In this post I link to and excerpt from the Cribsiders Aug 12, 2020 episode, #5 MIS-C: When COVID Affects Kids
AUGUST 12, 2020 By Dr JUSTIN BERK.
Here is the podcast:
Here are excerpts from the show notes:
THE DIAGNOSIS AND MANAGEMENT OF MULTISYSTEM INFLAMMATORY SYNDROME IN CHILDREN (MIS-C) WITH DR. ADRIANA TREMOULET
SUMMARY
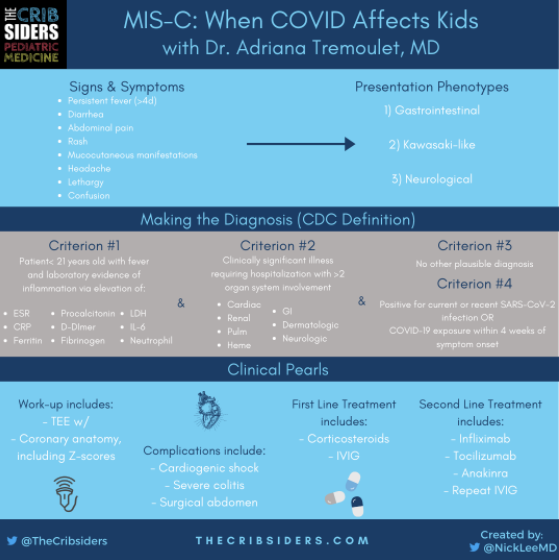
Four weeks after a COVID exposure, children may not be completely in the clear. MIS-C is a post-infectious inflammatory state that affects pediatric patients and can lead to heart failure, acute abdomen, and a new Kawasaki-like syndrome in older ages. We discuss the emerging evidence with expert, Dr. Adriana Tremoulet ( UCSD), who sits on the American College of Rheumatology MIS-C and COVID-19 Related Hyperinflammation Task Force. She educates us on the presentation, diagnosis, and management MIS-C so when you see this condition, you’ll be ready!
MIS-C Pearls
- The presentation of MIS-C seems to have three common phenotypes: Kawasaki-like, gastrointestinal, and neurologic presentations
- Other differential diagnoses (eg toxic shock, Kawasaki) should be ruled out prior to treating the patient as MIS-C
- Very elevated inflammatory markers (CRP > 10mg/dL) are frequently seen in MIS-C
- These patients can develop a critical illness, usually caused by cardiogenic shock. Others have presented with acute abdomen
- First-line treatment for MIS-C is typically steroids or IVIG
- Second-line treatment considerations may include anakinra, infliximab, tocilizumab
Evaluating for and Diagnosing MIS-C
The Febrile Child During COVID-19
Typically, a child with MIS-C will have had fevers for days and will be ill-appearing. There are a few questions that the examiner can ask to investigate MIS-C on the differential diagnosis:
- Has the fever been persistent over several days (> 3 to 4 days)?
- Is the child toxic appearing?
- Has there been significant COVID-19 activity within the area where the child resides (both community and within the household)?
If the answer is no to all of these questions, it is less likely to be MIS-C.
The Clinical Presentation of MIS-C
There appear to be at least three main presentations of MIS-C:
- Gastrointestinal phenotype: These patients can present with severe abdominal pain and/or significant diarrhea. Dr. Tremoulet notes that there have patients whose abdominal pain is so severe that they were taken to the operating room for appendectomy (Cabrero-Hernandez 2020).
- Kawasaki-like phenotype: These patients present with the fever and mucocutaneous syndrome that is more commonly associated with Kawasaki Disease.
- Neurological phenotype: These patients present with ataxia, confusion, significant headaches, seizures, and occasionally focal neurologic findings.
Producer’s Note: Most common clinical presentations include [UpToDate 2020]:
- Persistent fever > 4 days [100%]
- Gastrointestinal symptoms (abdominal pain, vomiting, diarrhea) [60 – 100%]
- Rash [45 – 75%]
- Conjunctivitis [30 – 80%]
- Mucous membrane involvement [25 – 75%]
- Neurocognitive symptoms (headache, lethargy, confusion) [30 – 60%]
If your suspicion for MIS-C is high, initial workup may include:
- CBC with differential, CMP, CRP/ESR
Dr. Tremoulet’s advice: If you decide to obtain labs, though, be sure that you have a plan to act upon them (whether it is more frequent follow-up versus asking them to present to the Emergency Department for potential admission).
Diagnosis of MIS-C
The Centers for Disease Control and Prevention (2020) defines MIS-C as:
1. An individual < 21yo with fever and laboratory evidence of inflammation (one or more of the following: elevated CRP, ESR< fibrinogen, procalcitonin, D-dimer, ferritin, LDH, or IL-6; elevated neutrophils; reduced lymphocytes; and low albumin),
and
2. Clinically significant illness requiring hospitalization with multisystem (>2) organ involvement (cardiac, renal, respiratory, hematologic, gastrointestinal, dermatologic, or neurologic).
and
3. No alternative plausible diagnoses
and
4. Positive for current or recent SARS-CoV-2 infection OR COVID-19 exposure within the 4 weeks prior to onset of symptoms.
Work-Up and Management of MIS-C
Initial Work-up of MIS-C
Diagnosis requires an interdisciplinary team of consults, oftentimes including infectious disease, rheumatology, and cardiology. This differential diagnosis includes toxic shock syndrome, Kawasaki disease, vasculitis, viral cardiomyopathy, etc.
Ideally, there should be an institution work-up designed to aid in workflow, but further labwork that you may want to obtain to check a baseline and/or trend include:
- Completed already: CBC, CMP, CRP, ESR
- Ferritin, Fibrinogen, LDH
- SARS-CoV2 PCR
- SARS-CoV2 Antibody (IgM and IgG if possible)
- BNP and troponin
- Any labwork recommended by consultants
- Echocardiogram and Electrocardiogram
Dr. Tremoulet Expert Pearl: If your platelet count is low and you have a consumptive coagulopathy, the body may not be able to mount an elevated ESR so it may appear low, but don’t be thrown off and think there is no inflammation.
Differences between MIS-C and KD: MIS-C can have more effect on heart function (with an associated elevation in BNP), while KD has more effect on coronary arteries. Presentations differ a bit too. Patients with MIS-C will often have diarrhea and GI complaints, which we don’t frequently see in KD. Often, inflammatory markers in KD, while elevated, will not be as high as those seen in patients presenting with MIS-C.
Presentation of MIS-C in adults has been documented.
Cardiac Manifestations of MIS-C
These patients can present in cardiogenic shock due to poor cardiac output. Thus, medical teams should be cautious with fluid resuscitation because over resuscitation could result in rapidly deteriorating respiratory function due to pulmonary edema.
In a study of 58 patients with MIS-C, 29 children (50%) developed shock and required inotropic support (Whittaker 2020). Concern for cardiac involvement is suggested by tachycardia (while afebrile) and an elevated BNP, though the diagnosis of heart failure is clinical.
For work-up, complete echo is required (function, coronary arteries, and coronary Z-scores). The EKG is important to evaluate for potential arrhythmias that have been documented in this patient population (Samuel 2020; Whittaker 2020).
If there are abnormalities on the EKG, it is recommended to repeat it every 48 hours to ensure there are no worsening findings (Henderson 2020). Similarly, abnormal Echos should be followed closely (7 days after discharge and more frequently inpatient as needed).
[For details on the management of MIS-C consult the show notes.]
WHAT TO WATCH FOR…
The major complication to monitor for is the development of cardiogenic shock. These patients can quickly go from compensated (perfusing well with sufficient cardiac output) to shock (where their cardiac function can no longer support their metabolic needs) that may require transfer to the Intensive Care Unit. Additionally, patients can develop worsening colitis that may even require surgical management.