Today, I review, link to and excerpt from Quantification and treatment of congestion in heart failure: A clinical and pathophysiological overview. [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Nefrologia (Engl Ed). 2021 Jul 18:S0211-6995(21)00114-4. doi: 10.1016/j.nefro.2021.04.006. Online ahead of print.
All that follows is from the above resource.
ABSTRACTRenal sodium and water retention with resulting extracellular volume expansion and redistribution are hallmark features of heart failure syndromes. However, congestion assessment, monitoring, and treatment represent a real challenge in daily clinical practice. This document reviewed historical and contemporary evidence of available methods for determining volume status and discuss pharmacological aspects and pathophysiological principles that underlie diuretic use.
Keywords: Heart failure Congestion Diuretic therapy BiomarkersKey concepts
The relevance of this review is based on:
- Congestion is a key pathophysiological phenomenon largely responsible for the clinical manifestations and morbidity and mortality associated with heart failure.
- Limited diagnostic performance of classic symptoms and signs in the assessment of congestion.
- Poor understanding of the complex pathophysiology of congestion, a fact that explains the great variability in this regard.
- Largely empirical therapeutic approach. In this sense, and from a pathophysiological and clinical point of view, we propose a detailed and updated review of the different agents and therapeutic strategies used.
- The increasingly prevalent role of cardiorenal syndrome.
Introduction
Heart failure (HF) is an increasing public health problem. The incidence, prevalence and, morbidity and mortality associated with this syndrome is high and constitutes the paradigm of the chronic patient who suffers from frequent decompensations.1 Most of these decompensations are attributable to congestion.2 In this scenario, diuretics are the mainstay of treatment.3 However, there is great uncertainty about how, how much and where to administer the diuretics.
The objective of this document is to inquire into clinical, pathophysiological and pharmacological aspects from an integrating perspective that contributes to a better understanding of congestion and the optimization of its treatment.
Diagnosis and characterization of congestion in HF
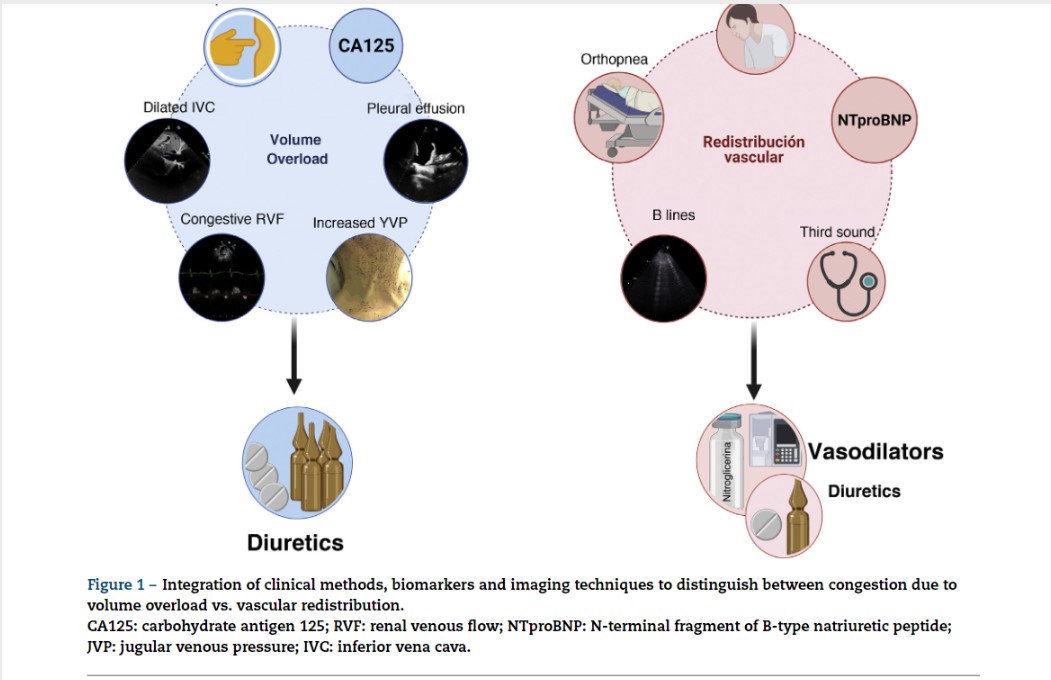
In HF, congestion is defined as the accumulation of fluid in the intravascular and extravacular compartment as a result of increased filling pressures. However, congestion is not a synonymous of volume overload.4 The concept of vascular redistribution suggests that increased venous tone (due to neurohormonal activation, myocardial ischemia, hypertensive episodes, medication changes, etc.) can precipitate a rapid redistribution of fluid from a peripheral venous reservoir (e.g., splanchnic bed) to the central cardiopulmonary circulation, increasing the intravascular hydrostatic pressure without increasing total blood volume.5 In this scenario, vasodilator therapy could be more appropriate than aggressive diuretic intervention (Fig. 1). In contrast, volume overload is a more latent phenomenon that results from the avidity of sodium and water in the renal tubule, and from the imbalance between the hydrostatic and oncotic pressures of the intravascular and interstitial compartment.6 Although most patients with decompensated HF present a combination of both, congestion and volume overload, identifying the predominant phenotype will determine the most appropriate therapeutic strategy (Fig. 1). It is noteworthy that the traditional symptoms and signs to assess congestion offer a limited diagnostic accuracy for the characterization and quantification of its severity.7,8