In this post I link to and excerpt from Episode 85 – Medical Clearance of the Psychiatric Patient. Written Summary and blog post by Anton Helman Aug 2016 with background research by Anton Nikouline.
In addition, in the body of the post, I have excerpted from Best Case Ever 48 – Organic vs Psychiatric Illness. Published August 2016 by Anton Helman in the body of the post.
Here are excerpts:
Psychiatric chief complaints comprise about 6 or 7% of all ED visits, with the numbers of psychiatric patients we see increasing every year. The ED serves as both the lifeline and the gateway to psychiatric care for millions of patients suffering from acute behavioural or psychiatric emergencies. As ED docs, besides assessing the risk of suicide and homicide, one of the most important jobs we have is to determine whether the patient’s psychiatric or behavioral emergency is the result of an organic disease process, as opposed to a psychological one.
There is no standard process for this.
Factors favouring psychiatric illness
- history of psychiatric illness
- younger age
- onset over weeks to months
Factors favouring organic illness
- no history of psychiatric illness
- older age (>40)
- onset over hours-days
- complaint of headache
- any recent new medication
A study out of the Annals of EM showed that The Quick Confusion Scale is as reliable as a full Mini-Mental Status Exam to reveal an altered level of awareness that may help pick up organic pathology:
The Quick Confusion Scale
What month is it?
Repeat phrase and remember it: “John Brown, 42 Market Street, New York”
About what time is it?
Count backward from 20 to 1
Say the months in reverse
Repeat the memory phrase
The 3 key elements of the mental status exam are orientation, memory and judgement which can often be gleaned from the patient encounter by an experienced EM provider without a validated scale.
Physical Exam Clues to Differentiate Organic vs Psychiatric Illness
As always, vital signs are vital! Any abnormality in vital signs should be addressed and accounted for.
Hypoglycemia can mimic many psychiatric illnesses from catatonic schizophrenia to severe depression as should be considered as “the 6th vital sign”.
Blood glucose (ABC Don’t Ever Forget Glucose)
Look for fluctuating level of awareness as it is rare in isolated psychiatric illness, and often signifies delirium and an underlying toxin, metabolic abnormality or CNS lesion.
Scrutinize the patient’s eyes – any abnormality in gaze, nystagmus, pupillary dilation etc may signify an organic pathology.
____________________________________________________
What follows is from Best Case Ever 48 – Organic vs Psychiatric Illness. Published August 2016 by Anton Helman
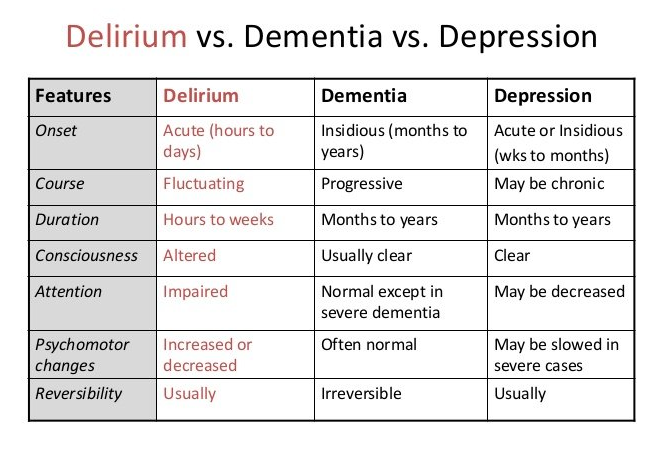
Differentiating Delirium, Dementia & Depression in Organic vs Psychiatric Illness
Delirium is the acute and fluctuating onset of in-attention, with disorganized thinking, and/or altered level of awareness. Unlike dementia (which progresses slowly) delirium happens acutely. In the elderly, 70% of delirium is initially “hypoactive,” which can delay its detection in the ED.
Delirium is a very serious presentation, which always has an underlying medical cause. Length of stay in hospital, and in-hospital mortality increases twofold in patients diagnosed with delirium, and delirium is not always reversible. Always assess the baseline functional status of elderly patients, and be suspicious of any acute decline.
Visual vs Auditory Hallucinations
Generally speaking, auditory hallucinations are more indicative of a psychiatric illness where as visual hallucinations are more indicative of an organic illness. While about 15% of patients with schizophrenia are said to experience visual hallucinations, these tend to occur in those schizophrenics with severe illness in addition to auditory hallucinations.
Visual hallucinations can occur in a myriad of organic illnesses and ingestions from LSD to Creutzfeldt-Jakob disease to Delirium Tremens to (my favourite) Anton’s Syndrome.
________________________________________________________
Resuming excerpts from Episode 85 – Medical Clearance of the Psychiatric Patient.
Visual hallucinations usually point to an organic illness. Generally speaking, auditory hallucinations are more indicative of a psychiatric illness whereas visual hallucinations are more indicative of an organic illness. While about 15% of patients with schizophrenia are said to experience visual hallucinations, these tend to occur in those schizophrenics with severe illness in addition to auditory hallucinations.
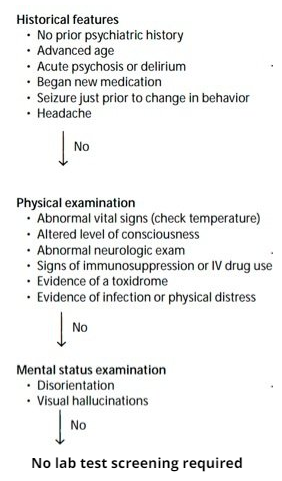
Which Psychiatric Patients Require Screening Lab Tests or CT Scan of the Head
CT is clinically indicated in psychiatric patients with altered mental status, trauma, immunodeficiency, or focal neurological findings.
Urine drug screens are not required routinely in the psychiatric patient. Most patients, if asked in a non-accusatory manner, will tell you what drugs they have recently taken. Olshaker found that the reliability of patient self-reported drug use had a sensitivity of 92% and specificity of 91%. The reliability of self-reported alcohol use was 96% sensitive and 87% specific. In addition, urine drug screens have many false positive and negatives which can be misleading.