Bottom line of this article in this post is that we don’t really know the significance or the treatment of this problem. See the Conclusion Section below.
See Resources (2) through (4) in Additional Resources for more helpful articles on this subject. They are worth reading now.
Here are links to Morning blood pressure surge: pathophysiology, clinical relevance and therapeutic aspects [PubMed Abstract] [Full Text HTML] [Full Text PDF]. 2018; 11: 47–56. Published online 2018 May 24.
And here are excerpts from the above article:
Abstract
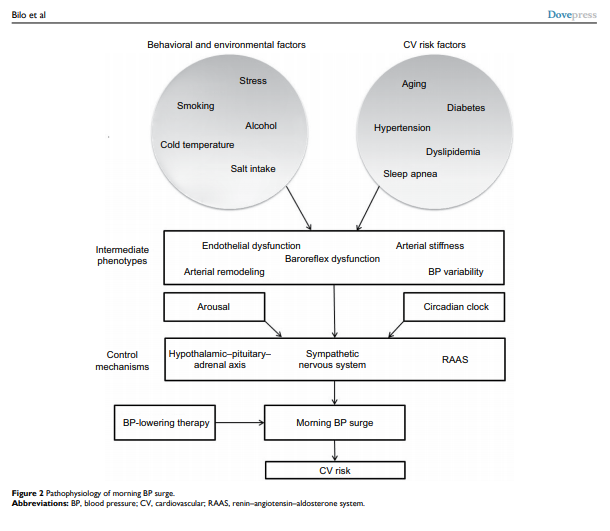
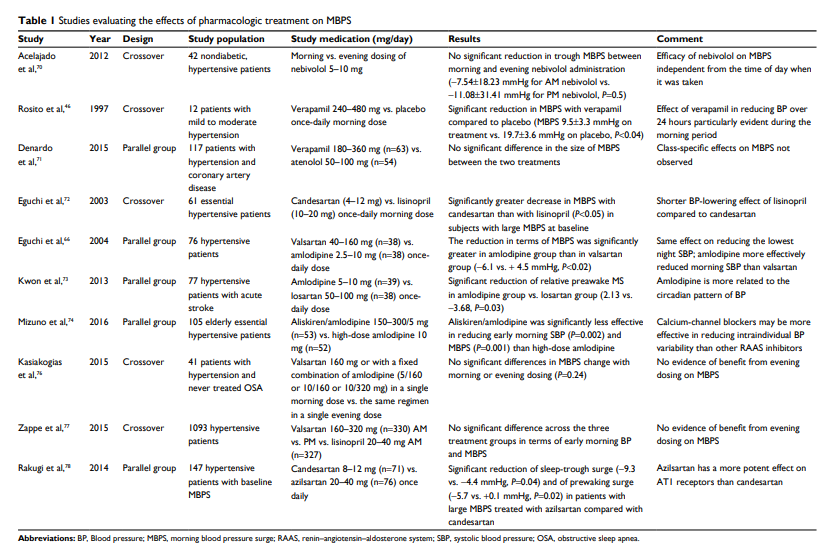
Morning hours are the period of the day characterized by the highest incidence of major cardiovascular events including myocardial infarction, sudden death or stroke. They are also characterized by important neurohormonal changes, in particular, the activation of sympathetic nervous system which usually leads to a rapid increase in blood pressure (BP), known as morning blood pressure surge (MBPS). It was hypothesized that excessive MBPS may be causally involved in the pathogenesis of cardiovascular events occurring in the morning by inducing hemodynamic stress. A number of studies support an independent relationship of MBPS with organ damage, cerebrovascular complications and mortality, although some heterogeneity exists in the available evidence. This may be due to ethnic differences, methodological issues and the confounding relationship of MBPS with other features of 24-hour BP profile, such as nocturnal dipping or BP variability. Several studies are also available dealing with treatment effects on MBPS and indicating the importance of long-acting antihypertensive drugs in this regard. This paper provides an overview of pathophysiologic, methodological, prognostic and therapeutic aspects related to MBPS.
Conclusion
MBPS is a complex phenomenon driven by several mechanisms, among which sympathetic activation plays the central
role. It is closely related with a number of physiological
variables, including arterial stiffness and endothelial function, as well as with specific patterns characterizing 24-hour BP profile, such as nocturnal BP fall and BP variability. Considering the limited reproducibility of current MBPS estimates, further research is needed to refine the methodology of its assessment.While a number of studies demonstrated the association
of MBPS with outcomes, it is not clear whether it should
be considered a causal factor or only an epiphenomenon
of global impairment of cardiovascular function. It is also
not clear whether it may represent a target for treatment,
although the available evidence suggests that MBPS size
may be limited by strategies based on the use of long-acting
drugs, aimed at providing a stable and sustained BP control
throughout the 24 hours.
Additional Resources:
(1) Morning blood pressure monitoring in the management of hypertension [PubMed Abstract]. J Hypertens. 2017;35:1554–1563. Wang J-G, Kario K, Park J-B, Chen C-H.
(2) Morning blood pressure surge: pathophysiology, clinical relevance and therapeutic aspects [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Integr Blood Press Control. 2018 May 24;11:47-56.
(3) Ambulatory blood pressure monitoring in clinical practice [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Indian Heart J. 2019 Jan – Feb;71(1):91-97.
(4) Practical Aspects of Home and Ambulatory Blood Pressure Monitoring [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Methodist Debakey Cardiovasc J. 2015 Oct-Dec;11(4):214-8.