In this post I link to the show notes and podcast and embed the podcast EMCrit 256 – RUSH Redux with Jacob Avila. September 18, 2019 by Dr Scott Weingart of EMCrit.
And here is the intro to the brief show notes, Dr. Weingart is speaking:
Some dozen years ago, a couple of my buddies and I created the RUSH exam. Today, I give you an update:
To keep me from saying something stupid regarding ultrasound, I wanted to get a master of all things ED POCUS to act as chaperone. There is no better person to fill this role than…
Jacob Avila – Host of the 5minutesono podcast and cohost of the ultrasound podcast, Jacob is an incredible ultrasound educator.
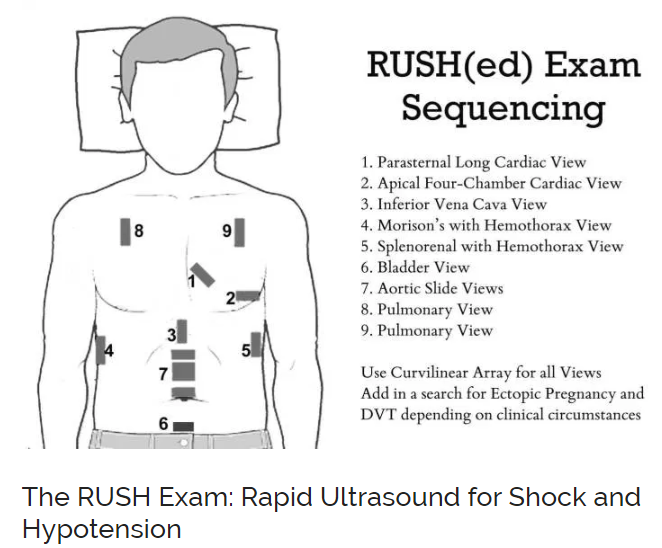
Here is the graphic from Rapid Ultrasound for Shock and Hypotension – the RUSH Exam from the earlier EMCrit post on the topic:
Dr. Weinberg states in the EMCrit 265 that if you cannot get good views on the chest of the parasternal and apical views, you can usually get a good substernal view of the heart and vice-versa.
So we start with the heart. And we’re looking for global function, pericardial effusion, and right heart enlargement.
You get a parasternal long axis and an apical four chamber. But if you have poor views in the chest, you will have a good subxiphoid. You just need to do one or the other.
So you could do the two chest views, parasternal long and apical 4-chamber and those will give you global LV function, pericardial effusion, and relative chamber size.
If you can’t get those views in the chest, subxiphoid will give you a reasonable 4-chamber. And [it] will give you enough information to get by with left ventricular function at this point.
One thing that wasn’t in the original paper but that wasn’t in the original paper but has been life saving for my patients in some circumstances–
Is, if you see a big right heart, sure it might be a pulmonary embolus but the other thing it should make you scared of is – is this undiagnosed pulmonary hypertension [or maybe it has been diagnosed but you don’t have the information available to you].
And that is a patient knowing this [pulmonary hypertension] will radically change your management whether this patient needs to be intubated right now or not.
So if you see a big right heart, you should realize that you could kill this patient [with pulmonary hypertension] in the peri-intubation.
And you probably should do everything in your power not to intubate as long as possible until certainly they have been fully resuscitated.
And even then, maybe it is not the greatest idea in a patient with a huge right heart to intubate at all if you can avoid it.
[And the above] is why we will always do a RUSH exam before we intubate a critically ill patient [if we have a second].
If we see that big right heart, our entire vision of the next step has changed. And we will not put a tube in this patient until everything is exactly right.
Then the next step is you evaluate the IVC. But don’t drown the septic patient in fluid.
Now I would say if you have a septic shock patient, give the patient a fluid bolus if you think they need it and can handle it.
And then stop regardless of what the IVC is doing.
They don’t need more fluid unless they have external losses.
You know, if the patient is vomitting, if they have massive diarrhea, or what have you.
But other than that if all the losses are internal – going from their intravascular space to their interstitium and their third spaces.
Don’t replace that. We have better ways of handling that now.
So give 20 to 30 cc [per kg] if they can handle it and then probably stop.
So now the IVC is not an indication to give fluid, it is just an indication of what is going on with their right sided heart pressures.
It is a gestalt. If you an iron pipe IVC with no variation and a big right heart, it is just an additional peace of information, that is saying there is something going on that his keeping that right heart from ejecting.
If you see an IVC that is completely collapsing with respiration, you can say a few things.
Chances are good if the clinical milieu matches that that they probably could take a little fluid. It doesn’t mean you have to give it. And the right heart pressures are low.
And that is all you can say. It just adds an aditional fact to your vision of what’s going on with the patient.
But don’t start measuring, this is key. No calibers. Just look at the IVC over two breaths.
And the next step is Morrison’s Pouch.
Dr. Weinberg says he just does Morrison’s pouch after putting the patient in Trendenlenberg 9and he looks for the liver tip.
You will never find a patient with significant intra-abdominal fluid or blood that does not have a positive Morrison’s in Trendelenberg. I’ve never seen it.
I’ve never found a spleno-renal or bladder view to tell me any information that Morrison’s at the liver tip does not.
Start at 19:15
Dr. Weinberg reminds us that the experienced clinician should be able to accomplish the exam in about 60 seconds.
I believe that some clinicians might want to use the phased array cardiac probe for the entire exam rather than the curvilinear probe. Here is what Dr. Lichtenstein advises in *The BLUE-points: three standardized points used in the BLUE-protocol for ultrasound assessment of the lung in acute respiratory failure [PubMed Abstract] [Full Text HTML] [Full Text PDF] Critical Ultrasound Journal [Open Access but now called The Ultrasound Journal]. August 2011, Volume 3, Issue 2, pp 109–110:
In the BLUE-protocol, we advise a 5-MHz microconvex
probe resulting in a small footprint, and a good resolution
for both superficial and deep disorders (Fig. 2). This probe
also allows satisfactory analysis of the vessels, heart, optic
nerves, belly, i.e., whole body analysis, neonate excepted
[2]. Those who do not benefit from this probe will need the
good resolution of abdominal probes for the anterior
analysis of the artifacts, the good superficial resolution of
linear probes for details on lung sliding, and the good
ergonomy of cardiac probes for PLAPS detection, taking
maximal care for disinfecting each probe between changes,
which prevents the BLUE-protocol to be performed within
3 min as advocated [4].
Returning to Dr. Weingart’s podcast, he reminds us that the mnemonic HI-MAPP refers to the order in which the examination is performed.