[Note: This blog is my peripheral brain* and thus all posts are simply my study notes and function as reminders and review to me when I need to revisit a subject. *I went to medical school before we had smart phones and tablets and so we carried a little notebook with hand written medical memory aides – a peripheral brain.]
In this post I review some of the points from Dr. Kerry’s article on Pediatric RSI. Resource (1)
Next, review my links in Resources for more on Rapid Sequence Intubation “gotchas” (because passing the tube is only a part of RSI):
Resource (2) – Pediatric Laryngoscope Blade Length Selection – YouTube Vid from Dr. Mellick + A Warning + Some Resources Posted on August 9, 2016 by Tom Wade MD.
Resource (3) – The Phsiologically Difficult Intubation – Critical Help From Drs. Weingart and Mellick Posted on September 1, 2016 by Tom Wade MD.
Resource (4) – Dr. Tim Horeczko’s podcast and show notes on Supraglottic Airways.
Resource (5) – [Pediatric] Adventures In RSI Nov 2015 by Dr. Tim Horezco
Dr. Brad Sobolowski’s interview and show notes with Dr. Kerry on Pediatric Rapid Sequence Intubation) Oct 16, 2016 is basically a podcast review of portions of Resource (1), A Modern and Practical Review of Rapid Sequence Intubation in Pediatric Emergencies.
The article covers the pitfalls of Pediatric RSI:
- The first major pitfall in the pediatric RSI process is the failure to identify a backup plan should laryngoscopy prove difficult and endotracheal tube insertion not possible.
- The second major pitfall in the pediatric RSI process is failure to adequately preoxygenate the patient.
- The third major pitfall in the pediatric RSI process is having only a single person, especially when a trainee is performing laryngoscopy, with a view of the glottis during laryngoscopy and endotracheal tube insertion. [meaning use video laryngoscopy].
- The fourth major pitfall in the pediatric RSI process is initiating laryngoscopy before the NMB taking full effect.
- The fifth major pitfall in the pediatric RSI process is the delayed recognition of a failing laryngoscopy attempt.
- The sixth major pitfall in the pediatric RSI process is prioritization of methods other than capnography/ capnometry to confirm tracheal location of the tube.
- The final major pitfall in the pediatric RSI process is the lack of a formal quality assurance and quality improvement program.
The following chart summarizes the article:
What follows are some quotes from the above article:
Although RSI is the preferred approach for the vast majority of pediatric patients, prolonged and/or failed endotracheal intubation attempts and adverse effects are common, especially in neonates and young children.8–12
In a study of RSI in a pediatric ED with more than 90 000 annual visits, endotracheal intubation was performed 147 times in a single year, with 123 of these instances representing RSI.9 Nearly two thirds of pediatric emergency medicine faculty and fellow physicians in this pediatric ED did not perform a single endotracheal intubation during the 12-month study period. 13
When the relative infrequency of pediatric RSI is coupled
with its complexity, significant risk emerges with
substantial variation in the process and threat to
patient safety.Difficult Bag Mask Ventilation
Questions to consider include the following: (1) Does the patient’s facial anatomy allow for an effective mask seal? (2) Can the jaw be easily manipulated? (3) Is the airway patent when maintained by external manual manipulation? (4) Can a few breaths be given easily with BMV?
The importance and effectiveness of achieving a mask seal using 2 hands should not be underestimated and should be the criterion standard in all cases of difficult BMV. [Emphasis added]
The basic question should be asked—Is there anything obvious to suggest that a patient’s airway will not be readily visualized with a commonly used laryngoscope?
The first major pitfall in the pediatric RSI process is the failure to identify a backup plan should laryngoscopy prove difficult and endotracheal tube insertion not possible. Fortunately, BMV is possible in most instances for pediatric patients, allowing the emergency provider time to formulate a new strategy when laryngoscopy and endotracheal tube insertion are not successful. However, if a backup plan has not been formulated before administration of the NMB and BMV proves difficult or impossible, the likelihood of patient morbidity and/or mortality significantly increases.
The rescue devices that are easiest to use in the pediatric ED patient are supraglottic airways including devices such as the laryngeal mask airway and the King laryngeal tube (Kingsystems, Nobleville, IN). Supraglottic airways have uncomplicated insertion techniques and can facilitate oxygenation and ventilation when laryngoscopy is difficult and BMV cannot be effectively performed.
ROLES DURING RSI
Because of the risk associated with task fixation and loss of situational awareness, we recommend that the provider performing laryngoscopy should not simultaneously function in the role of resuscitation team leader.
The second major pitfall in the pediatric RSI process is failure to adequately preoxygenate the patient. Children are at increased risk of rapid oxyhemoglobin desaturation and hypoxia during RSI.
Adequate preoxygenation is typically defined as 8 vital capacity breaths in a patient that can comply or 3 uninterrupted minutes of administration of the highest achievable fraction of inspired oxygen (FIO2).4 The purpose of preoxygenation is to provide an oxygen reservoir from which the patient can draw once the apneic period ensues following administration of the NMB.
There are several potential causes of inadequate preoxygenation.
First, the period of preoxygenation may be shorter than 3 minutes in duration; or significant interruptions in the continuous administration of the oxygen occur [and not be noticed by the team leader].
Second, although a high concentration of oxygen may be being administered by nonrebreathing face mask or by the application of continuous positive airway pressure using a flow-inflating anesthesia bag, the patient’s minute ventilation is inadequate to achieve optimal preoxygenation; and this goes unrecognized by the emergency provider orchestrating the RSI process.
Inadequate minute ventilation can result from an insufficient respiratory rate (eg, apnea or bradypnea) or reduced tidal volume (eg, hypopnea).
Of the 2 types of hypoventilation (apnea/bradypnea and hypopnea), hypopneic hypoventilation is likely more common and is also more challenging to recognize without the use of capnography/capnometry because the respiratory rate may appear normal by auscultation or traditional cardiorespiratory monitoring.
For preoxygenation to be effective, any patient demonstrating hypoventilation or apnea requires preoxygenation with BMV and 100% FIO2 rather than a nonrebreathing face mask or continuous positive airway pressure. [Emphasis added]
And remember that hypoventilation is likely more common than apnea/bradypnea and is harder to recognize without capnography because the respiratory rate may appear normal by ausculation or traditional cardiorespiratory monitoring.
APNEIC OXYGENATION
Once the NMB has been administered, a period of apnea ensues within approximately 30 to 60 seconds and lasts anywhere from a few minutes up to 45 minutes depending on the specific NMB administered and its associated dosing.
Apneic oxygenation represents supplemental oxygen administered via a nasal cannula that is thought to passively diffuse through the large airways to the alveoli to supplement the oxygen reservoir during the apneic period with a goal of prolonging the time before oxyhemoglobin desaturation occurs.
Although the evidence basis for clinical effectiveness is limited, apneic oxygenation is recommended by experts to delay the onset of hypoxemia.20 Specific recommendations for flow rates for apneic oxygenation have been proposed for adult patients, but evidence-based recommendations are lacking for pediatric patients. If used, we recommend 2 L/min for patients younger than 3 years, 4 L/min for those 3 to 8 years of age, and 6 L/min for those older than 8 years, although data regarding optimal flow rates are currently not available. The nasal cannula should be applied and the flow rate initiated before administration of the NMB.
Laryngoscope and Blades
The third major pitfall in the pediatric RSI process is having only a single person, especially when a trainee is performing laryngoscopy, with a view of the glottis during laryngoscopy and endotracheal tube insertion. [meaning use video laryngoscopy].
Some video laryngoscopes, such as the Storz C-MAC (Karl Storz, Tuttlingen,Germany), use laryngoscope blades almost identical in size, shape, and curvature to traditional direct laryngoscope blades, allowing the performance of direct laryngoscopy by the intubating provider while projecting the intraoral view on the video screen.
Endotracheal Tube Types and Stylets
We strongly encourage use of a blade/device that allows other providers in the room to view the laryngoscopy and endotracheal tube insertion process as a means of decreasing the risk of esophageal intubation and increasing the margin for patient safety.
[Use a cuffed endotracheal tube because] Newer evidence suggests that there is no increased risk of subglottic injury or stenosis as long as cuff pressures are monitored.30,31 The benefits of a cuffed endotracheal tube include the ability to provide higher peak inspiratory pressures often required to maintain oxygenation in patients with intrinsic lung disease and associated decreased compliance. Cuffed endotracheal tubes may also decrease the risk of aspiration.30,32–35
Although endotracheal tubes are often inserted
in the operating room setting without the presence of
a stylet, we would encourage routine use of a stylet for
pediatric emergency patients.Suction
It is prudent to prepare both Yankauer-tip suction as well as catheter-tip suction devices that may be required during laryngoscopy to clear secretions or blood. Likewise, it is wise to test the function of the suction apparatus before initiating RSI.
Premedications
Traditional RSI premedications include: (1) atropine
for the prevention of bradycardia associated
with laryngoscopy in infants and also with the
administration of succinylcholine in all young
patients and, (2) lidocaine and/or fentanyl to
mitigate potential cardiovascular and neurological
effects of laryngoscopy.The American Heart Association recommends the administration of atropine for any patient younger than 12 months and any patient younger than 5 years who will receive succinylcholine. It is also reasonable to consider atropine for any patient receiving a second dose of succinylcholine and any patient who has experienced bradycardia during the resuscitation before the initiation of the RSI process.38
As the pediatric literature is especially limited, we defer to local standard of care on the use of lidocaine or fentanyl as premedications for pediatric RSI.
Sedative Medications
If there is any doubt regarding the patient’s ability to appreciate noxious stimuli, the sedative should be used. Choice of sedative is up to the emergency provider. Table 1 displays commonly used sedative medications with their potential risks and benefits.
Neuromuscular Blocking Medications
Aside from cases of cardiac arrest, most patients will likely retain some muscle tone and protective airway reflexes, inhibiting the effectiveness of laryngoscopy and visualization of the glottic opening in the absence of the NMB. Therefore, the NMB is almost always of benefit. Table 2 displays commonly used NMBs with potential risks and benefits.
Your choices are succinylcholine or rocuronium. Succinylcholine has a lot more gotchas than rocuronium – see text. I use rocuronium.
RSI MEDICATION ADMINISTRATION
The sedative should be rapidly pushed followed by an isotonic sodium chloride solution flush; and immediately thereafter, the NMB should be rapidly pushed followed by an isotonic sodium chloride solution flush. A common error is the slow or prolonged administration of either/ both the sedative and NMB.
During pilot work for our RSI improvement initiative, we found that sedative flush– NMB flush could be completed in less than 30 seconds, which remains our standard approach.
The fourth major pitfall in the pediatric RSI process is initiating laryngoscopy before the NMB taking full effect.9 In our original study of RSI, 10% of first-attempt failures were due to the emergency provider not waiting long enough after administration of the NMB to initiate laryngoscopy. Not only is laryngoscopy more difficult in this situation secondary to the persisting muscle tone, but vomiting and aspiration may be induced if protective airway reflexes remain intact. As a result of our improvement work around RSI, we now use a timer to “force” a 45-second pause after administration of the NMB; and when this time limit is adhered to, we have nearly eliminated attempt failure due to patient movement and/or gagging.
LARYNGOSCOPY AND ENDOTRACHEAL TUBE INSERTIONThe fifth major pitfall in the pediatric RSI process is the delayed recognition of a failing laryngoscopy attempt. In the pediatric emergency department and likely anywhere children are undergoing RSI, emergency providers performing laryngoscopy and intubation may not achieve true procedural proficiency in pediatric patients largely because of inadequate experience secondary to infrequent exposure. As a result, prolonged laryngoscopy attempts are more common.
Laryngoscopy attempts lasting beyond 30 seconds are 6 times more likely, when compared with those lasting 30 seconds or less, to result in oxyhemoglobin desaturation.
In one study, investigators found that intervening at the time of desaturation to 95% prevented nearly all episodes of hypoxemia to less than 90%, whereas patients allowed to fall to 90% were likely to drop significantly below that cutoff, and several experienced associated bradycardia.50
Based on the best available evidence and the results of our improvement work, we recommend ending a laryngoscopy attempt at 45 seconds or if the oxyhemoglobin saturation approaches 90%, assuming a beginning oxyhemoglobin saturation of 100%. In both our original study and improvement work, the vast majority of patients began RSI with oxygen saturations at or near 100%. As with duration of preoxygenation and the 45-second pause after NMB administration, a timer with an audible alarm may help improve situation awareness and promote safely ending the laryngoscopy attempt at 45 seconds, especially when an authority gradient exists or is perceived to exist between the provider performing laryngoscopy and the provider supervising the RSI process.
CONFIRMATION OF ENDOTRACHEAL TUBE PLACEMENTThe sixth major pitfall in the pediatric RSI process is prioritization of methods other than capnography/ capnometry to confirm tracheal location of the tube. The confirmatory method with the strongest evidence base to confirm tracheal location is capnography/ capnometry.51,52 In our experience, teams tend to default to auscultation as the primary confirmatory method, especially during critical situations or more chaotic resuscitations. With the exception of auscultation being used to distinguish between tracheal and main stem bronchus positioning of the endotracheal tube tip, available evidence clearly supports the superiority of capnography/capnometry in determining tracheal vs nontracheal position of the tube.
In the absence of a capnography waveform and/or a reasonable capnometry value within 10 to 20 seconds of endotracheal tube placement in a patient with a perfusing rhythm, we recommend removal of the endotracheal tube and reoxygenation with BMV. Most importantly, providers should not wait for oxyhemoglobin desaturation to occur before removal of the misplaced endotracheal tube.
In our experience, video visualization, by a member of the care team in addition to the provider performing laryngoscopy, of the endotracheal tube passing through the vocal cords may be as accurate as capnography/capnometry. The combination of capnography and video visualization when available may be the ideal approach to confirmation of appropriate tube placement.
UNSUCCESSFUL ATTEMPTS
Unsuccessful laryngoscopy attempts should be expected and planned for when performing RSI, especially for children in academic settings where trainees perform laryngoscopy. Key aspects to consider include reoxygenation to optimally replete the oxygen reservoir; additional dosing of sedative and NMB, if indicated; keeping in mind the short expected duration of action of sedatives such as etomidate and NMBs such as succinylcholine; and a planned change in approach from the unsuccessful laryngoscopy attempt to optimize chances that the same result does not reoccur.
For reoxygenation, we recommend BMV to achieve the highest possible oxyhemoglobin saturation, with continued BMV for a minimum of 1 minute at the highest achievable oxyhemoglobin saturation before the next laryngoscopy attempt. The emergency provider should consider placement of an oral or nasopharyngeal airway to facilitate BMV.
If etomidate has been used as the sedative or succinylcholine as the NMB, we recommend additional doses of each if 10 minutes or more has elapsed since the initial medication administration. This time period often represents 2 unsuccessful cycles of laryngoscopy, endotracheal tube insertion attempt, and reoxygenation with BMV.
An explicit discussion of the planned change in approach from the unsuccessful attempt should occur. Potential changes to consider include adjusting positioning of the patient; selection of additional or different equipment, for example, an endotracheal tube that is 1 size smaller; switching the laryngoscopist; and a call for assistance from other airway management experts if available, such as anesthesia or otolaryngology.
IMMEDIATE POST-RSI CARE
As part of the preparatory process before laryngoscopy and endotracheal tube insertion, postintubation medications should be planned for and prepared. Key considerations include adequate postintubation sedation and continued pharmacologic paralysis if necessary. If these medications are prepared before laryngoscopy and endotracheal tube insertion, they will be readily available to facilitate securing the tube and decrease the risk of waning sedative effect while other postintubation management is performed.
Transition of the patient to the ventilator is also an important consideration. When performing BMV by hand during critical situations, there is a risk of overventilating the patient that could place the patient at increased risk in situations such as traumatic brain injury. The ventilator provides steady ventilation and optimizes oxygenation through the provision of positive end-expiratory pressure, thereby improving alveolar recruitment.
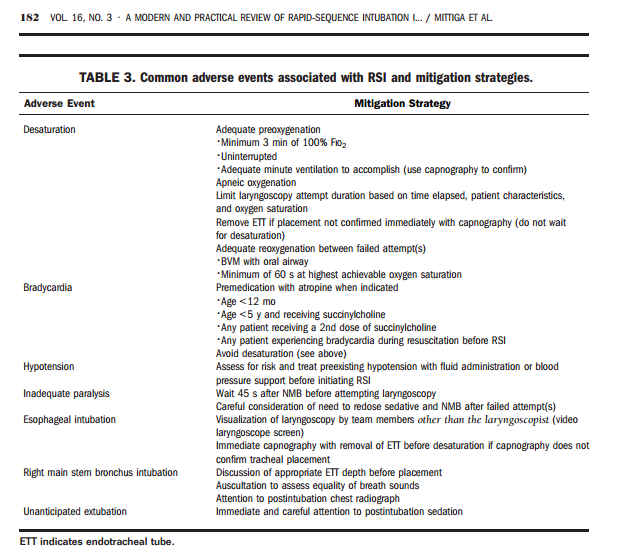
ADVERSE EVENTS ASSOCIATED WITH RSI
Table 3 [above] displays common adverse events associated with the RSI process and potential mitigation strategies.
Resources
(All that follow except Resource (2), (3), and (4) are courtesy of Dr. Ben Kerry via Dr. Brad Sobolowski’s interview and show notes with Dr. Kerry on Pediatric Rapid Sequence Intubation Oct 16, 2016.)
(1) A Modern and Practical Review of Rapid Sequence Intu bation in Pediatric Emergencies 2015.
(2) Pediatric Laryngoscope Blade Length Selection – YouTube Vid from Dr. Mellick + A Warning + Some Resources Posted on August 9, 2016 by Tom Wade MD. Resource (2)
(3) The Phsiologically Difficult Intubation – Critical Help From Drs. Weingart and Mellick
Posted on September 1, 2016 by Tom Wade MD. Resource (3)
(4) Dr. Tim Horeczko’s podcast and show notes on Supraglottic Airways from the Pediatric Playbook
(5) – [Pediatric] Adventures In RSI Nov 2015 by Dr. Tim Horeczko from the Pediatric Playbook
(6) Rapid Sequence Intubation for Pediatric Emergency Patients: Higher Frequency of Failed Attempts and Adverse Effects Found by Video Review [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Ann Emerg Med. 2012 Sep;60(3):251-9. doi: 10.1016/j.annemergmed.2012.02.013. Epub 2012 Mar 15.
(7) Response to the above article from Steve Green
(10) Preoxygenation and Prevention of Desaturation During Emergency Airway Management