Here is the link to The Clinical Pathways Library [a comprehensive list of the clinical pathways at the Children’s Hospital of Philadelphia (CHOP)].
For a complete list of the outstanding pediatric FOAM courses from the Children’s Hospital of Philadelphia, please see CHOP Open-access Medical Education.
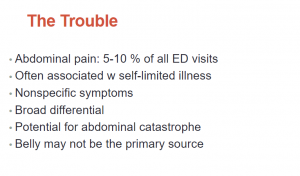
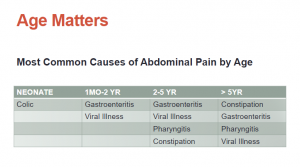
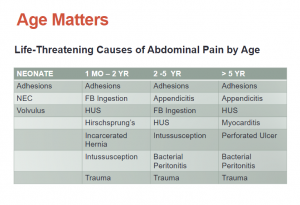
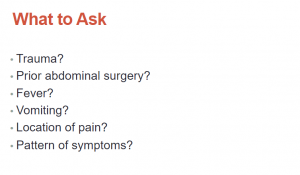
What follows are excerpts from the Pediatric Abdominal Emergencies Lecture from The Children’s Hospital of Philadelphia (CHOP):
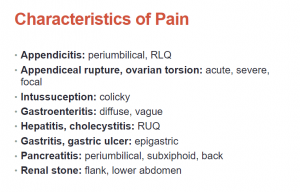
Fig 5:
Fig 6:
Fig 7:
Fig 8:
Fig 9:
Fig 10:
We commonly miss early myocarditis in a lot of infants because they confuse us because they present with GI symptoms that confuse us and mislead us away from the fact that this is actually a cardiac process rather than a primary GI process and we don’t recognize the cardiac inflammation until they come back in extremis.
See Myocarditis in infants and children: A review for the paediatrician [PubMed Abstract] [Full Text] [Full Text PDF]. Paediatr Child Health. 2001 Oct;6(8):543-5:
CLINICAL PRESENTATION
Dyspnea with feeding*, vomiting and pallor are common presenting complaints in infants. Older children
present with a marked decrease in stamina and shortness of breath in the context of a viral infection. Complaints of palpitation suggest coexistent arrhythmia.
Chest pain is nonspecific and indicates a possible associated pleural or pericardial inflammation.
*Poor feeding, weak feeding or prolonged feeding can be the only sign of myocarditis as it can of many other serious causes at the onset of disease.
On physical examination, the child is tachypneic,
tachycardic and febrile. Hypotension suggests severely
depressed cardiac function. Pallor and peripheral vasoconstriction due to sympathetic activation are usually
noted. Peripheral capillary refill is delayed. In children,
the earliest sign of fluid retention secondary to congestive
heart failure is eyelid puffiness. More severe failure presents with hepatomegaly and generalized edema. A pericardial rub and distant heart sounds suggest the
presence of an associated pericardial effusion. A soft
first heart sound is common but nonspecific and often
difficult to appreciate in the tachycardic infant. A gallop
rhythm produced by a third heart sound is frequent and
best heard at the apex. A high pitch regurgitant murmur
detected at the apex indicates coexistent mitral insufficiency.DIFFERENTIAL DIAGNOSIS
Sepsis, severe dehydration or anemia should be considered as diagnostic possibilities in the ill neonate or infant. Primary endocardial fibroelastosis and metabolic
dilated cardiomyopathy are myocardial disorders that
can present in a similar fashion. Congenital structural lesions, such as critical coarctation of the aorta or anomalous origin of the left coronary artery from the pulmonary artery, must be ruled out.
As soon as the diagnosis of myocarditis is known or suspected, even if initially mild, it is important to transfer the patient to a center that can provide circulatory support if needed.
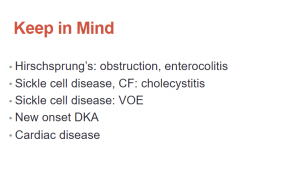
Fig 11:
Look everywhere. [On the left is pt with abdominal pain from Henoch Schonlein purpura and on the right with abdominal pain from Acute Pharyngitis.]
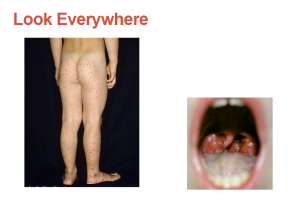
Fig 12:
The obterator and the psoas signs are meant to help identify if there is any retroperitoneal irritation or inflammation [from appendicitis].
Fig 13:
Fig 14:
Fig 15:
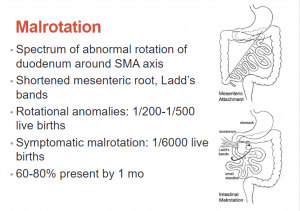
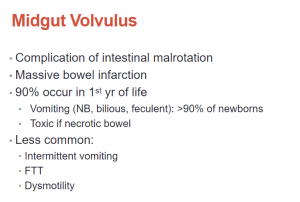
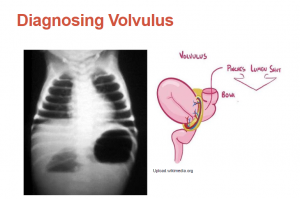
The complication we all worry about with malrotation is mid-gut volvulus where you can get massive bowel infarction. . . . The patient can become incredibly toxic in hours and you have very little time to have a sense that this is occurring and [initiate definitive] treatment.
I’ve seen babies present with non-bilious emesis, bilious emesis, with feculent emsis so keep an open mind when you are evaluating a newborn with vomitting and no other symptoms. [Emphasis added]
Fig 17:
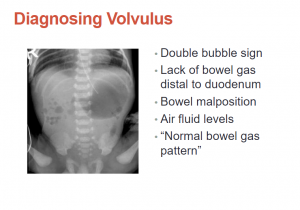
While it [an abdominal plain film] is often how we start in the emergency department, there are plenty of times when the reading is normal bowel gas pattern. So if you still have a high suspicion you need to k33p going.
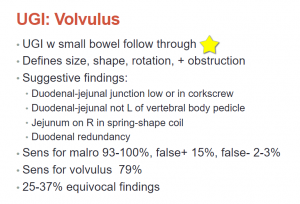
Fig 18
Fig 19
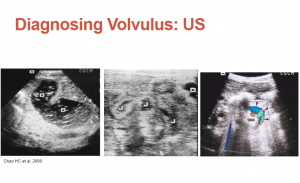
Fig 23:
Please see:
- The efficiency of sonography in diagnosing volvulus in neonates with suspected intestinal malrotation [PubMed Abstract] [Full Text] [Full Text PDF]. Medicine (Baltimore). 2017 Oct;96(42):e8287
- Ultrasound diagnosis of midgut volvulus [Full Text HTML] [Download Full Text PDF]. Appl Radiol By Mostapha Youssfi, MD; Scott Jorgenson, MD; and Richard Towbin, MD| June 10, 2016
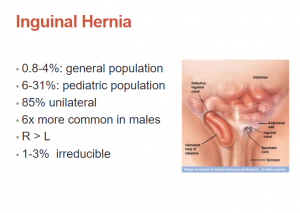
Fig 26:
Fig 27:
In the left x-ray image, we see bowel gas in the scrotum. In the right ultrasound image we see bowel in the scrotum (the orange arrow).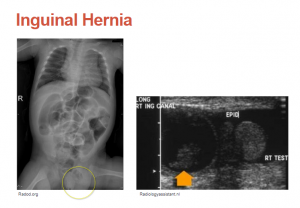
Fig 28:
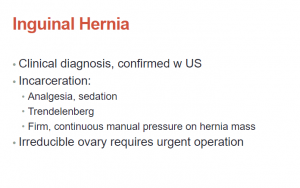
In general it is a clinical diagnosis that we might confirm with ultrasound but there are plenty of times, at least in our emergency department, when our surgeons are concerned and they can’t reduce, they go straight to the OR without imaging. . . . It is going to be impossible to reduce that [hernia] unless you actually sedate these babies. They are not going to have any kind of muscle relaxation. . . . These babies are supremely uncomfortable. We give a significant amount of sedation and comfort medications for that.
Fig 31
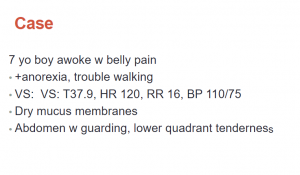
[The history below] is a very classic story for intussception.
What follows is from Diagnosis of Intussusception Using Bedside Ultrasound by a Pediatric Resident in the Emergency Department [PubMed Abstract] [Full Text] [Full Text PDF]. Hawaii J Med Public Health. 2014 Feb;73(2):58-60.
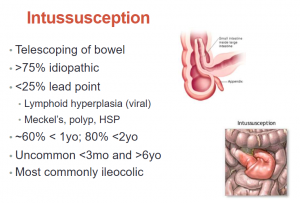
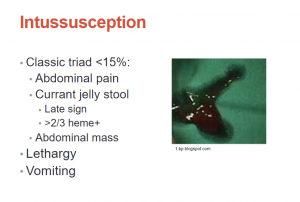
Intussusception occurs when part of the gastrointestinal tract telescopes into an adjacent distal segment and is the most common cause of intestinal obstruction in children between three months and six years of age with an incidence of 38 per 100,000 cases in the first year of life and 31 per 100,000 cases in the second year of life.6 If not promptly diagnosed and treated with enema reduction, intussusception can lead to intestinal necrosis, sepsis, or death.7 The classical presentation of intussusception consists of the triad of colicky abdominal pain, bloody stool (commonly described as “currant jelly”), and vomiting. While the presence of this triad has a positive predictive value of 93% for intussusception, it unfortunately occurs in less than 25% of cases. Many patients instead present with varying combinations of non-specific symptoms including vomiting, abdominal pain, excessive crying, or lethargy and may initially be misdiagnosed with other abdominal and neurological conditions.8,9.
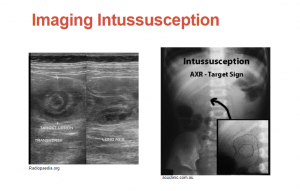
Fig 32:
Fig 33:
Fig 34:
Please see my post Evaluation Of Excessive Crying In The Infant and Toddler – Four Resources
Posted on January 30, 2019
Please see “Pediatric Emergency Ultrasound: Deep Dive on POCUS for Intussusception” – Help From ACEP With Additional Resources
Posted on January 20, 2019 by Tom Wade MD
What follows is from Diagnosis of Intussusception Using Bedside Ultrasound by a Pediatric Resident in the Emergency Department [PubMed Abstract] [Full Text] [Full Text PDF]. Hawaii J Med Public Health. 2014 Feb;73(2):58-60.
Intussusception has a characteristic appearance on ultrasound. Using warm gel and a 10 MHz linear transducer, the examiner begins the ultrasound exam at the cecum in the right lower quadrant of the abdomen and gradually moves proximally toward the right upper quadrant while aligning the transducer in a transverse orientation to the colon until the area of intussusception is encountered; this area sometimes presents as a palpable mass.6,10 On longitudinal view, the characteristic hayfork or sandwich sign is formed by three parallel hypoechoic areas separated by hyperechoic zones. These zones represent the dilated intussucipiens containing the intussuceptum and is considered pathognomonic for intussusception.15 Alternatively, the appearance of a pseudokidney sign is formed if the intussusception is curved and when the mesentery is seen on only one side of the intussusceptum.16 The pseudokidney sign is most commonly seen on long-axis view.17 On axial view, there is a hypoechoic ring from the edematous walls of the intussuscipiens around an echo-dense center formed by the interfaces of the mucosal and serosal layers of the intussusceptum. This characteristic sign, which goes by several names including bulls eye sign, target sign, donut sign, or concentric ring sign, may also be seen in normal intestinal loops and with space-occupying lesions.16
There has also been growing interest in bedside ultrasound training for pediatric emergency physicians and fellows due to the reported ease of use and high sensitivity in early learners. One study showed that six pediatric emergency medicine physicians who completed a one hour long course in bedside ultrasound were able to perform the exam with a sensitivity of 85%, specificity of 97%, positive predictive value of 85%, and negative predictive value of 97% for diagnosing intussusception.6 Another study found that a month long training course in bedside ultrasound examination enabled five pediatric emergency medicine physicians to perform bedside ultrasound with a similar positive predictive value for intussusception compared to ultrasound performed by trained gastroenterologists.20 These studies show that different approaches can be used to teach novice learners how to diagnose intussusception with ultrasound. These approaches provide physicians the benefit of a rapid diagnosis, resulting in timely treatment and reduced length of stay in the ED—benefits that were also emphasized in this study as well as in other case reports of bedside ultrasound by emergency medicine physicians.21
Our case report illustrates that ultrasound applications may also be quickly taught to general pediatric residents working in the ED.
Fig 36:
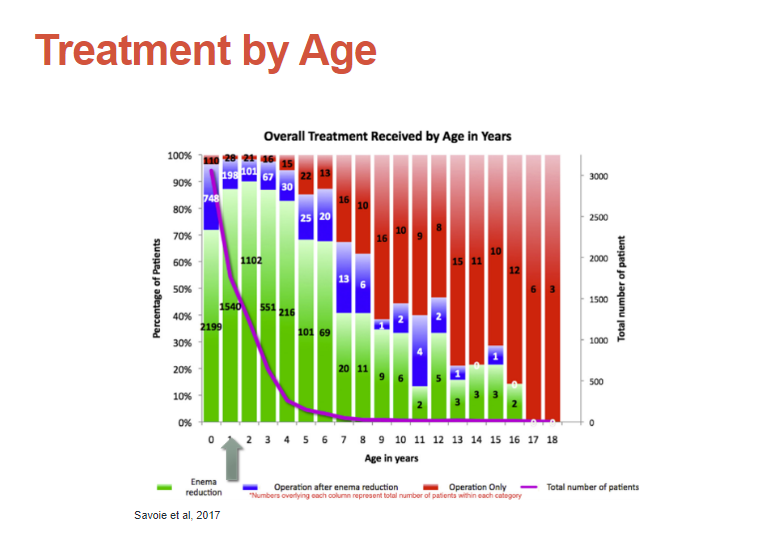
Intussusception can be treated with enema reduction, surgery after attempted enema reduction, or surgical reduction. The slide below details the success of each treatment by age.
Fig 40:
This is a very classic case [of appendicitis].
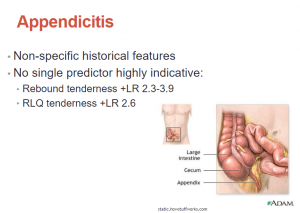
Fig 41:
So this is again, a kid with appendicitis. These are hard sometimes because there is really no single predictor that is highly indicative. You just have to develop some clinical sense of what you are seeing.
Fig 42:
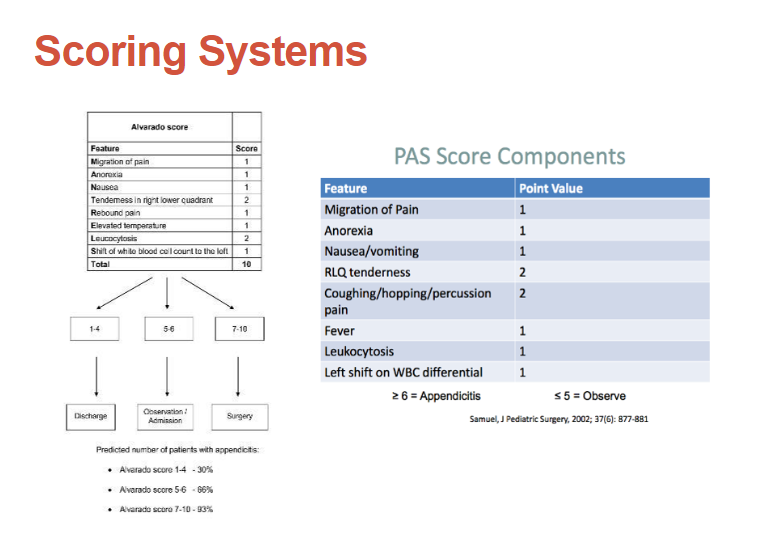
We have lots of scoring systems that we teach to use.
Fig 43:
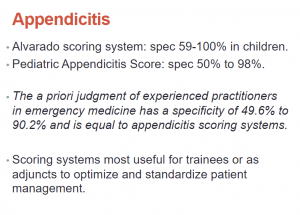
But when you look at the data, it does show that the a priori judgment of experienced practioners in emergency medicine has the same specificity and is equal to appendicitis scoring systems. So they don’t really add to how well we evaluate kids with appendicitis. It doesn’t really change our clinical suspicion very much.
Fig 44:
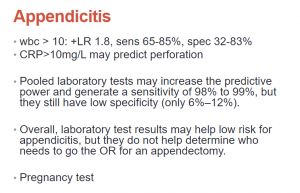
So you can look at things like the white count or the CRP. You know, if the white count is super high, it is not going to be simple appendicitis; if the CRP is elevated in a highly suspicious patient, it is more likely that it is perforated. That is sort of all we can get from laboratory tests.
Fig 45:
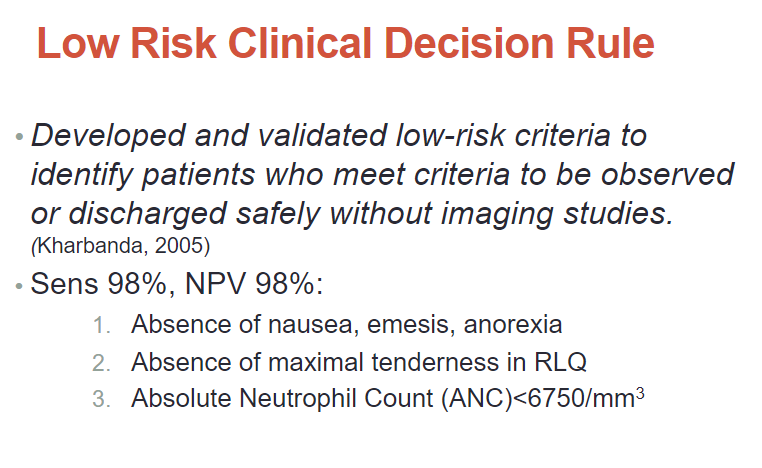
So Kharbanda published a low risk clinical decision rule to at least help us figure out who we don’t need to do anything more for.
Who are the patients that we can say clinically we’re not worried enough to do any kind of labs or imaging on.
And he was actually able to show with a sensitivity of 98% and a negative predictive value of 98% that [in patients who meet the three characteristics on the slide below] we really don’t need to feel obligated to do any sort of evaluation.
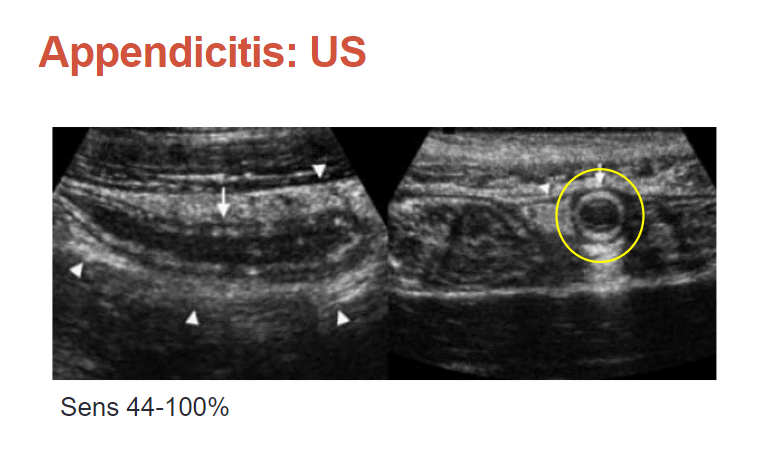
Fig 46:
The problem with ultrasound is that it is super operator dependent. So if you have experienced hands doing this, we can often get a definitive answer. If the patient has a body habitus that’s challenging or if the appendix is retrocecal, then we’re sort of stuck.
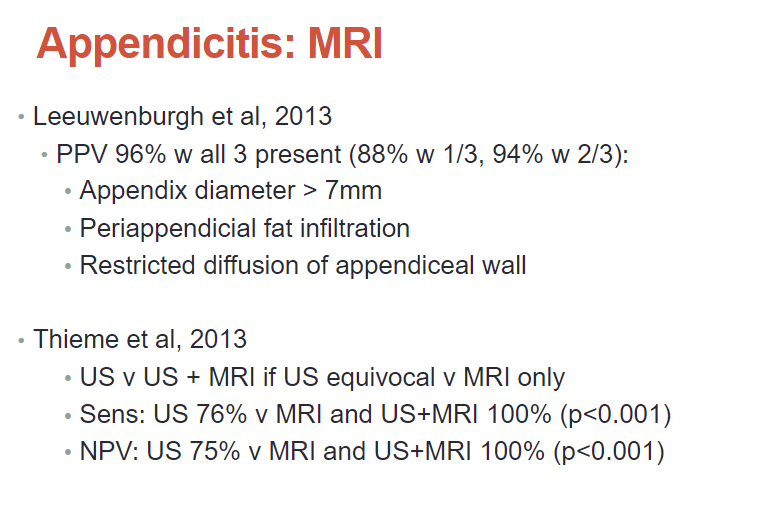
And then we move on to MRI, that’s our next choice.
Fig 47:
In our emergency department, we just do a very limited MRI of the appendix to see if we can get some more information.
Fig 48:
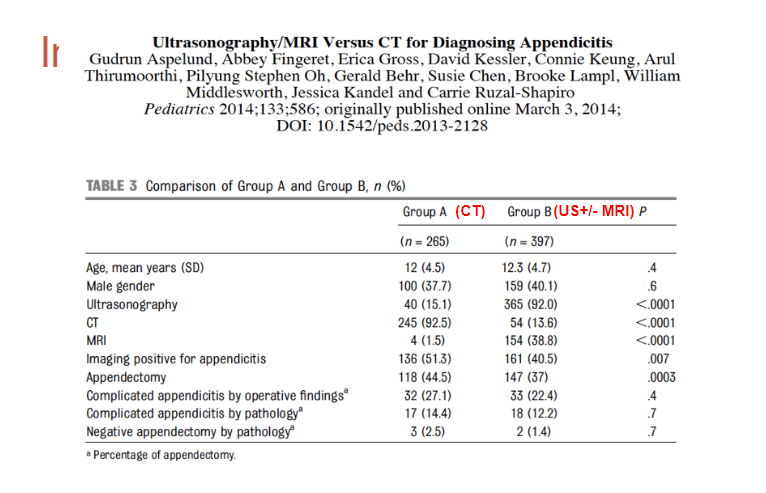
Dr. Friedlainder reminds us that we very much want to avoid doing CT scans for appendicitis on children because of the radiation. But the question was is US/+ or – MRI for diagnose of appendicitis as effective as a CT scan in diagnosis and management.
And the answer is yes according to the study in the slide below: