In this post I link to and excerpt from the Infectious Diseases Society of America (ISDA) “IDSA Guidelines on the Treatment and Management of Patients with COVID-19“, Published by IDSA on 4/11/2020. Last updated, 4/5/2021.
Here is the citation:
Bhimraj A, Morgan RL, Shumaker AH, Lavergne V, Baden L, Cheng VC, Edwards KM, Gandhi R, Gallagher J, Muller WJ, O’Horo JC, Shoham S, Murad MH, Mustafa RA, Sultan S, Falck-Ytter Y. Infectious Diseases Society of America Guidelines on the Treatment and Management of Patients with COVID-19. Infectious Diseases Society of America 2021; Version 4.1.2. Available at https://www.idsociety.org/practice-guideline/covid-19-guideline-treatment-and-management/. Accessed 25/04/2021.
The practice guideline definitions:
*Critical illness is defined as patients on mechanical ventilation and extracorporeal mechanical oxygenation (ECMO). Critical illness includes end organ dysfunction as is seen in sepsis/septic shock. In COVID-19, the most commonly reported form of end organ dysfunction is ARDS
**Severe illness is defined as patients with SpO2 ≤94% on room air, including patients on supplemental oxygen.
***Non-severe illness is defined as patient with a SpO2 > 94% not requiring supplemental oxygen.
Note to myself: The following recommendation should be kept in mind –
Recommendation 13: Among ambulatory patients with mild to moderate COVID-19 at high risk for progression to severe disease, the IDSA guideline panel suggests bamlanivimab/etesevimab rather than no bamlanivimab/etesevimab. (Conditional recommendation, low certainty of evidence)
• Remarks:
o Patients with mild to moderate COVID-19 who are at high risk of progression to
severe disease admitted to the hospital for reasons other than COVID-19 may also
receive bamlanivimab/etesevimab.
o For patients at high risk for progression to severe disease, the data are strongest for
bamlanivimab/etesevimab. Bamlanivimab monotherapy or casirivimab/imdevimab
may have similar clinical benefit, but data are more limited.
o There are limited data on efficacy of bamlanivimab/etesevimab in high-risk patients
between 12 and 18 years of age.High risk is defined as patients who meet at least one of the following criteria:
• Have a body mass index (BMI) ≥35
• Have chronic kidney disease
• Have diabetes
• Have immunosuppressive disease
• Are currently receiving immunosuppressive treatment
• Are ≥65 years of age
• Are ≥55 years of age AND haveo cardiovascular disease, OR
o hypertension, OR
o chronic obstructive pulmonary disease/other chronic respiratory disease.• Are 12 – 17 years of age AND have
o BMI ≥85th percentile for their age and gender based on CDC growth charts, OR
o sickle cell disease, OR
o congenital or acquired heart disease, OR
o neurodevelopmental disorders, for example, cerebral palsy, OR
o a medical-related technological dependence, for example, tracheostomy,
gastrostomy, or positive pressure ventilation (not related to COVID-19), OR
o asthma, reactive airway or other chronic respiratory disease that requires daily
medication for control.a. These criteria refer to Recommendation 13 (the use of bamlanivimab/etesevimab in ambulatory patients with COVID-19).
Reference
1. U.S. Food and Drug Administration. Fact Sheet for Health Care Providers: Emergency
Use Authorization (EUA) of Bamlanivimab and Etesevimab. Available at:
https://www.fda.gov/media/145802/download. Accessed 25 February 2021.
Here is the Abstract:
Background: There are many pharmacologic therapies that are being used or considered for treatment of coronavirus disease 2019 (COVID-19). There is a need for frequently updated practice guidelines on their use, based on critical evaluation of rapidly emerging literature.
Objective: There are many pharmacologic therapies that are being used or considered for treatment of coronavirus disease 2019 (COVID-19). There is a need for frequently updated practice guidelines on their use, based on critical evaluation of rapidly emerging literature.
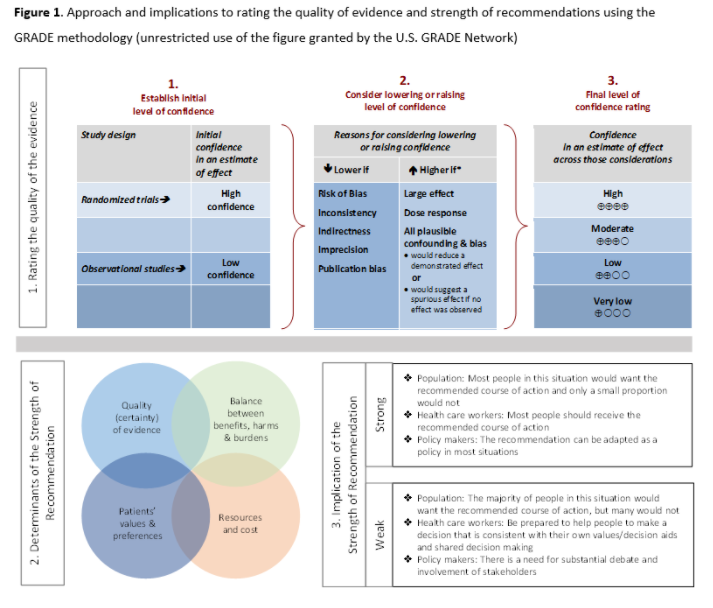
Methods: In March 2020, the Infectious Diseases Society of America (IDSA) formed a multidisciplinary guideline panel of infectious disease clinicians, pharmacists, and methodologists with varied areas of expertise. The process followed a rapid recommendation checklist. The panel prioritized questions and outcomes. Then a systematic review of the peer-reviewed and grey literature was conducted. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was used to assess the certainty of evidence and make recommendations.
Results: On April 11, 2020, IDSA released online initial treatment recommendations and narrative summaries of other treatments under evaluation. Since that time, the guideline panel and methodologists have continued to monitor the literature and issue updates and addendums to these guidelines in response to evolving research.
Conclusions: Since the inception of its work, the panel has expressed the overarching goal that patients be recruited into ongoing trials, which would provide much needed evidence on the efficacy and safety of various therapies for COVID-19, given that we could not make a determination whether the benefits outweigh harms for most treatments.
Keywords: coronavirus, SARS-CoV-2, COVID, COVID-19, pneumonia
Here is a link to Download the PDF.
COVID-19 Guideline, Part 2: Infection Prevention
COVID-19 Guideline, Part 3: Diagnostics
COVID-19 Guideline, Part 4: Serology
April 5, 2021
Version 4.1.2 has been released and contains a revision to the number of studies included in Table 9 in the section on remdesivir.
Executive Summary and Background
Executive Summary
Coronavirus disease 2019 (COVID-19) is a pandemic with a rapidly increasing incidence of infections and deaths. Many pharmacologic therapies are being used or considered for treatment. Given the rapidity of emerging literature, the Infectious Diseases Society of America (IDSA) identified the need to develop living, frequently updated evidence-based guidelines to support patients, clinicians and other health-care professionals in their decisions about treatment and management of patients with COVID-19.
Summarized below are the recommendations with comments related to the clinical practice guideline for the treatment and management of COVID-19. A detailed description of background, methods, evidence summary and rationale that support each recommendation, and research needs can be found online in the full text. In brief, per Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology, recommendations are labeled as “strong” or “conditional”. The word “recommend” indicates strong recommendations and “suggest” indicates conditional recommendations. In situations where promising interventions were judged to have insufficient evidence of benefit to support their use and with potential appreciable harms or costs, the expert panel recommended their use in the context of a clinical trial. These recommendations acknowledge the current “knowledge gap” and aim at avoiding premature favorable recommendations for potentially ineffective or harmful interventions.
- Recommendation 1: Among patients with COVID-19, the IDSA guideline panel recommends against hydroxychloroquine. (Strong recommendation, Moderate certainty of evidence)
- Remark: Chloroquine is considered to be class equivalent to hydroxychloroquine.
- Recommendation 2: Among hospitalized patients with COVID-19, the IDSA guideline panel recommends against hydroxychloroquine plus azithromycin. (Strong recommendation, Low certainty of evidence)
- Remark: Chloroquine is considered to be class equivalent to hydroxychloroquine
- Recommendation 3: Among hospitalized patients with COVID-19, the IDSA guideline panel recommends against the use of the combination lopinavir/ritonavir. (Strong recommendation, Moderate certainty of evidence)
- Recommendation 4: Among hospitalized critically ill patients* with COVID-19, the IDSA guideline panel recommends dexamethasone rather than no dexamethasone. (Strong recommendation, Moderate certainty of evidence)
- Remark: If dexamethasone is unavailable, equivalent total daily doses of alternative glucocorticoids may be used. Dexamethasone 6mg IV or PO for 10 days (or until discharge) or equivalent glucocorticoid dose may be substituted if dexamethasone unavailable. Equivalent total daily doses of alternative glucocorticoids to dexamethasone 6 mg daily are methylprednisolone 32 mg and prednisone 40 mg.
- *Critical illness is defined as patients on mechanical ventilation and ECMO. Critical illness includes end organ dysfunction as is seen in sepsis/septic shock. In COVID-19, the most commonly reported form of end organ dysfunction is ARDS
- Recommendation 5: Among hospitalized patients with severe**, but non-critical, COVID-19, the IDSA guideline panel suggests dexamethasone rather than no dexamethasone. (Conditional recommendation, Moderate certainty of evidence)
- Remark: Dexamethasone 6 mg IV or PO for 10 days (or until discharge) or equivalent glucocorticoid dose may be substituted if dexamethasone unavailable. Equivalent total daily doses of alternative glucocorticoids to dexamethasone 6 mg daily are methylprednisolone 32 mg and prednisone 40 mg.
- **Severe illness is defined as patients with SpO2 ≤94% on room air, including patients on supplemental oxygen.
- Recommendation 6: Among hospitalized patients with non-severe*** COVID-19 without hypoxemia requiring supplemental oxygen, the IDSA guideline panel suggests against the use of glucocorticoids. (Conditional recommendation, Low certainty of evidence)
- ***Non-severe illness is defined as patient with a SpO2 > 94% not requiring supplemental oxygen.
- Recommendation 7: Among hospitalized adults with progressive severe* or critical** COVID-19 who have elevated markers of systemic inflammation, the IDSA guideline panel suggests tocilizumab in addition to standard of care (i.e., steroids) rather than standard of care alone. (Conditional recommendation, Low certainty of evidence)
- Remarks:
- Patients, particularly those who respond to steroids alone, who put a high value on avoiding possible adverse events of tocilizumab and a low value on the uncertain mortality reduction, would reasonably decline tocilizumab.
- In the largest trial on the treatment of tocilizumab, criterion for systemic inflammation was defined as CRP ≥75 mg/L.
Severity definitions:
- *Severe illness is defined as patients with SpO2 ≤94% on room air, including patients on supplemental oxygen.
- **Critical illness is defined as patients on mechanical ventilation and ECMO. Critical illness includes end organ dysfunction as is seen in sepsis/septic shock. In COVID-19, the most commonly reported form of end organ dysfunction is ARDS.
- Recommendation 8: Among patients who have been admitted to the hospital with COVID-19, the IDSA guideline panel recommends COVID-19 convalescent plasma only in the context of a clinical trial. (Knowledge gap)
- Recommendation 9: In hospitalized patients with severe* COVID-19, the IDSA panel suggests remdesivir over no antiviral treatment. (Conditional recommendation, Moderate certainty of evidence)
- Remark: For consideration in contingency or crisis capacity settings (i.e., limited remdesivir supply): Remdesivir appears to demonstrate the most benefit in those with severe COVID-19 on supplemental oxygen rather than in patients on mechanical ventilation or ECMO.
- *Severe illness is defined as patients with SpO2 ≤94% on room air, and those who require supplemental oxygen, mechanical ventilation, or ECMO.
- Recommendation 10: In patients on supplemental oxygen but not on mechanical ventilation or ECMO, the IDSA panel suggests treatment with five days of remdesivir rather than 10 days of remdesivir. (Conditional recommendation, Low certainty of evidence)
- Remark: In patients on mechanical ventilation or ECMO, the duration of treatment can be 10 days.
- Recommendation 11: In patients with COVID-19 admitted to the hospital without the need for supplemental oxygen and oxygen saturation >94% on room air, the IDSA panel suggests against the routine use of remdesivir. (Conditional recommendation, Very low certainty of evidence)
- Recommendation 12: Among hospitalized patients with severe COVID-19, the IDSA panel suggests against famotidine use for the sole purpose of treating COVID-19 outside of the context of a clinical trial. (Conditional recommendation, very low certainty of evidence)
- Recommendation 13: Among ambulatory patients with mild to moderate COVID-19 at high risk for progression to severe disease, the IDSA guideline panel suggests bamlanivimab/etesevimab rather than no bamlanivimab/etesevimab. (Conditional recommendation, low certainty of evidence)
- Remarks:
- Patients with mild to moderate COVID-19 who are at high risk of progression to severe disease admitted to the hospital for reasons other than COVID-19 may also receive bamlanivimab/etesevimab.
- For patients at high risk for progression to severe disease, the data are strongest for bamlanivimab/etesevimab. Bamlanivimab monotherapy or casirivimab/imdevimab may have similar clinical benefit, but data are more limited.
- There are limited data on efficacy of bamlanivimab/etesevimab in high-risk patients between 12 and 18 years of age.
- Recommendation 14: Among hospitalized patients with severe COVID-19, the IDSA guideline panel recommends against bamlanivimab monotherapy. (Strong recommendation, Moderate certainty of evidence)
- Recommendation 15: Among hospitalized patients with severe* COVID-19 who cannot receive corticosteroids because of a contraindication, the IDSA guideline panel suggests use of baricitinib with remdesivir rather than remdesivir alone. (Conditional recommendation, Low certainty of evidence)
- Remark: Baricitinib 4 mg daily dose for 14 days (or until hospital discharge). The benefits of baricitinib plus remdesivir for persons on mechanical ventilation are uncertain. See the remdesivir section for dose and duration.
- Severe illness is defined as patients with SpO2 ≤94% on room air, including patients on supplemental oxygen, oxygen through a high-flow device, or non-invasive ventilation.
- Recommendation 16: Among hospitalized patients with COVID-19, the IDSA guideline panel recommends treatment with baricitinib plus remdesivir plus corticosteroids only in the context of a clinical trial. (Knowledge gap)
- Recommendation 17: In hospitalized patients with severe COVID-19, the IDSA panel suggests against ivermectin use outside of the context of a clinical trial. (Conditional recommendation, very low certainty of evidence)
- Recommendation 18: In outpatients with COVID-19, the IDSA panel suggests against ivermectin use outside of the context of a clinical trial. (Conditional recommendation, very low certainty of evidence)
Since the inception of its work, the panel has expressed the overarching goal that patients be recruited into ongoing trials, which would provide much needed evidence on the efficacy and safety of various therapies for COVID-19. The panel has determined that when an explicit trade-off between highly uncertain benefits and known putative harms of these therapeutic agents were considered, a net positive benefit was not reached and could possibly be negative (risk of excess harm). The panel acknowledges that enrolling patients in randomized controlled trials (RCTs) might not be feasible for many frontline providers due to limited access and infrastructure. Should lack of access to clinical trials exist, we encourage setting up local or collaborative registries to systematically evaluate the efficacy and safety of drugs to contribute to the knowledge base. Each clinician can play a role in advancing our understanding of this disease through a local registry or other data collection efforts.
Background
The first cases of COVID-19 were reported from Wuhan, China in early December 2019 [1], now known to be caused by a novel beta-coronavirus, named as Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Within a span of months, COVID-19 has become pandemic due to its transmissibility, spreading across continents with the number of cases and deaths rising daily [2]. Although most infected individuals exhibit a mild illness (80%+), 14% have serious and 5% have critical illness. Approximately 10% will require hospital admission due to COVID-19 pneumonia, of which approximately 10% will require ICU care, including invasive ventilation due to acute respiratory distress syndrome (ARDS) [3]. While mortality appears to be more common in older individuals and those with comorbidities, such as chronic lung disease, cardiovascular disease, hypertension and diabetes, young people with no comorbidities also appear to be at risk for critical illness including multi-organ failure and death.
There has been an expanding number of studies rapidly published online and in academic journals; however, some of these may be of limited quality and are pre-published without sufficient peer-review. Critical appraisal of the existing studies is needed to determine if the existing evidence is sufficient to support currently proposed management strategies.
Given the rapid global spread of SARS-CoV-2 and the difficulty for the overburdened front-line providers and policymakers to stay up to date on emerging literature, IDSA has recognized the necessity of developing a rapid guideline for the treatment of COVID-19. The guideline panel is using a methodologically rigorous process for evaluating the best available evidence and providing treatment recommendations. Two additional guidelines on diagnostic testing and infection prevention also have been developed. These guidelines will be frequently updated as substantive literature becomes available and are accessible on an easy to navigate web and device interface at https://www.idsociety.org/covid19guidelines.
There continue to be several ongoing trials evaluating therapeutic agents for the treatment of COVID-19. As data becomes available from these trials and if there is a preponderance of evidence to suggest the use of a therapeutic agent even in the context of clinical trials is no longer warranted it will be removed from future updates of the guideline (and the removal will be noted in the updated guidelines). If there is emerging evidence on the efficacy or safety of a therapeutic agent not mentioned in the current version of the guideline it will be included in future updates of the guideline.
These recommendations are intended to inform patients, clinicians, and other health professionals by providing the latest available evidence.