This post contains my study notes on Resource (1) below, Standards of Medical Care in Diabetes—2018 Abridged for Primary Care Providers [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Clin Diabetes. 2018 Jan;36(1):14-37. doi: 10.2337/cd17-0119.
Here are the excerpts:
This is an abridged version of the Standards containing the evidence-based recommendations most pertinent to primary care. The tables and figures have been renumbered from the original document to match this version. All of the recommendations (bulleted text) are precisely the
same as in the full Standards of Care.CLASSIFICATION AND DIAGNOSIS OF DIABETES
Diabetes can be classified into the
following general categories:1. Type 1 diabetes (due to autoimmune β-cell destruction, usually leading to absolute insulin deficiency) 2. Type 2 diabetes (due to a progressive
loss of β-cell insulin secretion frequently on the background
of insulin resistance) 3. Gestational diabetes mellitus (GDM) (diabetes diagnosed in the second or third trimester of pregnancy that was not clearly overt diabetes prior to gestation)
4. Specific types of diabetes due to other causes, e.g., monogenic diabetes syndromes (such as neonatal diabetes and maturity-onset diabetes of the young), diseases of the exocrine pancreas (such as cystic fibrosis and pancreatitis),
and drug- or chemical-induced diabetes (such as with glucocorticoid use, in the treatment of HIV/AIDS, or after organ transplantation)Diagnostic Tests for Diabetes
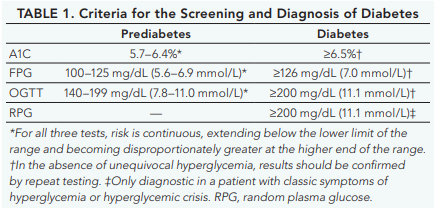
Diabetes and prediabetes may be screened based on plasma glucose criteria, either the fasting plasma glucose (FPG) or the 2-h plasma glucose (2-h PG) value during a 75-g oral glucose tolerance test (OGTT), or A1C criteria (Table 1).
There is incomplete concordance between A1C, FPG, and 2-h PG, and the 2-h PG diagnoses more people with diabetes than the FPG or A1C. Marked discrepancies between measured A1C and plasma glucose levels should prompt consideration that the A1C assay may not be reliable for that individual, since a relatively small percentage of patients have conditions such as sickle cell trait or hemoglobinopathies that skew A1C
results. See the full 2018 Standards of Care for conditions causing discrepancies. Unless there is a clear clinical diagnosis based on overt signs of hyperglycemia, a second test
is required for confirmation, either repeating the same test used initially or a different test. If patients have test results near the margins of the diagnostic threshold, the health care professional should follow the patient closely and repeat the test in 3–6 months.
Exercise in the Presence of Specific Long-term Complications of Diabetes
Retinopathy
If proliferative diabetic retinopathy or severe nonproliferative diabetic retinopathy is present, then vigorous intensity aerobic or resistance exercise may be contraindicated because of the risk of triggering vitreous hemorrhage or retinal detachment. Consultation with an ophthalmologist prior to engaging
in an intense exercise regimen may be appropriate.Peripheral Neuropathy
Decreased pain sensation and a higher pain threshold in the extremities result in an increased risk of skin breakdown, infection, and Charcot joint destruction with some forms of exercise.Autonomic Neuropathy*
Autonomic neuropathy can increase the risk of exercise-induced injury or adverse events through decreased cardiac responsiveness to exercise, postural hypotension, impaired thermoregulation, impaired night vision due to impaired papillary reaction, and greater susceptibility to hypoglycemia.
Cardiovascular autonomic neuropathy is also an independent risk factor for cardiovascular death and silent myocardial ischemia. Therefore, individuals with diabetic autonomic
neuropathy should undergo cardiac investigation before beginning physical activity more intense than that to which they are accustomed.
*See Resources (3), (4), and (5) below for articles on cardiovascular autonomic neuropathy and on autonomic neuropathy.
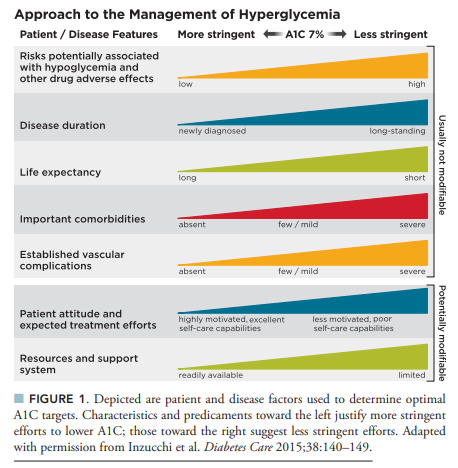
Pharmacologic Therapy for Type 2 Diabetes
For a detailed set of charts from Resource (2) below on Pharmacologic Therapy for Type 2 Diabetes, see my post, Eight Charts That Summarize “Management of hyperglycaemia in type 2 diabetes, 2018” Posted on October 14, 2018
Resources
(1) Standards of Medical Care in Diabetes—2018 Abridged for Primary Care Providers [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Clin Diabetes. 2018 Jan;36(1):14-37. doi: 10.2337/cd17-0119.
(2) Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) [PubMed Abstract] [Full Text HTML] [Full Text PDF].
(3) Cardiac autonomic neuropathy: Risk factors, diagnosis and treatment [PubMed Abstract] [Full Text HTML] [Full Text PDF]. World J Diabetes. 2018 Jan 15; 9(1): 1–24.
(4) Cardiovascular autonomic neuropathy [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Proc (Bayl Univ Med Cent). 2016 Apr; 29(2): 157–159.
(5) Autonomic Neuropathy Updated: Jun 14, 2018 from emedicine.medscape.com.