In this post I link to and excerpt from Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Am J Respir Crit Care Med. 2019 Oct 1;200(7):e45-e67.
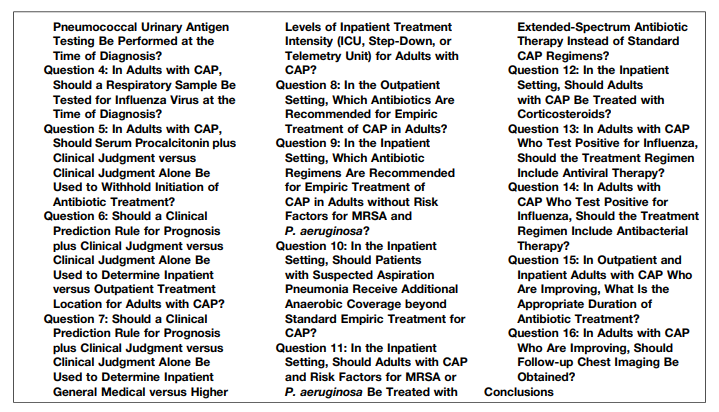
The Guidelines asks and answers the following 16 Questions Regarding Community Acquired Pneumonia:
The guidelines provide the rationale for all of the recommendations in the article.
These are my study notes and so I’m just going to excerpt the recommendations for each of the Sixteen Questions.
Question 1: In Adults with CAP, Should Gram Stain and Culture of Lower Respiratory Secretions Be Obtained at the Time of Diagnosis?
The authors recommend not getting Gram Stain and Culture in CAP patients managed as out patients.
They do recommend Gram Stain and Culture in hospitalized patients 1) who have severe pneumonia [Table 1] or are intubated; or 2) a. – receiving empiric rx for MRSA or Pseudomonas or b. – have been previously infected with one or the other of those species or c. – patients who have been hospitalized in the previous 90 days and have recieved IV antibiotics.
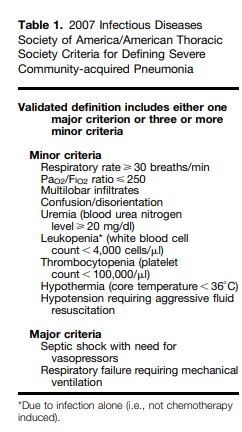
Table 1 below defines Severe Community-acquired Pneumonia.
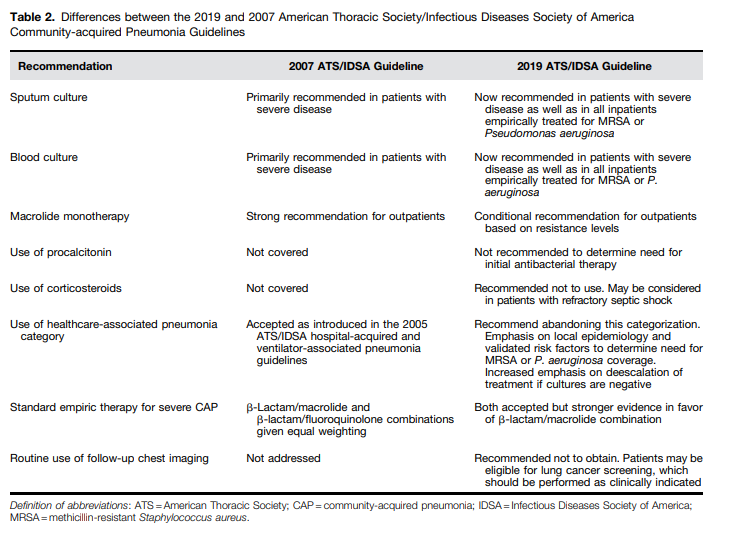
Table 2 highlights the differences between the 2007 and 2019 Guidelines
Question 2: In Adults with CAP, Should Blood Cultures Be Obtained at the Time of Diagnosis?
The authors do not recommend blood cultures in patients with CAP who are managed as outpatients.
They do recommend blood cultures in hospitalized patients with severe pneumonia [Table 1 above]; in patients empirically treated for MRSA or for Pseudomonas; or in patients previously infected with MRSA or Pseudomonas, especially respiratory tract infections; or in patients who were hospitalized and received IV antibiotics in the previous 90 days.
Question 3: In Adults with CAP, Should Legionella and Pneumococcal Urinary Antigen Testing Be Performed at the Time of Diagnosis?
Recommendation.
We suggest not routinely testing urine for pneumococcal
antigen in adults with CAP (conditional recommendation, low quality of evidence), except in adults with severe
CAP (conditional recommendation, low quality of evidence).We suggest not routinely testing urine for Legionella antigen in adults with CAP (conditional recommendation, low quality of evidence), except
1. in cases where indicated by epidemiological factors, such as
association with a Legionella outbreak or recent travel (conditional recommendation, low quality of evidence); or2. in adults with severe CAP (see Table 1) (conditional recommendation, low quality of evidence).
We suggest testing for Legionella urinary antigen and collecting lower respiratory tract secretions for Legionella culture on selective media or Legionella nucleic acid amplification testing in adults with severe CAP (conditional recommendation, low quality of evidence).
An increase in Legionella infections in the United States in the past decade highlights the importance of this diagnosis especially among severely ill patients, particularly in the setting of potential outbreaks due to a common source, although most cases are not associated with a known outbreak and remain sporadic (30, 31).
Question 4: In Adults with CAP, Should a Respiratory Sample Be Tested for Influenza Virus at the Time of Diagnosis?
Recommendation. When influenza viruses are circulating in the community, we recommend testing for influenza with a rapid influenza molecular assay (i.e., influenza nucleic acid amplification test), which is preferred over a rapid influenza diagnostic test (i.e., antigen test) (strong recommendation, moderate quality of evidence).
See my post Links To And Excerpts From 2018 Update Of The Influenza Guidelines
Posted on January 5, 2020 by Tom Wade MD.
Question 5: In Adults with CAP, Should Serum Procalcitonin plus Clinical Judgment versus Clinical Judgment Alone Be Used to Withhold Initiation of Antibiotic Treatment?
Recommendation. We recommend that empiric antibiotic therapy should be initiated in adults with clinically suspected
and radiographically confirmed CAP regardless of initial serum procalcitonin level (strong recommendation, moderate quality of evidence).
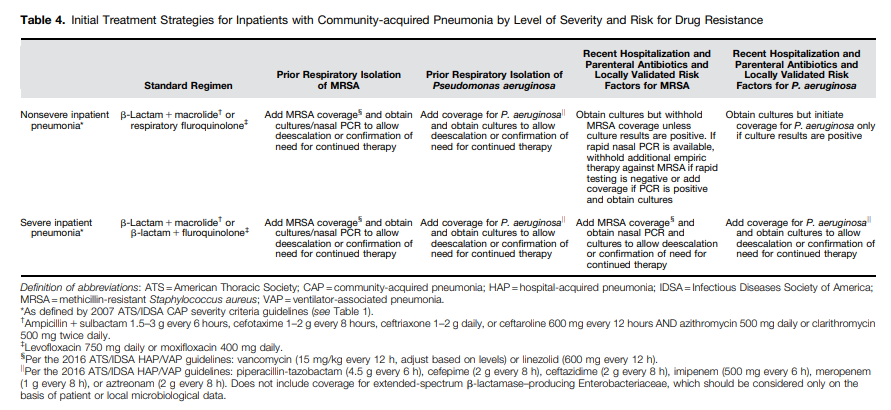
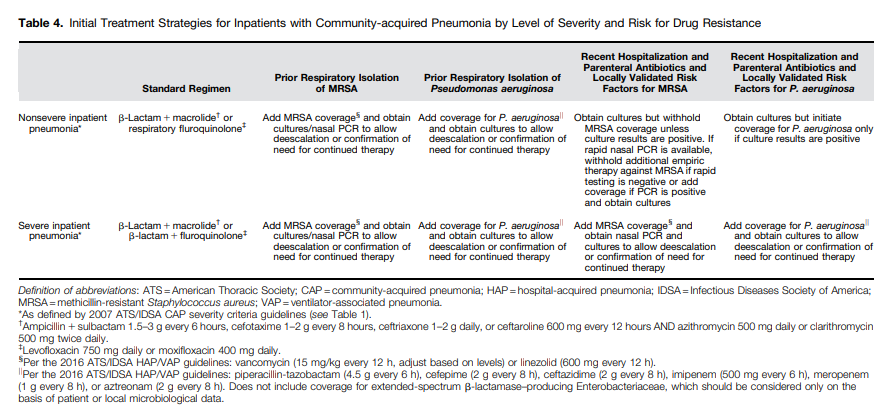
Table 4. Treatment for inpatient community-acquired pneumonia
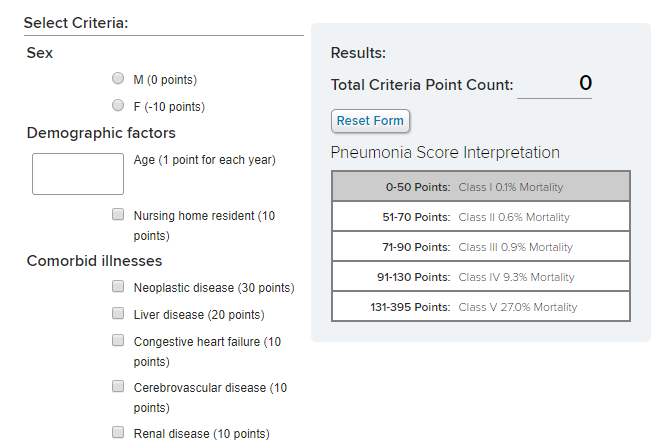
Question 6: Should a Clinical Prediction Rule for Prognosis plus Clinical Judgment versus Clinical Judgment Alone Be Used to Determine Inpatient versus Outpatient Treatment Location for Adults with CAP?
Recommendation. In addition to clinical judgement, we recommend that clinicians use a validated clinical prediction rule for prognosis, preferentially the Pneumonia Severity Index* (PSI) (strong recommendation, moderate quality of evidence) over the CURB-65 (tool based on confusion, urea level, respiratory rate, blood pressure, and age >65) (conditional
recommendation, low quality of evidence), to determine the need for hospitalization in adults diagnosed with CAP.
* Pneumonia Severity Index – Reference From The Medscape Calculator
Community-Acquired Pneumonia Severity Index (PSI) for Adults
Clinical severity is not the only consideration in determining the need for hospital admission (49, 50). Some patients
have medical and/or psychosocial contraindications to outpatient therapy, such as inability to maintain oral intake,
history of substance abuse, cognitive impairment, severe comorbid illnesses, and impaired functional status.
The PSI may underestimate illness severity among younger patients and oversimplify how clinicians interpret continuous variables (e.g., all systolic blood pressures ,90 mm Hg are considered abnormal, regardless of the patient’s baseline and actual measurement). Therefore, when used as a decision aid, the PSI should be used in conjunction with clinical judgment.Question 7: Should a Clinical Prediction Rule for Prognosis plus Clinical Judgment versus Clinical Judgment Alone Be Used to Determine Inpatient General Medical versus Higher Levels of Inpatient Treatment Intensity (ICU, StepDown, or Telemetry Unit) for Adults with CAP?
Recommendation. We recommend direct admission to an ICU for patients with hypotension requiring vasopressors or
respiratory failure requiring mechanical ventilation (strong recommendation, low quality of evidence).For patients not requiring vasopressors or mechanical ventilator support, we suggest using the IDSA/ATS 2007 minor severity criteria (Table 1) together with clinical judgment to guide the need for higher levels of treatment intensity (conditional recommendation, low quality of evidence).
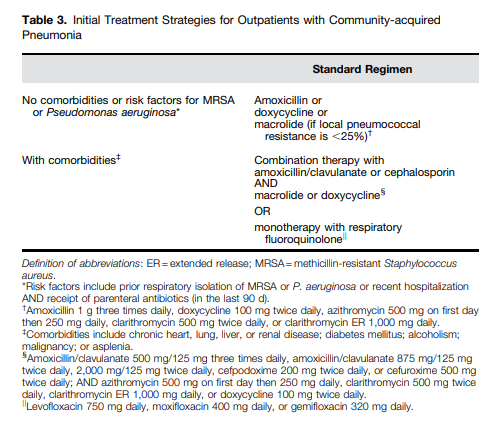
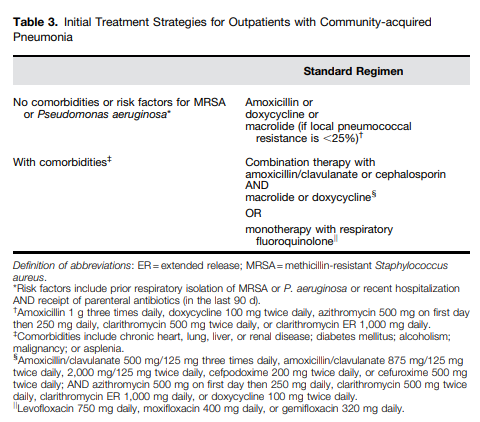
Question 8: In the Outpatient Setting, Which Antibiotics Are Recommended for Empiric Treatment of CAP in Adults?
Question 9: In the Inpatient Setting, Which Antibiotic Regimens Are Recommended for Empiric Treatment of CAP in Adults without Risk Factors for MRSA and P. aeruginosa?
Question 10: In the Inpatient Setting, Should Patients with Suspected Aspiration Pneumonia Receive Additional Anaerobic Coverage beyond Standard Empiric Treatment for CAP?
Recommendation. We suggest not routinely adding anaerobic coverage for suspected aspiration pneumonia unless lung abscess or empyema is suspected (conditional recommendation, very low quality of evidence).
Question 11: In the Inpatient Setting, Should Adults with CAP and Risk Factors for MRSA or P. aeruginosa Be Treated with Extended-Spectrum Antibiotic Therapy Instead of Standard CAP Regimens?
We recommend clinicians only cover empirically for MRSA or P. aeruginosa in adults with CAP if locally validated risk
factors for either pathogen are present (strong recommendation, moderate quality of evidence). Empiric treatment options for MRSA include vancomycin (15 mg/kg
every 12 h, adjust based on levels) or linezolid (600 mg every 12 h). Empiric treatment options for P. aeruginosa include
piperacillin-tazobactam (4.5 g every 6 h), cefepime (2 g every 8 h), ceftazidime (2 g every 8 h), aztreonam (2 g every 8 h),
meropenem (1 g every 8 h), or imipenem (500 mg every 6 h).If clinicians are currently covering empirically for MRSA or P. aeruginosa in adults with CAP on the basis of published
risk factors but do not have local etiological data, we recommend continuing empiric coverage while obtaining culture data to establish if these pathogens are present to justify continued treatment for these pathogens after the first few days of empiric treatment (strong recommendation, low
quality of evidence).Question 12: In the Inpatient Setting, Should Adults with CAP Be Treated with Corticosteroids?
Recommendation. We recommend not routinely using corticosteroids in adults with nonsevere CAP (strong
recommendation, high quality of evidence).We suggest not routinely using corticosteroids in adults with severe CAP (conditional recommendation, moderate
quality of evidence).We suggest not routinely using corticosteroids in adults with severe influenza pneumonia (conditional recommendation, low quality of evidence).
We endorse the Surviving Sepsis Campaign recommendations on the use of corticosteroids in patients with CAP and refractory septic shock (169).
Question 13: In Adults with CAP Who Test Positive for Influenza, Should the Treatment Regimen Include Antiviral Therapy?
Recommendation. We recommend that antiinfluenza treatment, such as oseltamivir, be prescribed for adults with CAP who test positive for influenza in the inpatient setting, independent of duration of illness before diagnosis (strong recommendation,
moderate quality of evidence).We suggest that antiinfluenza treatment be prescribed for adults with CAP who test positive for influenza in the outpatient setting, independent of duration of illness before diagnosis (conditional recommendation, low quality of evidence).
Several observational studies suggest that treatment with oseltamivir is associated with reduced risk of death in patients
hospitalized for CAP who test positive for influenza virus (181, 182). Treatment within 2 days of symptom onset or
hospitalization may result in the best outcomes (183, 184), although there may be benefits up to 4 or 5 days after symptoms
begin (181, 185).The use of antiinfluenza agents in the outpatient setting reduces duration of symptoms and the likelihood of lower
respiratory tract complications among patients with influenza (186), with most benefit if therapy is received within 48 hours after onset of symptoms (187).Question 14: In Adults with CAP Who Test Positive for Influenza, Should the Treatment Regimen Include Antibacterial Therapy?
Recommendation. We recommend that standard antibacterial treatment be initially prescribed for adults with clinical and
radiographic evidence of CAP who test positive for influenza in the inpatient and outpatient settings (strong recommendation, low quality of evidence).Question 15: In Outpatient and Inpatient Adults with CAP Who Are Improving, What Is the Appropriate Duration of Antibiotic Treatment?
Recommendation. We recommend that the duration of antibiotic therapy should be guided by a validated measure of clinical
stability (resolution of vital sign abnormalities [heart rate, respiratory rate, blood pressure, oxygen saturation, and
temperature], ability to eat, and normal mentation), and antibiotic therapy should be continued until the patient achieves stability and for no less than a total of 5 days (strong
recommendation, moderate quality of evidence).Failure to achieve clinical stability within 5 days is associated with higher mortality and worse clinical outcomes (205–207). Such failure should prompt assessment for a pathogen resistant
to the current therapy and/or complications of pneumonia (e.g., empyema or lung abscess) or for an alternative source of
infection and/or inflammatory response (208, 209).When assessment of clinical stability has been introduced into clinical practice, patients have shorter durations of antibiotic therapy without adverse impact on outcome (210). All clinicians should therefore use an assessment of clinical stability as part of routine care of patients with CAP.
Longer courses of antibiotic therapy are recommended for 1) pneumonia complicated by meningitis, endocarditis, and other deep-seated infection; or 2) infection with other, less-common
pathogens not covered in these guidelines (e.g., Burkholderia pseudomallei, Mycobacterium tuberculosis or endemic fungi).Question 16: In Adults with CAP Who Are Improving, Should Follow-up Chest Imaging Be Obtained?
Recommendation. In adults with CAP whose symptoms have resolved within 5 to 7 days, we suggest not routinely obtaining
follow-up chest imaging (conditional recommendation, low quality of evidence).[The conclusions section should be reviewed in its entirety as it is a great summing up of the whole guideline.]