In this post I link to and excerpt from What is the efficacy and safety of rapid exercise tests for exertional desaturation in covid-19? [Full Text HTML] [Full Text PDF]. April 21, 2020, from The Centre for Evidence-Based Medicine.
Here are excerpts:
Abstract
Background
Even when resting pulse oximetry is normal in the patient with acute Covid-19, hypoxia can manifest on exertion. We sought to summarise the literature on the performance of different rapid tests for exertional desaturation.
Main research question
What tests have been formally evaluated for the rapid assessment of exertional hypoxia in patients with lung disease against a gold standard exercise test such as the 6MWT and CPET?
Method
AMED, CINAHL, EMBASE MEDLINE, Cochrane and PubMed using LitCovid, Scholar and Google databases were searched to September 2020. Studies where participants had Covid-19 or another lung disease and underwent any form of exercise test which was compared to a reference standard were eligible. Risk of bias was assessed using QUADAS 2. Heterogeneity of study design precluded meta-analysis.
Results
Of 47 relevant papers, 15 were empirical studies, of which 11 described an attempt to validate one or more exercise desaturation tests in lung diseases other than Covid-19. In all but one of these, methodological quality was poor or impossible to fully assess. None had been designed as a formal validation study (most used simple tests of correlation). Only one validation study (comparing a 1-minute sit-to-stand test [1MSTST] with the reference standard 6-minute walk test [6MWT] in 107 patients with interstitial lung disease) contained
sufficient raw data for us to calculate the sensitivity (88%), specicity (81%), and positive and negative predictive value (79% and 89% respectively) of the 1MSTST. The other 4 empirical studies included two predictive studies on patients with Covid-19, and two on HIV positive patients with suspected pneumocystis pneumonia. We found no studies on the 40-step walk test (a less demanding test that is widely used in clinical practice to assess Covid-19 patients).Discussion
Exertional desaturation tests have not yet been validated in patients with (or suspected of having) Covid-19. Whilst there is limited evidence for the diagnostic accuracy of the 1MSTST in other diseases, specfic features of this disease (e.g. exertional hypoxia is common and many assessments are done remotely with no clinician present to resuscitate) may raise safety issues. The less strenuous 40-step walk test should be urgently evaluated.
See the article from pages 2 through 10 of the PDF for the outstanding discussion of the use of exercise tesing for hypoxia in COVID-19. The text is an excellent short review on all aspects of exercise testing for hypoxia in other lung diseases.
Conclusion
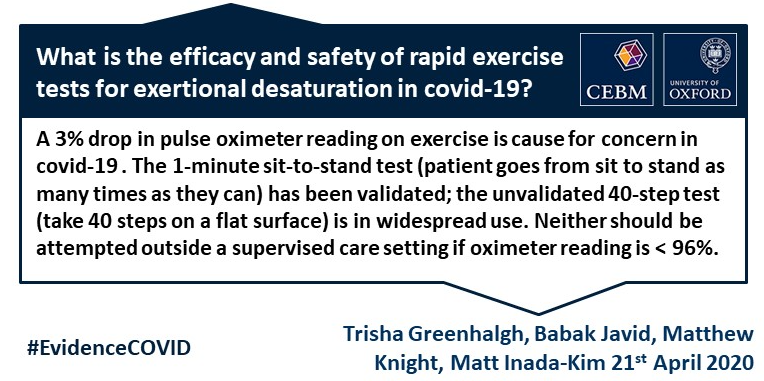
The 40-step test (which is in widespread clinical use but has not been validated) and the 1MSTST are considered the least demanding tests and therefore may be the most appropriate for recommending to patients at home (perhaps modifed so the patient is not advised to complete “as many as you can” in the 1MSTST). We hypothesise that they are specic but not sensitive (that is, a positive test is serious cause for concern but a negative test should not necessarily reassure), though there is currently no hard data on this.
More research is needed on the prognostic value and clinical utility of exertional desaturation tests in all settings (GP, emergency department, ambulance), in the context of covid-19. Furthermore, an understanding of how best to ask the patient about breathlessness on exertion, and how this correlates with exertion oximetry, could also help in the assessment of hypoxia in Covid-19.
Finally, it is important to remember that a pulse oximeter reading, whether at rest or in an exertional test, does not replace thorough clinical assessment. A normal test does not necessarily mean the patient can be reassured that all is ne. Nevertheless, exertional hypoxia of 3% or more is a signicant nding and always warrants further investigation.