve opens, allowing the patient to passively exhale.If the expiratory time is long enough, the patient will be able to exhale to baseline before the next breath begins, and there will be no AutoPEEP.
8.2.1. Inspiration
When using PC-CMV, the peak flowrate is dependent upon the Total PEEP, set PIP and Slope, as well as the patient’s airway resistance, pulmonary compliance, and effort. The difference between the PIP and the alveolar pressure is frequently referred to as the Delta PInsp (PIP – alveolar pressure). During inspiration, as the alveolar pressure increases, the Delta PInsp decreases (Fig. 2) [not included in excerpt], resulting in a decreasing inspiratory flowrate. If the inspiratory time is long enough for the alveolar pressure to equilibrate with the set pressure, the inspiratory flow waveform will return to baseline (Fig. 1, Middle Waveform). However, if the inspiratory time is not long enough for the alveolar pressure to reach the set pressure, the inspiratory flow waveform will not return to baseline. This generally results in a lower alveolar pressure and a reduced tidal volume (Fig. 3, Middle Waveform).
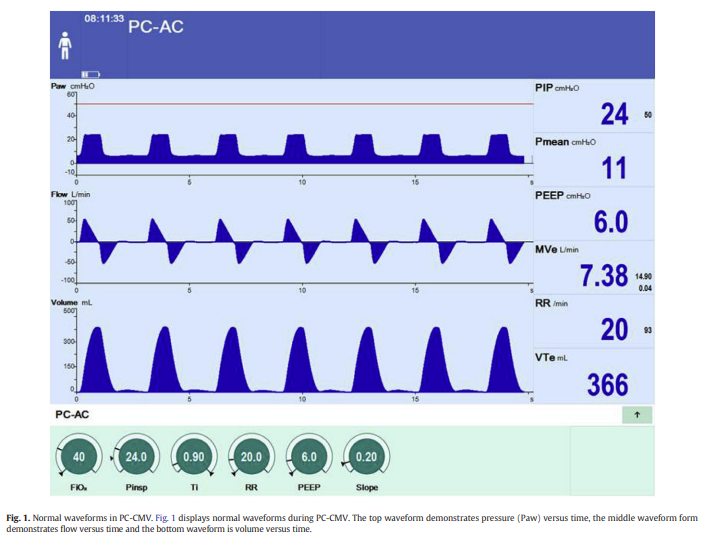
If the inspiratory time continues after the inspiratory flow has returned to the zero-flow baseline, an inspiratory pause will occur (Fig. 4, Middle Waveform).
8.2.2. Exhalation
If the expiratory time is long enough for the expiratory flowrate to return to the zero-flow baseline before the beginning of the next inspiration, there will be no AutoPEEP (Fig. 1, Middle Waveform).
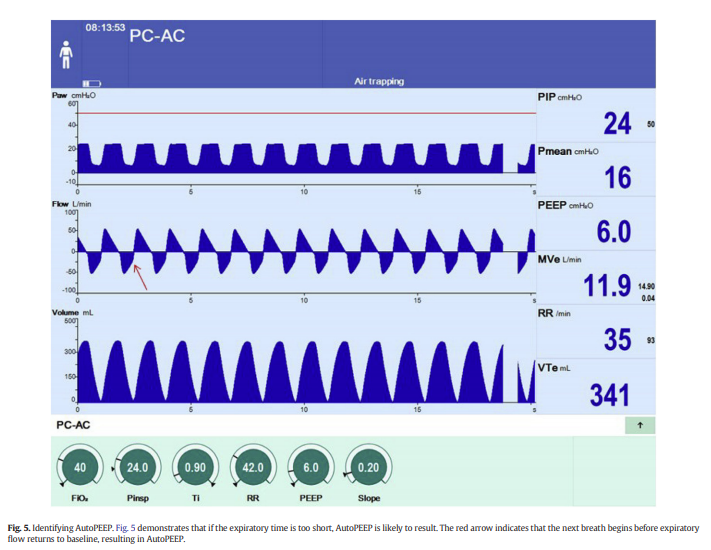
However, if the expiratory time* is too short and there is not enough time for the expiratory flowrate to return to baseline before the next breath begins, AutoPEEP is present (Fig. 5, Middle Waveform).
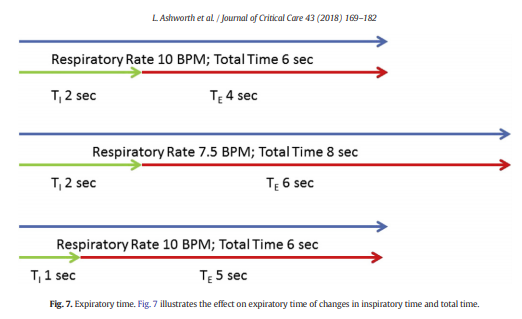
*The expiratory time is not directly set but rather is the result of the inspiratory time and of the respiratory rate.
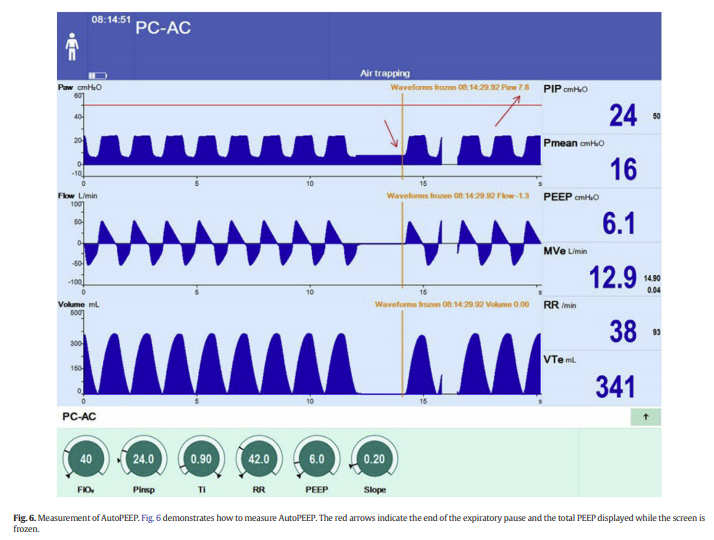
When ventilating a patient in PC-CMV, the presence of AutoPEEP will reduce the actual Delta PInsp by the amount of the AutoPEEP. For example, if the PIP is set at 24 cm H2O, and the PEEP at 6 cm H2O, and AutoPEEP is 0 cm H2O, the Delta PInsp will equal 24 cm H2O – 6 cm H2O = 18 cm H2O. However, if the patient has a Total PEEP 7.8 cm H2O, but the set PEEP is 6 cm H2O, AutoPEEP is present and can be calculated as 7.8 cm H2O (TotalPEEP) – 6 cm H2O (set PEEP) = 1.8 cm
H2O (AutoPEEP). This means that the alveoli are actually starting at 7.8 cm H2O (Total PEEP) rather than 6 cm H2O (PEEP), which results in a reduction in the Delta PInsp by 1.8 cm H2O, resulting in an overall decrease in delivered tidal volume (Fig. 6).
During PC-CMV, if AutoPEEP exists and is subsequently reduced
(e.g. a reduction in airway resistance after delivery of an inhaled bronchodilator), the Delta PInsp will increase. This usually results in an increase in delivered tidal volume. Options to reduce the AutoPEEP in PC-CMV include decreasing airway resistance and/or increasing expiratory time. Expiratory time can be increased by decreasing respiratory rate and/or decreasing inspiratory time (Fig. 7).
However, it is important to make sure that a decrease in respiratory rate does not result in a decreased minute ventilation, especially in a spontaneously breathing patient. Similarly, tidal volume must be monitored carefully as a decrease in inspiratory time may result in a decreased tidal volume.
9. Making changes: an algorithmic approach
9.1.1. Initial decision
When a patient has an elevated PaCO2 resulting in a respiratory acidosis, and the decision is made to reduce the PaCO2, one must either deliver a larger tidal volume or increase the respiratory rate. In cases where ventilator induced lung injury is a concern, clinicians may choose to not increase the tidal volume.
When evaluating acid-base status, the first decision that has to be made is whether or not the PaCO2 is high enough and/or the pH is low enough to necessitate a reduction in PaCO2. If the PaCO2 is not > 50–70 Torr and the pH is not < 7.25, the decision may be made to maintain current therapy. However, if there is a need to reduce PaCO2, the next decision is whether or not to increase minute ventilation by changing ventilator settings or to utilize other, non-ventilator strategies to decrease the PaCO2 (Fig. 8)
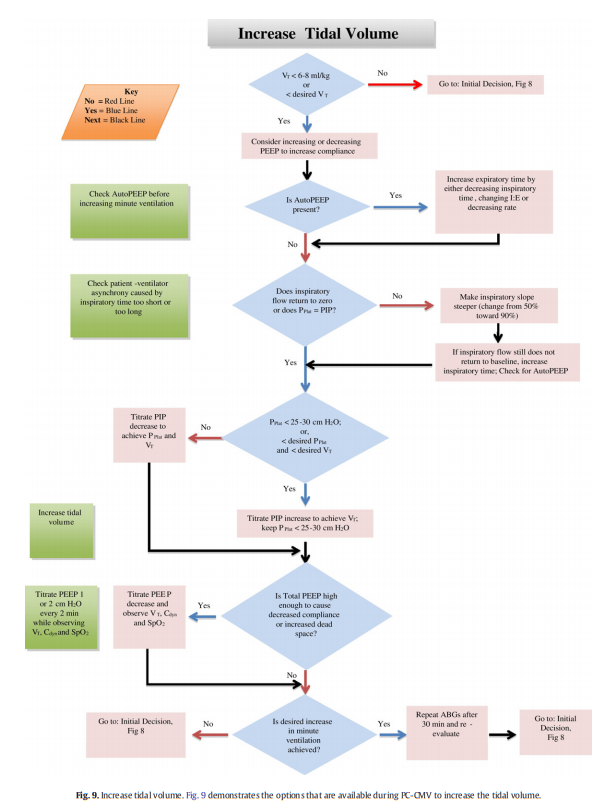
If the decision is made to change the ventilatory setting to increase the minute ventilation, the Pplat and tidal
volume must first be evaluated. If the Pplat is < 25–30 cm H2O (or less than the desired Pplat), or if the tidal volume is < 6–8 ml/kg PBW, and if the desired outcome is an increase in tidal volume, then options to increase tidal volume should be considered (Fig. 9).
If the decision is made to not increase the tidal volume, then options to increase respiratory rate should be considered (Fig. 10)
Fig10
If the decision is made to not increase tidal volume or respiratory rate, then non-ventilatory strategies
should be considered (Fig. 11).
Fig 11
9.1.2. Increasing tidal volume
When a decision is made to increase the tidal volume, there are
many options to consider. As illustrated in Fig. 9, increasing the PIP should not be considered the default option. As discussed earlier, if the patient has low compliance, PC-CMV will result in a decreased tidal volume at a given pressure. Consideration should be given to try to increase the compliance by either increasing the PEEP level if it is too low (potentially causing atelectasis), or by decreasing the PEEP level if it is too high
(potentially resulting in overdistension), as both of these issues can result in a low compliance.As previously described, AutoPEEP will reduce the effective Delta Insp. Evaluating the patient for AutoPEEP should be part of the ongoing patient assessment. If the patient has AutoPEEP, methods to decrease the AutoPEEP should be considered. Such considerations include decreasing the airway resistance, increasing expiratory time by decreasing inspiratory time, prolonging the expiratory time by changing the I:E, and/or decreasing the respiratory rate.
The inspiratory flow waveform should be a major part of both routine and continual patient assessments. Throughout inspiration, as the alveolar pressure increases, the inspiratory flow will return closer to baseline. If the inspiratory flow does not return to baseline, an increase in inspiratory time will generally result in an increased tidal volume and should be considered as long as increasing inspiratory time does not result in shortening expiratory time, causing AutoPEEP, or result in patient-ventilator asynchrony. When the inspiratory flow waveform does not return to baseline, the Pplat will be less than the set PIP. When adjusting the inspiratory time, it is important to re-assess the Pplat and evaluate the patient-ventilator asynchrony that could be caused by the inspiratory time being too short or too long.
The next step in a complete assessment is to evaluate the Pplat. If the Pplat is b25–30 cm H2O, or less than the desired Pplat, and the tidal volume is less than the desired tidal volume, PIP should be increased gradually to achieve the desired tidal volume, ensuring that the Pplat is < 25–30 cm H2O.
If the Total PEEP is too high, it may lead to overdistension of alveoli. This will generally result in a decrease in compliance and potentially an increase in alveolar dead space due to stretching of the alveoli and compression of the pulmonary capillaries. This causes reduced perfusion to the over-distended alveoli and an increase in the ventilation/perfusion ratio, which may increase the dead space and result in an increased PaCO2. A decremental PEEP trial involves decreasing the set
PEEP 1 or 2 cm H2O every one to two minutes while monitoring the dynamic compliance (Cdyn), tidal volume, and SpO2. If the Total PEEP was too high, as the set PEEP is decreased, the Cdyn will increase. The optimal PEEP level can be identified as the point at which the highest Cdyn occurred. The set PEEP level should be set 2–3 cm H2O above this point [6,10].Start at next paragraph at top of p177. But first insert fig10 and fig11 above.