In addition to today’s resource, please review:
- Acute Intermitent Porphyria from StatPearls. Last Update: May 1, 2023
- Familial Mediterranean Fever from StatPearls. Last Update: July 31, 2023
- Systemic Mastocytosis from StatPearls. Last Update: July 4, 2023
- Eosinophilic Gastroenteritis from StatPearls. Last Update: June 26, 2023
- Hereditary Angioedema from StatPearls. Last Update: May 1, 2023
- Malabsorption Syndromes from StatPearls. Last Update: July 24, 2023
- Celiac Disease from StatPearls. Last Update: February 4, 2025
- Inflammatory Bowel Disease from StatPearls.
Today, I review and embed Medical Mystery Solved — A Swell Diagnosis | NEJM.
All that follows is from the above resource.
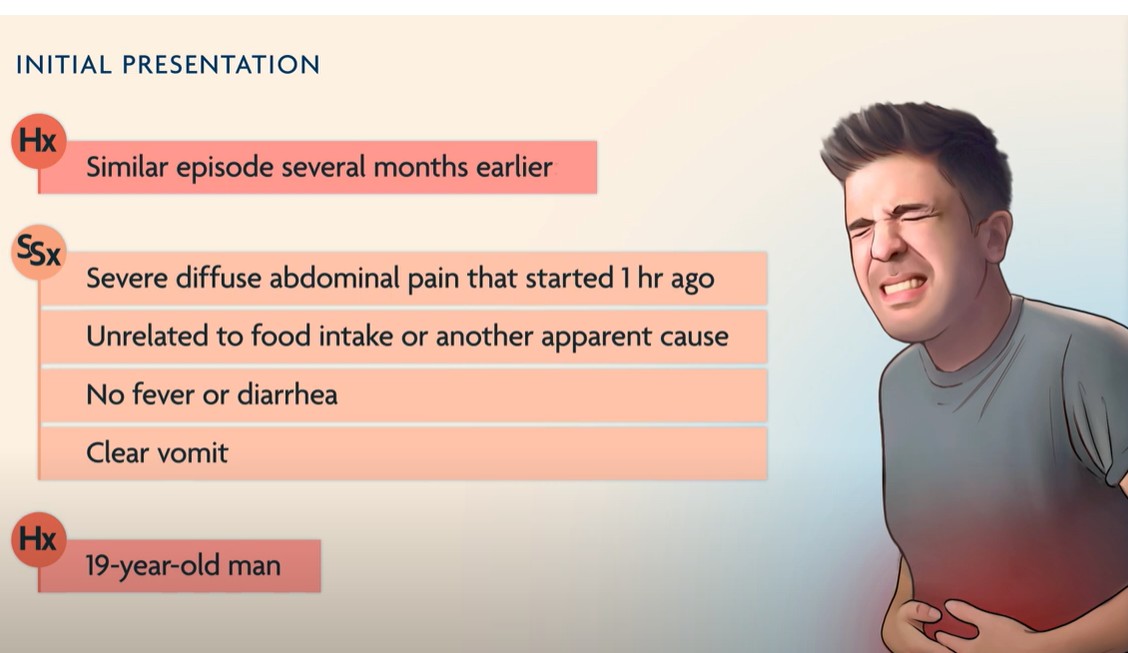
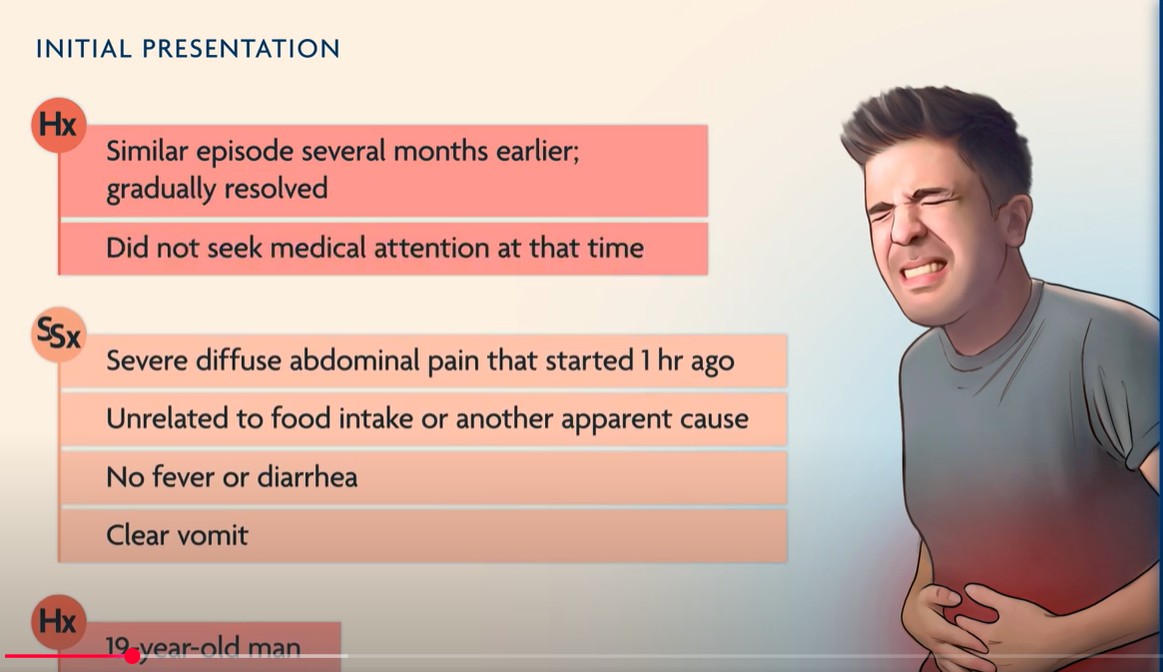
Feb 26, 2025This Double Take video from the New England Journal of Medicine describes a man with recurrent severe diffuse abdominal pain without obvious associated symptoms. Based on a Clinical Problem-Solving article published in the Journal, the video explores the broad differential diagnosis of recurring abdominal pain and the evolution of the diagnosis as new clinical findings are presented. For further reading, the Clinical Problem-Solving article referenced in this video is available at https://www.nejm.org/doi/full/10.1056… : A Swell Diagnosis (Allam et al., in the January 4, 2024, issue of the Journal).
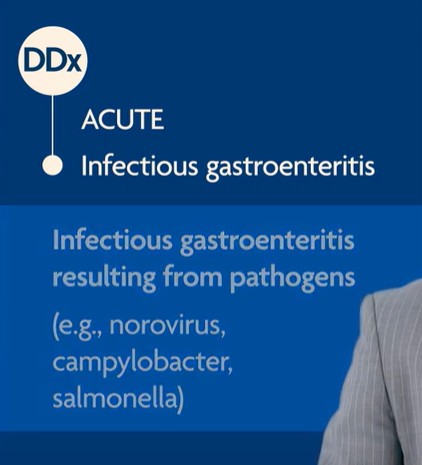
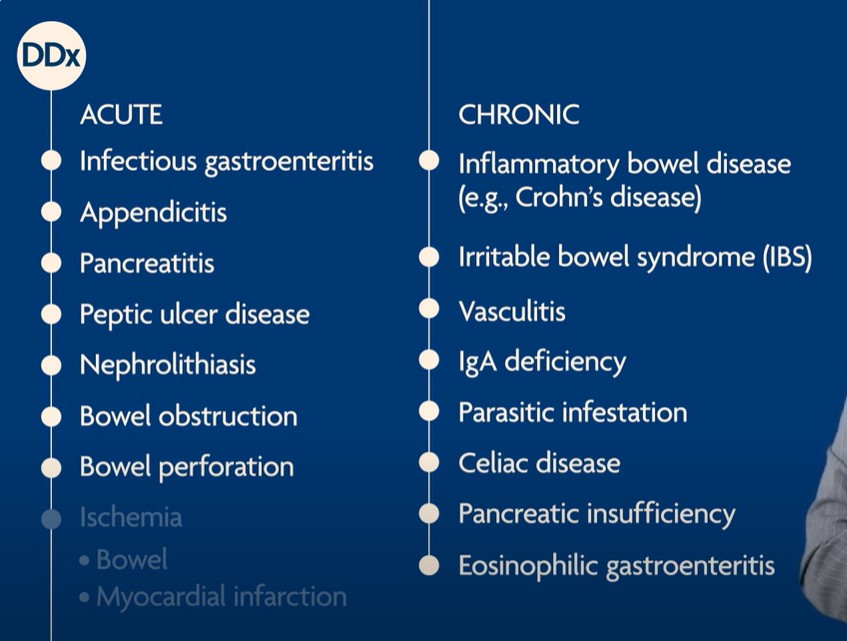
1:231:562:28The normal stools make inflammatory bowel disease and malabsorption syndromes, such as celiac
2:34
disease or pancreatic insufficiency, unlikely.
2:38
A diagnosis of nephrolithiasis remains possible without urinary symptoms, and a urinalysis
2:43
should be performed to look for red blood cells.The normal stools make inflammatory bowel disease and malabsorption syndromes, such as celiac
disease or pancreatic insufficiency, unlikely.
A diagnosis of nephrolithiasis remains possible without urinary symptoms, and a urinalysis
should be performed to look for red blood cells.
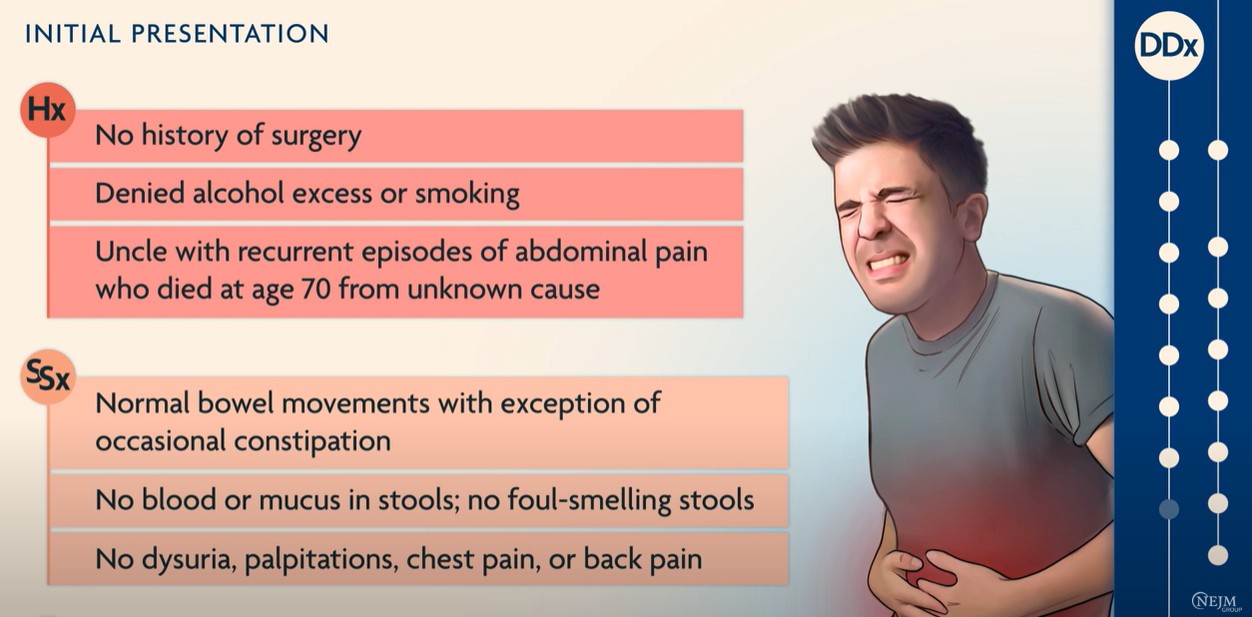
In the emergency department, the patient appeared uncomfortable but was alert and oriented.
He was tachycardic with a heart rate of 106, but otherwise had normal vital signs.
His abdomen was soft and slightly distended, with mild tenderness to palpation in the midabdomen,
without rebound tenderness or guarding.
Carnett’s sign and McBurney’s sign were both negative.
Carnett’s sign tests for abdominal-wall tenderness that increases when abdominal muscles are
tensed, and is indicative of abdominal wall pathologies, such as a rectus sheath hematoma.
The absence of Carnett’s sign suggests a visceral cause for the pain.
Conversely, McBurney’s sign looks for point tenderness on deep palpation one third of the
distance from the right anterior superior iliac spine to the umbilicus, and has been traditionally
considered a sign of acute appendicitis.
The negative Carnett’s and McBurney’s signs make abdominal wall pathologies and acute appendicitis
less likely, however we should review laboratory testing before fully ruling out appendicitis.
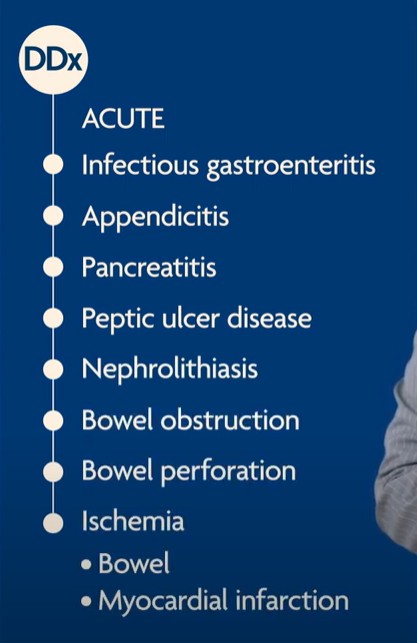
The complete blood count and basic metabolic panel were normal.
Additionally, lipase, liver enzymes, thyrotropin, and CRP levels were normal, as was the
erythrocyte sedimentation rate and urinalysis.
In the presence of normal vital signs and an unrevealing physical examination and
laboratory tests, emergencies such as an acute infection, appendicitis, obstruction of
the gastrointestinal tract, nephrolithiasis, or bowel perforation are very unlikely.
The normal lipase and liver tests are inconsistent with pancreaticobiliary disease; the normal erythrocyte
sedimentation rate and CRP make primary inflammatory disorders and autoimmune disease less likely.
He was treated with intravenous fluids and an antiemetic agent.
His symptoms completely resolved within 3 hours and he was discharged from the emergency department.
Over the next several years, the patient presented to the emergency department on numerous occasions
with the same symptom complex — unrelated to food intake and never associated with fever.
The patient noticed that after abdominal attacks he was not able to have
bowel movements for at least 8 hours.
His abdominal pain typically resolved within a few hours after supportive treatments.
He did not report mood changes, itchy rashes, flushing, weakness, or sensory
changes and had no history of psychosis.
The patient’s transient inability to defecate after a pain episode points to
temporary obstruction or dysmotility.
At this point, rare diseases that can cause severe diffuse and recurrent abdominal pain should be
considered, such as acute intermittent porphyria*, a disorder of heme metabolism;
*Acute Intermitent Porphyria from StatPearls. Last Update: May 1, 2023.
familial Mediterranean
fever*, or FMF, a genetically inherited disease characterized by recurrent attacks of fever and
serositis;
*Familial Mediterranean Fever from StatPearls. Last Update: July 31, 2023
mastocytosis*, a disorder of mast-cell proliferation*;
*Systemic Mastocytosis from StatPearls. Last Update: July 4, 2023.
and eosinophilic gastroenteritis*,
an inflammatory disorder characterized by eosinophilic infiltration of the intestinal wall.
*Eosinophilic Gastroenteritis from StatPearls. Last Update: June 26, 2023.
However, these diagnoses are inconsistent with our patient’s clinical presentation.
Patients with acute intermittent porphyria commonly have neurologic or psychiatric symptoms, such as
sensory or motor changes, mood changes, and psychosis.
Familial Mediterranean fever is unlikely in the absence of fevers, and mastocytosis is unlikely in the absence
of flushing, pruritus, urticaria, and hypotension.
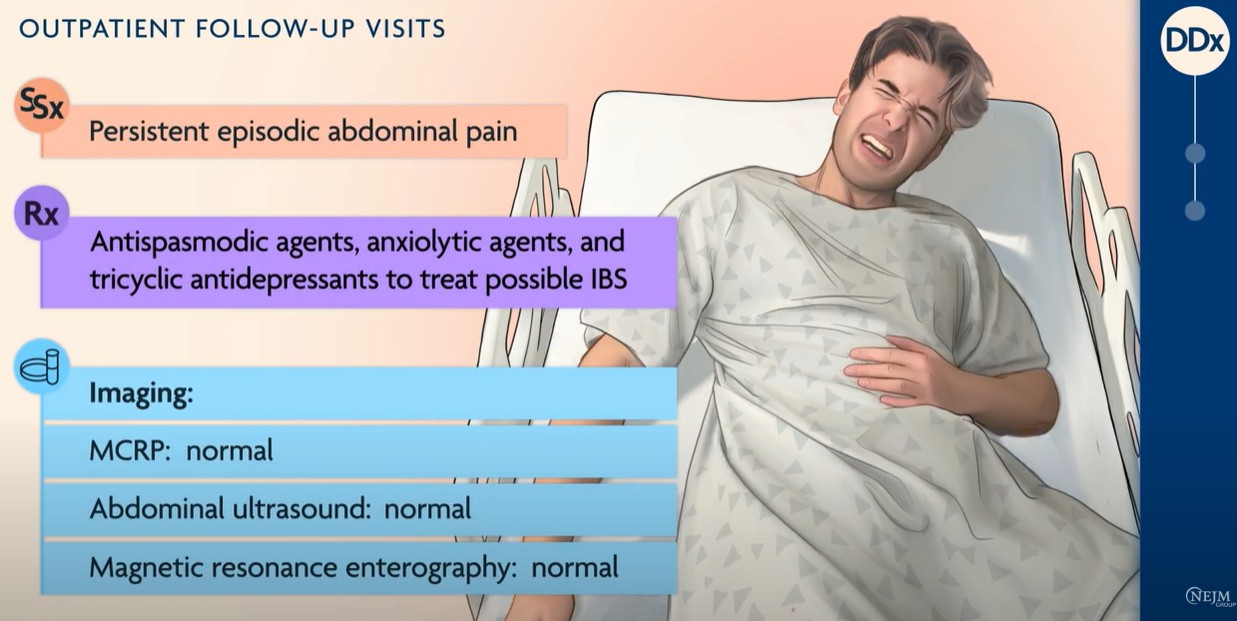
During outpatient follow-up visits, multiple upper gastrointestinal endoscopies and
colonoscopies were performed with biopsies for histologic examination, all of which were normal.
The patient’s normal intestinal biopsies tell us a lot.
The absence of villous atrophy is inconsistent with celiac disease, and the normal level of
eosinophils is incompatible with eosinophilic gastroenteritis and certain parasitic infections.
The lack of mast cells, again, argues against mastocytosis.
Finally, there are no crypt abscesses to suggest inflammatory bowel disease and no
granulomas, as may be seen in Crohn’s disease.
The normal endoscopies and colonoscopies also make parasitic infections less likely.
Additional laboratory results included normal quantitative immunoglobulin levels, negative
testing for hepatitis viruses, and negative serologies consistent with autoimmune disease.
A genetic screen for mutations associated with familial Mediterranean fever was negative.
MRI scan of the pancreatobiliary system [MRCP], abdominal ultrasonography, and magnetic
resonance enterography were all normal.
In an attempt to relieve the patient’s symptoms, antispasmodic agents, anxiolytic agents, and
tricyclic antidepressants were prescribed to treat possible irritable bowel syndrome but the
patient continued to have episodic abdominal pain.
The test results rule out FMF, IgA deficiency, hepatitis, and autoimmune disorders.
IBS is usually associated with diarrhea, or constipation, or both.
This patient reported normal stools and did not respond to medications that are often used for IBS.
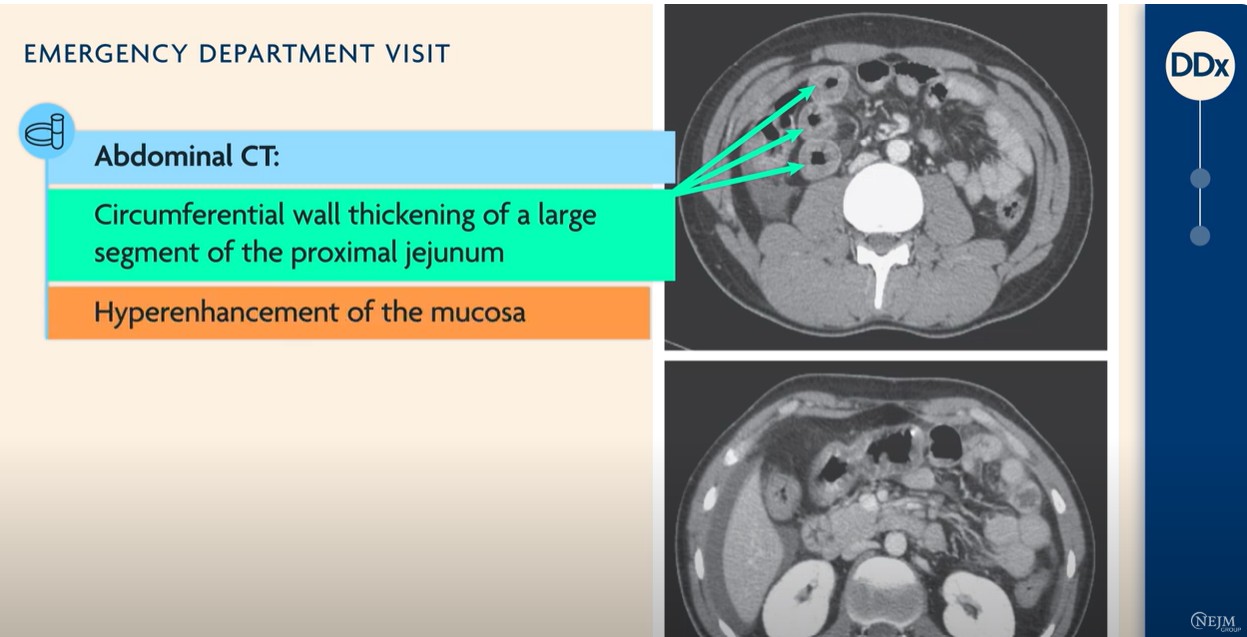
During one of the patient’s subsequent emergency department visits, abdominal CT
showed marked circumferential wall thickening of a large segment of the proximal jejunum with
hyperenhancement of the mucosa, mesenteric edema, and a moderate amount of intraabdominal fluid.
The intermittent wall thickening of the jejunum probably represents mucosal or submucosal edema.
This finding — along with the history of recurrent abdominal pain in an uncle — is strongly suggestive
of hereditary angioedema, a disease characterized by recurrent episodes of swelling in various parts
of the body that can be severely debilitating.
Abdominal pain can be the sole symptom in an attack of angioedema.
Triggers include emotional stress, physical trauma, infections, physical exertion,
surgery, and other medical procedures.
At this point, the patient’s abdominal attacks had been occurring intermittently for 10 years and were
increasing in frequency — now up to every 2 weeks.
On further questioning, the patient also recalled a single episode of mild
tongue swelling in the remote past.
Testing revealed a low C4 complement level and a low C1 esterase inhibitor activity level.
The lab results, coupled with the single episode of tongue swelling, are consistent
with a diagnosis of hereditary angioedema.
See StatPearls‘ Hereditary Angioedema. Last Update: May 1, 2023.