Our medical group will be using the VICTOR charts and vital sign norms for our pediatric patients. Hence this post.
The following are excerpts from Resource (1) below, Clinical Guidelines (Nursing): Observation and Continuous Monitoring from Royal Children’s Hospital of Melbourne:
1. Introduction
Regular measurement and documentation of physiological observations (i.e. clinical observations) are essential requirements for patient assessment and the recognition of clinical deterioration.
The Victorian Children’s Tool for Observation and Response (ViCTOR) charts are a set of 5 age-specific ‘track and trigger’ paediatric observation charts for use in Victorian hospitals, and are designed to assist in recognising and responding to clinical deterioration in children.
An age appropriate ViCTOR chart must be used for all inpatients at RCH. The charts are available for the following 5 age groups: less than 3 months, 3 to 12 months, 1 to 4 years, 5 to 11 years and 12 to 18 years. At RCH there are no adult charts and the 12-18 years chart should be used for young people older than 18 years.
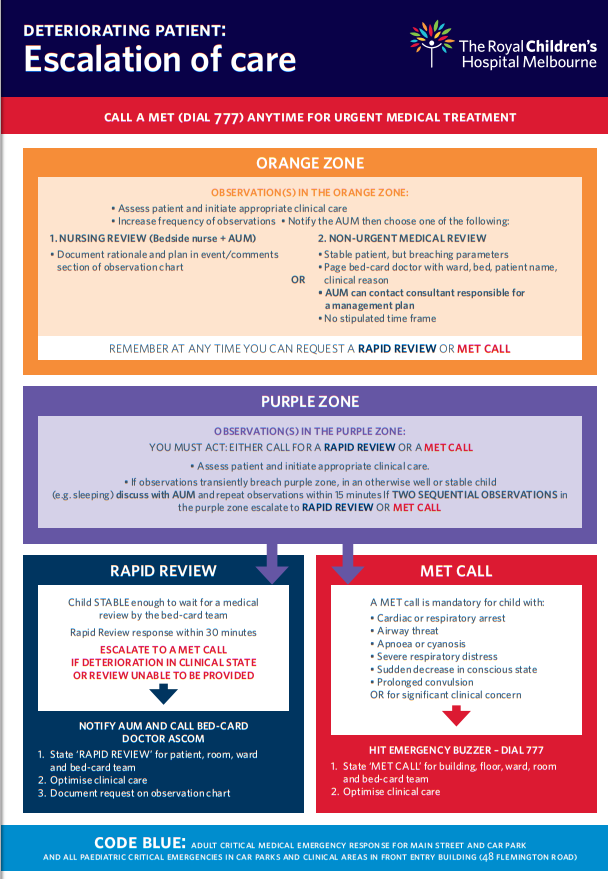
These ‘track and trigger’ charts mandate a response by the clinician once the patient’s observations reach a designated ‘zone’. Concerning changes in any one observation, or vital sign, are indicated by two coloured zones (Orange and Purple). If a child’s observation transgresses the Orange or Purple zone an escalation of care response is triggered. The type and urgency of the escalation response depends on the degree of clinical abnormality.
2. Aim
To provide guidance to clinical staff regarding the:
- Measurement of clinical observations;
- Use of the Victorian Children’s Tool for Observation and Response; and
- Role of continuous cardio-respiratory monitoring and pulse oximetry monitoring.
4. Guideline details
A. Clinical Observations
Clinical observations include estimation of haemoglobin-oxygen saturation (SpO2, pulse oximetry), oxygen delivery, respiratory rate, respiratory distress, heart/pulse rate, blood pressure (systolic, diastolic and mean), temperature, level of consciousness OR level of sedation, and a pain score. In certain clinical circumstances further observations (for example, neurological observations or neurovascular observations) may be required.
Clinical observations will be recorded by the nurse as part of an admission assessment, at the commencement of each shift and at a frequency determined by the child’s clinical status. Further guidelines about Nursing Assessment can be found here.
The frequency of observations should be documented, unless they are to be performed routinely, 4 hourly.
The type and frequency of observations must reflect the therapies and interventions being delivered to the child and be consistent with requirements of other individual guidelines and procedures. For example, required observations during blood product transfusions and all fresh blood products can be found here.
Observations should be performed at least once per hour if the patient:
- Has previous observations within the shaded orange or purple zone (unless modified)
- Was transferred from PICU/NICU (for 8 hours or as clinically indicated)
- Is receiving PCA, Epidural, or Opioid infusion
- Is receiving an Insulin infusion
- has ICP monitoring
- is receiving oxygen therapy
(Note, some children will require hourly observations and continuous monitoring as described later in this guideline).
Clinical observations must be recorded before transfer from one area to another, for example from ED to ward, PICU to ward or PACU to ward. If a child’s observations are transgressing the Orange or Purple zone, this must be addressed prior to transfer.
The nurse responsible for the child’s care will determine the type and frequency of observations based on the results of previous observations and the child’s clinical condition, and in consultation with others involved in the child’s treatment.
Because normal pediatric vitals vary with age, there are 5 different track and trigger charts depending on the pediatric patient’s age. Here is the link to Resource (2) below, Normal Ranges for Physiological Variables.
There are 5 Age Specific Track and Trigger Charts:
- Under Three Months
- 3 – 12 Months
- 1 – 4 Years
- 5 – 11 Years
- 12 – 18 Years
Click on the link Resource (3), Victorian Children’s Tool For Observation and Response (VICTOR) – ViCTOR charts & folders to see an example of each of the five individual Track and Trigger Charts.
Coloured zones
There are 3 distinct coloured ‘zones’ within the ViCTOR graph.
The White zone is considered the ‘acceptable zone’. That is, most patients trending in this area are considered to have acceptable age-related vital signs ( Normal Ranges for Physiological Variables.) Nevertheless, it is important to be vigilant – for example, a heart rate that is steadily rising in this White zone should trigger attention before crossing into the Orange zone.
The Orange zone is the first zone to signal that the patient may be deteriorating. It triggers the clinician to escalate care to the AUM (at a minimum) to decide if a medical review or other emergency response is required. The Purple zone is the second and more concerning trigger and signals that the patient may be deteriorating or is seriously ill. If the patient is in the Purple zone, an emergency call must be initiated, that is, a Rapid Review or MET call.
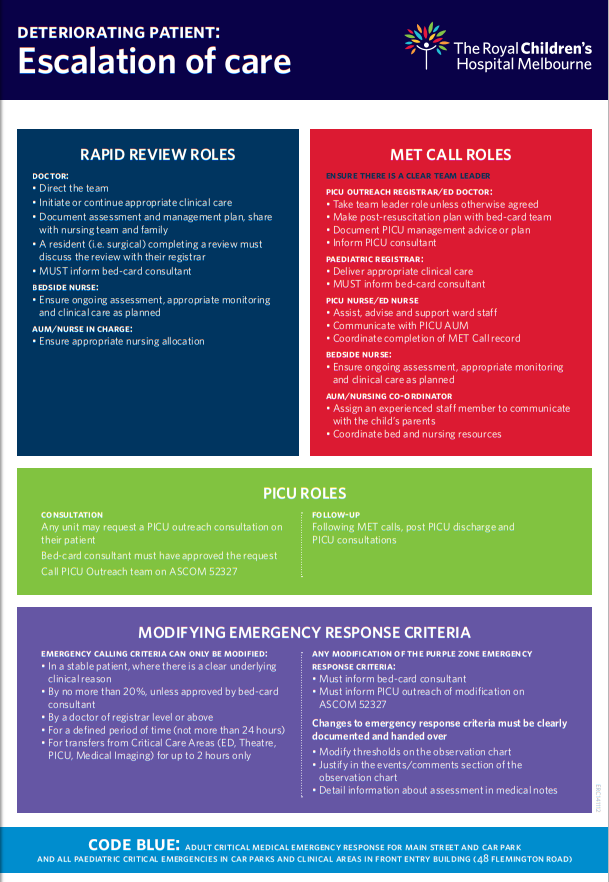
Appropriate escalation of care must occur as per the Deteriorating Patient: Escalation of Care flow chart and the Medical Emergency Response Procedure.
Remember, regardless of what zone the patient is in, if a staff member or parent is very worried about the child’s clinical state, initiate an emergency response.
O2 Saturation and oxygen delivery
Haemoglobin-oxygen saturations (SpO2) should be entered numerically in the allocated box.
Oxygen delivery refers to the flow (L/min) or percentage (%) of oxygen that the patient is receiving. If no oxygen is given, write ‘RA’ (room air).
The device used to deliver oxygen should be noted as follows:
- Nasal prongs (NP)
- Hudson Mask (HM)
- Humidified Nasal Prongs (HNP)
- High Flow Nasal Prongs (HFNP)
- Non-rebreather mask (NRM)
- Tracheostomy (T)
Oxygen delivery guidelines can be found by clicking on this web-link. Standing medical orders for alteration of oxygen therapy by nurses for patients in PICU can be found by clicking on this web link .
For children on continuous pulse oximetry monitoring, the saturation probe site should normally be re-sited every 4 hours for infants <1year (2 hourly may be necessary for some infants) and 4-6 hourly for >1year. This should be indicated on the chart.
Note: It is not recommended to secure oxygen saturation probes with CombanTM stretch compression bandage.
Respiratory rate and pulse rate
Respiratory rate and pulse rate must be entered on the flowsheet activity in EMR. In EMR, ViCTOR graphs will be automatically populated to enable review of trends.
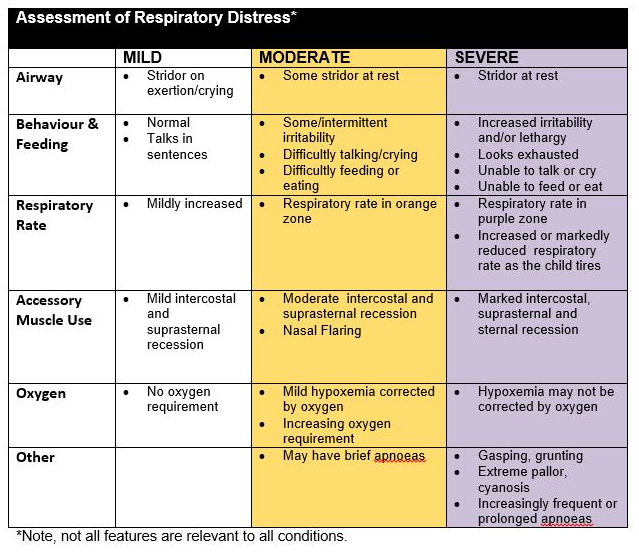
Respiratory Distress
Respiratory distress should be recorded as Nil, Mild, Moderate or Severe and be determined by assessing the following features (see www.victor.org.au)
Blood Pressure
Blood pressure (BP) must be recorded as systolic, diastolic and mean BP. Only systolic BP triggers an escalation of care response. A measurement in the Orange zone reflects hypertension (upper zone) and in the Purple zone, hypotension (lower zone).
BP should be assessed at least once on admission, and thereafter at a frequency appropriate for the child’s clinical state. If a child’s pulse/heart rate falls in the Orange or Purple zone, BP must be measured and documented.
Temperature
For infants less than 3 months, the temperature section contains an Orange zone to escalate care for the infant with a low (≤ 36°C) or high temperature (≥38.5°C).
For neonates, the temperature should be > 36.5°C ( link to Temperature Management Clinical guideline)
For other age groups, in the observation frequency section (EMR), an order can be placed when, and if an alteration in temperature should be reported to medical staff (e.g. febrile neutropenic patient, temperature rise >1°C and at least 38°C during blood product transfusion).
Level of Consciousness
Level of Consciousness assessment should be made by using the AVPU scale:
A = child is Alert (opens eyes spontaneously when approached).
V = child responds to Voice.
P = child responds to a Painful stimulus.
U = the child is Unresponsive to any stimulus.The AVPU score may be difficult to determine for infants. Some infants may respond to the voice of a parent, but not a clinician.
Children should be woken before scoring AVPU. Conversely, in an otherwise clinically stable patient, it may not be appropriate to wake a sleeping child to assess the level of consciousness, with every set of observations (e.g an infant with bronchiolitis who is on hourly observations for ongoing evaluation of respiratory distress and has just settled to sleep).
A more comprehensive neurological assessment must be performed for any patient who has, or has the potential, to have an altered neurological state. Neurological observations should be made, including an assessment of the Glasgow Coma Score, limb movements and pupils. These observations should be recorded on a separate Neurological Observation Chart.
Children who require neurological observations include those with:
- Increasing, or potential for increased, intracranial pressure
- Neurosurgical procedures
- Encephalopathy (e.g. metabolic disorder, liver failure)
- Endocrine disorders (e.g. Diabetic ketoacidosis, Diabetes Insipidus)
- Electrolyte disorders (e.g hyponatraemia)
- Demyelinating neurological conditions (e.g. Guillain – Barre syndrome)
- Seizures –consider underlying diagnosis, or new onset. AVPU scoring may be appropriate for children with pre-existing seizure conditions.
Level of Sedation
Level of Sedation assessment should be made ONLY for patients receiving sedation (e.g. chloral hydrate, midazolam, nitrous oxide, and opiates at higher doses) and the Level of Sedation score is to be used instead of the AVPU score.
The University of Michigan Sedation Score (UMSS) is used to score the Level of Sedation.
0 Awake and alert 1 Minimally sedated: may appear tired/sleepy, responds to verbal conversation +/- sound 2 Moderately sedated: somnolent/sleeping, easily roused with tactile stimulation or verbal command 3 Deep sedation: deep sleep, rousable only with deep or physical stimulation 4 Unrousable
Guidelines for procedural sedation can be found by clicking on this web-link.
Pain scores
Pain scores should be calculated by using a Pain Assessment tool appropriate for the age, developmental level and clinical state of the child. Suggested ages are as follows:
- FLACC scale for infants and toddlers and non-verbal children
- Wong-Baker Faces Scale for children 5 -17 years (may be used for some children from 3 years)
- Numeric rating scale for children >8 years.See: Nursing Clinical Guideline Pain Assessment and Measurement
Other Pain assessment tools include the neonatal Pain Assessment Tool (PAT) ( link to the Neonatal Pain Assessment clinical guideline) and COMFORT- B scale (used in PICU).
Contact the Children’s Pain Management Service (CPMS) for any pain related issues, including all children with PCA and epidural infusions.
Additional Observations
Further observations may be required.
These may include:
- Blood sugar level
- Capillary refill time
- Non-invasive ventilation parameters
- Ventilation parameters
- Isolette/radiant heater temperature ( <1 year only)
- Nausea/Vomiting
Neurovascular observations should be performed in the Neurovascular section. Further details about neurovascular observations can be found here.
The following are excerpts from Resource (3), Victorian Children’s Tool For Observation and Response (VICTOR) – ViCTOR charts & folders:
ViCTOR
ViCTOR Urgent Care
- ViCTOR Urgent Care under 3 mths
- ViCTOR Urgent Care 3 – 12 mths
- ViCTOR Urgent Care 1 – 4 yrs
- ViCTOR Urgent Care 5 – 11 yrs
- ViCTOR Urgent Care 12-18 yr
ViCTOR Neurological
ViCTOR Newborn
ViCTOR Fluid Management Charts
ViCTOR Paediatric Emergency Response Metrics Form
The following are excerpts from Resource (4) below, Deteriorating Patients: Escalation of Care from The Royal Children’s Hospital of Melbourne. The link is to two page resource on when to call for a rapid response team:
Resources:
(1) Clinical Guidelines (Nursing): Observation and Continuous Monitoring from The Royal Children’s Hospital of Melbourne.
(2) Clinical Practice Guidelines: Normal Ranges For Physiologic Variables from The Royal Children’s Hospital of Melbourne.
(3) Victorian Children’s Tool For Observation and Response (VICTOR) – ViCTOR charts & folders
Educational resources
Videos to support the implementation of ViCTOR charts can be found here
Videos describing how to take paediatric observations can be found here
(4) Deteriorating Patients: Escalation of Care from The Royal Children’s Hospital of Melbourne. The link is to two page resource on when to call for a rapid response team.