In this post I link to and excerpt from Emergency Medicine Cases’ Episode 87 – Alcohol Withdrawal and Delirium Tremens: Diagnosis and Management. Written Summary and blog post written by Keerat Grewal, edited by Anton Helman October, 2016
Note to myself: As always at the time of managing a patient with potential alcohol withdrawal or delirium tremens, it is best to review the entire written summary. The notes I post are simply to help me fix important points in my memory.
Here are excerpts:
Timing of Alcohol Withdrawal and Delirium Tremens
Symptoms from alcohol withdrawal usually start within 6-8 hours after the blood alcohol level decreases, peak at 72 hours, and diminish by days 5 to 7 of abstinence. Delirium Tremens can occur anytime from 3 to 12 days after abstinence.
Patients who are severely dependent on alcohol become tolerant to alcohol and their nervous systems have been reset to compensate for the sedating effects of alcohol. The likelihood of developing withdrawal is dependent on the usual amount consumed and the duration of consumption. Therefore, patients who consume large amounts of alcohol on a regular basis are more likely to develop withdrawal requiring pharmacologic management compared to those who binge sporadically.
Ethanol Level in patients with alcohol withdrawal
A serum ethanol level should be considered only if the history is inconsistent or you are unsure of the diagnosis. Even then, there is no single ethanol level at which withdrawal is impossible. Chronic alcohol users may experience alcohol withdrawal at serum ethanol levels that are intoxicating to the naïve drinker.
ECG in patients with alcohol withdrawal
There is some evidence to suggest that patients in severe alcohol withdrawal are at risk for prolonged QT which may be at least partially a result of the associated electrolyte abnormality such as hypomagnesemia. Consider a baseline ECG in patients who require admission for alcohol withdrawal.
Differential Diagnosis of Alcohol Withdrawal and Delirium Tremens
First, some patients with alcohol intoxication can have some of the signs of alcohol withdrawal (tachycardia, elevated BP, diaphoresis, agitation), so assuming that they are in withdrawal and giving them high doses of benzodiazepines can lead to complications of oversedation. Be sure to examine for tremor carefully. If they don’t have a true withdrawal tremor then they are probably drunk and not in withdrawal.
Pitfall: Some patients with alcohol intoxication can have some of the signs of alcohol withdrawal (tachycardia, elevated BP, diaphoresis, agitation), and assuming that they are in withdrawal and giving them high doses of benzodiazepines can lead to complications of oversedation.
Next, it is important to complete a neurological exam and look for any signs of head injury in patients with alcohol intoxication or withdrawal. Patients with a history of alcohol abuse are at a higher risk for head injury and intracranial hemorrhage as many of them have coagulopathies related to liver disease and fragile intracranial bridging veins from cerebral atrophy. Have a low threshold to obtain a CT head to rule out a bleed if there are signs or suspicion of a head injury.
In patients who are suffering from delirium, keep a broad differential diagnosis including infection, other toxidromes (sympathomimetics, anticholinergics, toxic alcohols), serotonin syndrome, NMS, hypertensive crisis, acute pain and thyrotoxicosis.
Pharmacologic Treatment of Patients with Alcohol Withdrawal
Benzodiazepines for Alcohol Withdrawal
The first line medication for treating patients with alcohol withdrawal is benzodiazepines. The drug of choice is diazepam because it has a long half-life of ~100 hours, and carries a decreased risk of developing serious withdrawal symptoms once the patient is discharged. Diazepam also has a faster onset of action than lorazepam. It is important to remember that diazepam should be avoided in patients with overt liver failure or a history of liver failure.
Use oral benzodiazepines in stable patients with mild withdrawal who are not vomiting. Use IV benzodiazepines allowing faster onset and easier titration in patients with severe withdrawal as these patients are at a higher risk of seizure.
Dosing of Benzodiazepines in Alcohol Withdrawal
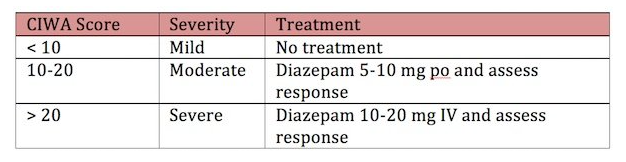
Dose benzodiazepines according to the severity of the alcohol withdrawal:
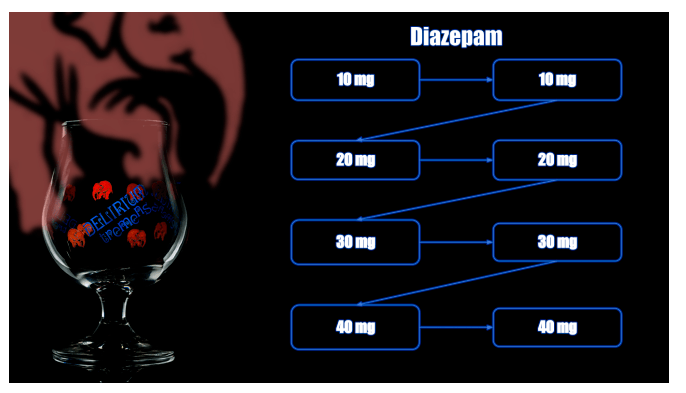
Another protocol to consider for patients with severe withdrawal is to give a first dose of diazepam 10mg IV, and repeat in 5 minutes if the response is not adequate. Then double the dose to 20 mg and continue with 20mg, 30mg, 30mg, 40mg, 40mg every 5 minutes as needed.
Example [above] diazepam dosing guide for severe withdrawal (from Management of Delirium Tremens from First 10EM)
The CIWA protocol is a 10-item scale. It has been well validated in patients with alcohol withdrawal, but should not be used for patients with delirium tremens. The CIWA calls for patients to be assessed hourly and treated if the total score is 10 or greater. When 2 sequential scores are < 10 they may be considered for discharge.
CIWA on MDCalc Here
Observational studies show that patients are often either undertreated resulting in complications of alcohol withdrawal such as seizures and delirium tremens, or oversedated leading to prolonged length of stay and airway complications. If a patient has two sequential CIWA scores < 10 two hours apart, and there are no concerning risks for deterioration, consider discharging the patient from the ED. The patient’s tremor should be minimal or resolved before discharge regardless of the CIWA score.
Pitfall: Patients with a CIWA score <10 yet still have a severe alcohol withdrawal tremor are at risk of complications of alcohol withdrawal if discharged from the ED.
The CIWA-Ar is only intended to allow assessment of withdrawal severity once the diagnosis has been made. It is not a diagnostic test for withdrawal.
It is strongly discouraged that patients be provided a take-away supply or prescription for benzodiazepines. The long half-life of diazepam will protect patients from developing serious symptoms of withdrawal, and if adequately treated in the ED, no additional medications will be required.