I’ve divided these posts, my study notes on the European high blood pressure guidelines, into several parts for ease of my review. Links to all my post on the 2018 European Hypertension Guidelines are in Additional Resources after this post.
The following are excerpts from the Secondary Hypertension section from the 2018 ESC/ESH Guidelines for the management of arterial hypertension [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Eur Heart J. 2018 Sep 1;39(33):3021-3104. doi: 10.1093/eurheartj/ehy339:
Secondary Hypertension
Secondary hypertension is hypertension due to an identifiable cause, which may be treatable with an intervention specific to the cause. A high index of suspicion and early detection of secondary causes of hypertension are important because interventions may be curative, especially in younger patients [e.g. corrective surgery for aortic coarctation, renal angioplasty in younger patients with renal artery fibromuscular dysplasia, reversal of an endocrine cause of hypertension (e.g. by removal of an adrenal adenoma), or drug treatment of a monogenic disorder affecting a specific drug-sensitive ion channel (e.g. selective use of amiloride in Liddle’s syndrome)]. Interventions
that treat the cause of secondary hypertension later in life are less likely to be curative (i.e. remove the need for antihypertensive medication) because longstanding hypertension results in vascular and other organ damage that sustains the elevated BP, but intervention is still important because it will often result in much better BP control with less medication.The prevalence of secondary hypertension is reported to be
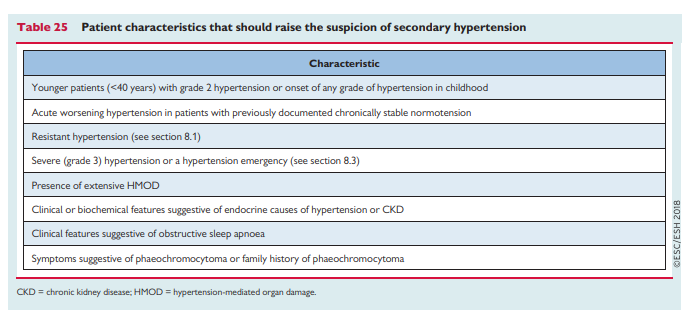
5–15%396 of people with hypertension. Screening all hypertensive patients for secondary hypertension is not feasible or cost-effective; however, there are some general patient characteristics that suggest those more likely to have secondary hypertension and in whom screening should be considered after confirming that BP is elevated with ABPM (Table 25).
It is beyond the scope of these Guidelines to describe the detailed
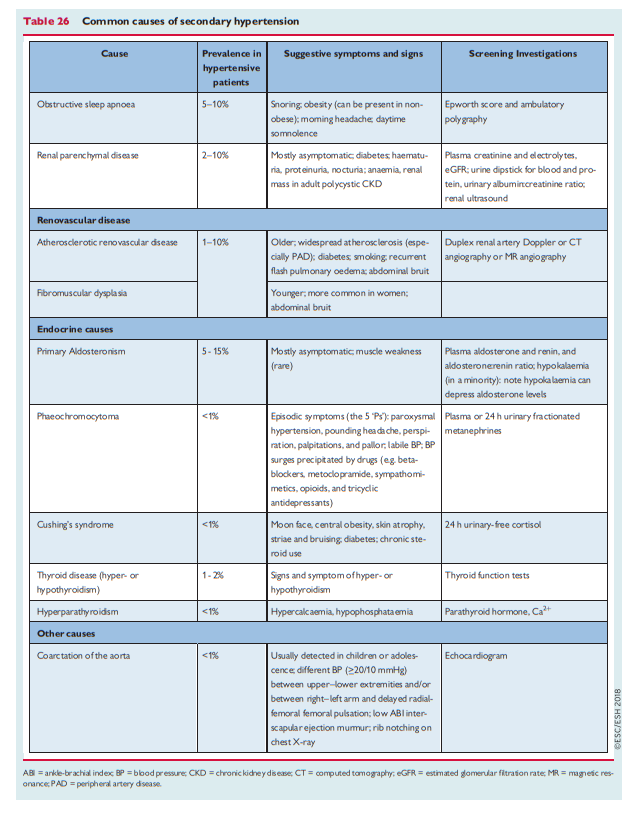
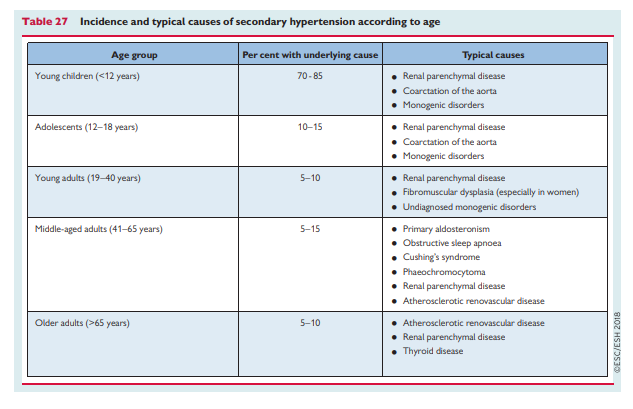
clinical management of specific causes of secondary hypertension. However, the commoner causes of secondary hypertension, clinical history, and screening tests are described in Table 26, and the typical age distribution of these causes of secondary hypertension is shown in Table 27. Review of these tables demonstrates that most screening can be undertaken with blood and urine tests, abdominal ultrasound, and echocardiography
Review of these tables [above] demonstrates that most screening can be undertaken with blood and urine tests, abdominal ultrasound, and echocardiography. Referral to a specialist centre is recommended for additional investigations to confirm a suspected diagnosis of secondary hypertension and for clinical management.
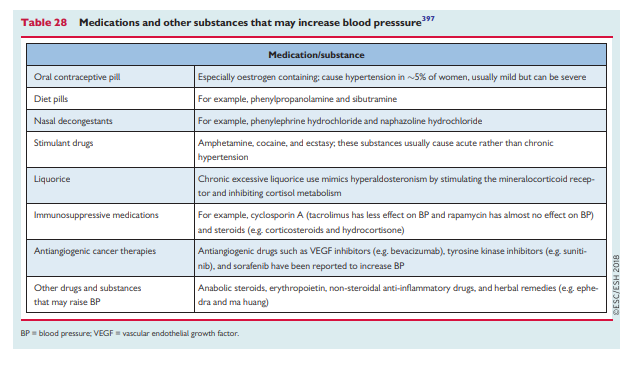
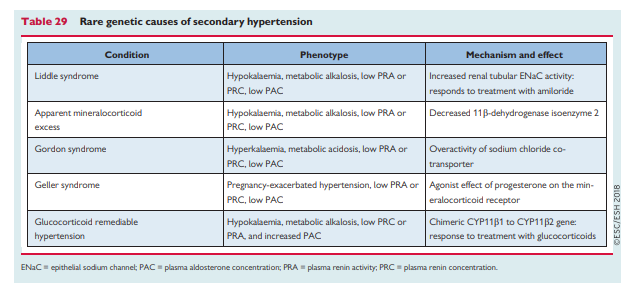
Other causes of secondary hypertension due to drugs and substances, and rarer monogenic causes, are described below and are summarized in Tables 28 and 29.