Here is the home page of The Clinical Problem Solvers.
Here is the link to the home page for Virtual Morning Report [From this link you can directly access all 572 episodes].
Here is the Clinical Problem Solvers page with the list of links to all the Diagnostic Schema.
Here is the Clinical Problem Solvers page with the list of links to all the illness Scripts.
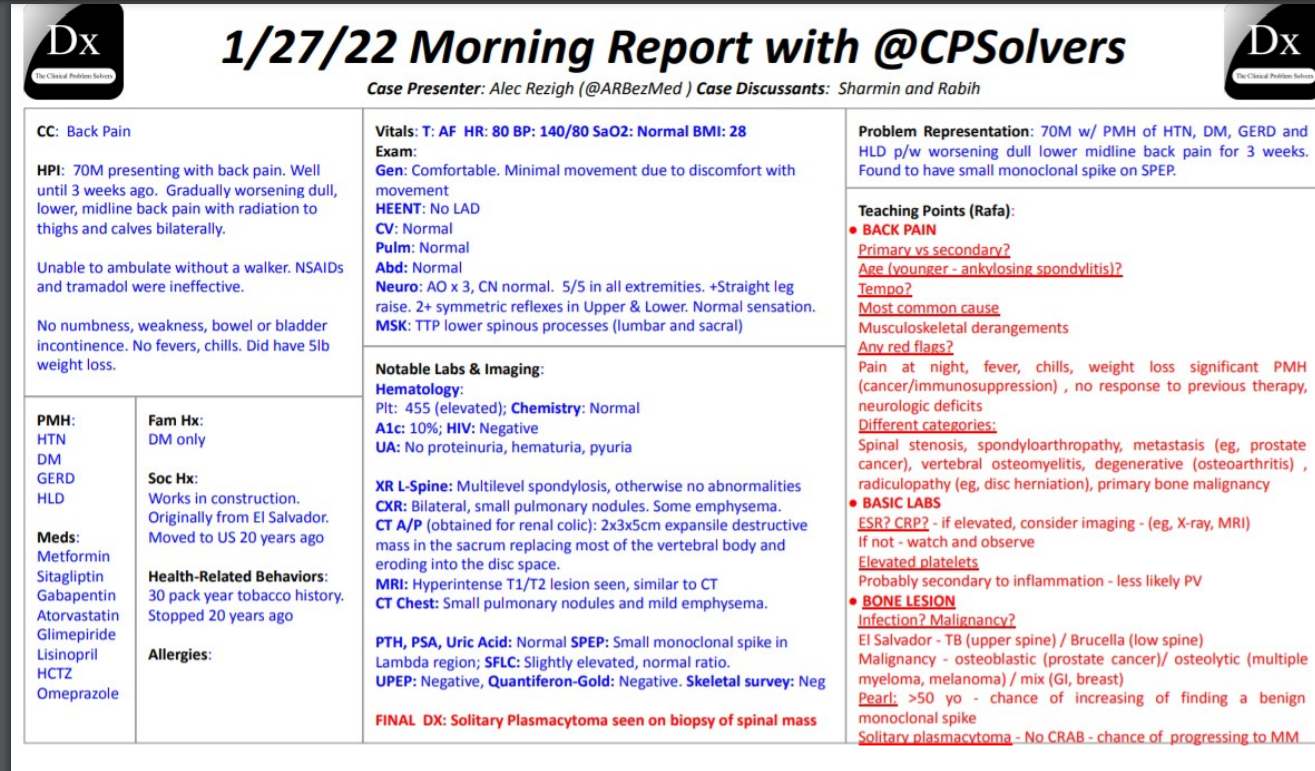
Episode 570 – Virtual Morning Report – January 27 – Back Pain [watch on the Clinical Problem Solvers website].
Case presenter – Alec Rezigh
Case overview & teaching points – Here
“Solitary plasmacytoma-No CRAB symptoms (Hypercalcemia, Renal Failure, Anemia, Bone Disease)*
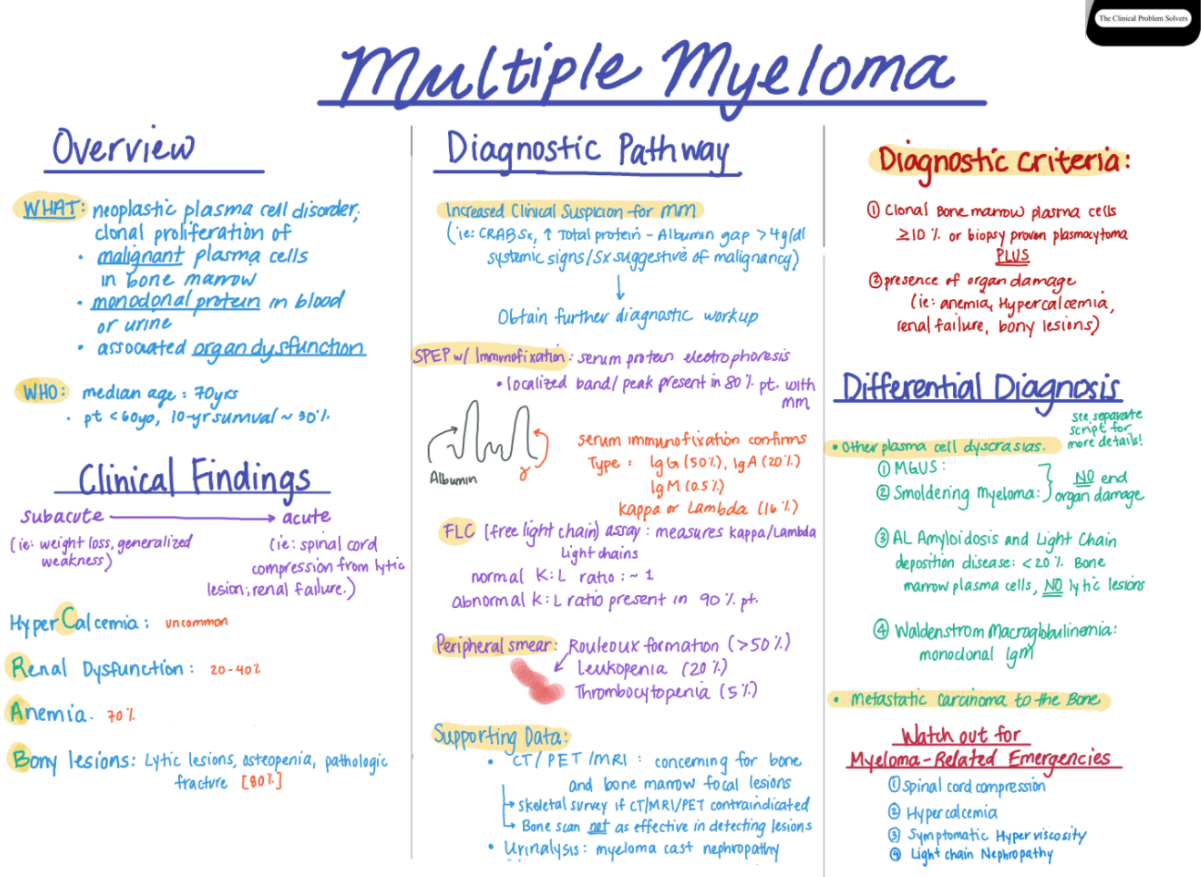
Final Diagnosis: plasmacytoma. See also Multiple Myeloma Diagnostic Criteria. Both are from emedicine.medscape.com
Diagnostic Schema:
Illness Script:
Illness Script:
Illness Script:
Diagnostic Schema:
In this post I link to and excerpt from The YouTube Clinical Problem Solvers‘ “January 27, 2022 “30-minute Thursday” VMR – back pain” [Link is to the video on YouTube]
By watching the video on YouTube, you can follow along in the transcript.
The case is of a 70-year-old patient with a 3-week history of low back pain who over the last week has to use a walker to ambulate.
All that follows is from the above outstanding resource:
The teacher states in the transcript that the emergency department physician ordered CT of abdomen and pelvis for renal colic. It is more likely that ed physician ordered them looking for abdominal, pelvic, or retroperitoneal disease causing referred back pain as the U/A was completely normal.
In all back pain patients, the question is always: Is imaging indicated (whether back pain is acute, subacute, chronic, or acute on chronic).
And if imaging is indicated, what imaging studies are needed?
From the transcript:
9:09 Two red flags of the need for imaging are overt neurologic compromise or a history of cancer.
09:18negative predictive value of an esr and09:21crp09:22in low to medium risk back pain is very09:25high so what would i do in real life for09:27this patient if his esr and crp are low09:29i would not image him and i would wait09:31to see how the disease progresses09:33everything that i am worried about and09:35that the chat has mentioned ranging from09:36infections to malignancies is associated09:39with at least minimal elevation of those09:41inflammatory markers09:42so that’s number step number one
09:45step number two09:47if a patient has a metastatic infection09:50in their back09:52you’ll find it in one of two other09:55places almost all the time09:57the first is if they have hematogenous09:59dissemination of pyogenic organisms like10:02staph and strep you’ll find it in the10:03blood so blood cultures are very10:05important10:07that presentation is less consistent10:09with three weeks of progressive back10:10pain and would be more acute what is10:12more likely here if this is infection is10:14this person has a granulomatous10:16infection10:17like tuberculosis brucella10:19and um and others10:22now where do those infections come from10:24they almost always come from the lungs.
10:26the source10:27of these infections that are granulomas10:30and go to the spine is often pulmonary10:32so this is the time to order not only10:35esr crp and basic lab but to consider10:38ordering a chest x-ray in a patient with10:40no pulmonary symptoms10:42and if he has anything on x-ray10:44the chances of something bad in his back10:46goes through the roof
10:56: All the labs were normal except the platelet count of 455. ESR and CRP were normal.
11:31in regards to imaging had a11:33x-ray of the lumbar spine11:36which showed11:37mild multi-level spondylus but no clear11:40fractures or other abnormalities11:42and then did have a chest x-ray11:45which showed some bilateral very small11:48pulmonary nodules and some mild11:50emphysema11:52didn’t have any to compare to previously
12:14 [The ed got]a ct abdomen and pelvis12:17which didn’t show any12:19gu pathology [again I think the ED got the CT looking for referred pain} but did show a two by three12:22by five centimeter12:25expansion destructive mass in the sacrum12:29that replaced most of the vertebral body12:31and eroded through the disc space12:35and12:36produced some narrowing of the epidural12:38space but no clear spinal cord12:40compression12:42and this was confirmed on mri12:47and was hyper intense12:50on12:50on imaging with t1 t2
13:15thrombocytosis or an elevated platelet13:17count is pretty robust evidence of13:18inflammation so as soon as you get that13:20data back you got to go all the way with13:22imaging, it’s very very unusual to have13:24thrombocytosis that is otherwise13:27unexplained so in real life once you get13:29that platelet count you know you need to13:30get imaging of some way shape or form13:34so here’s the what i told you might come13:35up which is how do you decide between ct13:37and mri i’ll tell you that it’s not13:39uncommon as in this case that both are13:41obtained but but if your patient doesn’t13:43have overt neurological compromise you13:46should get a ct why because it’s much13:48faster and covers much more than just13:51the cord the advantage of mri is it sees13:54the cord way better but the ct seizes13:56the bones better actually way better13:57than mri and sees the less rest of the14:00abdomen14:01so unless you are worried specifically14:02about neurological compromise i.e the14:04chord is involved you should get an mri14:05otherwise ct is faster and more more14:07extensive so here the order in which14:09things were obtained makes a lot of14:10sense
16:45um and i think you know the most common16:47scenario is when we see a bone lesion we16:49see something else so here’s the common16:51scenarios you have mass in the liver and16:52a bone lesion or you have a renal cell16:54and you have a bone lesion and so the16:56question i think in this case is what16:57happens to the probability of malignancy17:00and what kind of malignancies only show17:01up as an isolated bone lesion without17:03disease anywhere else17:05and that’s tricky because there are some17:07cancers that will just show up in the17:09bone and will show up nowhere else like17:11melanoma for example or multiple myeloma17:15and so17:16if you just know bone lesion it’s17:18probably cancer 10 times more than17:20infection but if you say17:22isolated bone lesion without evidence of17:25cancer anywhere else
17:27then it starts to narrow a little bit
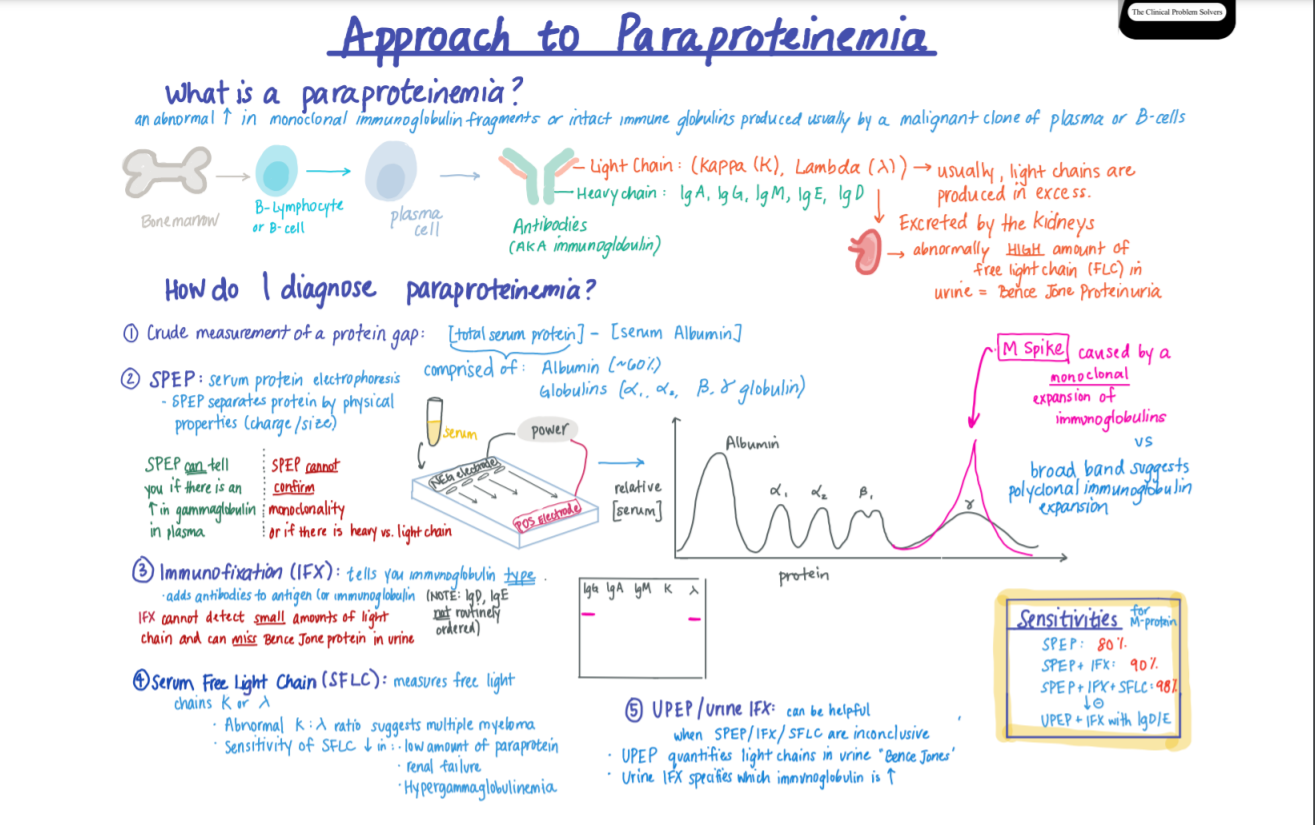
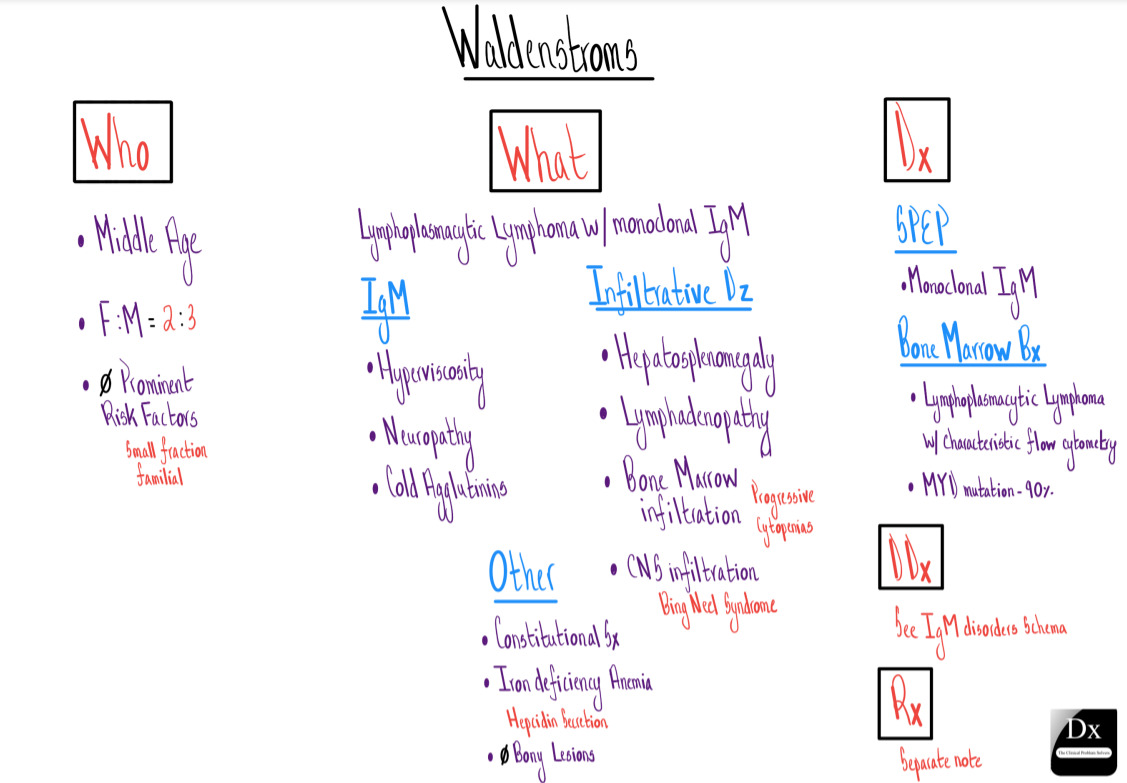
22:41but why is it not oh why if you’re an if22:44you’re a learner who’s who who isn’t22:46fully dived into the world of aspeb why22:47isn’t the answer obviously multiple22:48myeloma when you say you have a bone22:50lesion and a positive aspect and the22:52answer is that at the age of above 5022:56you have a one percent chance of having22:57an incidental monoclonal protein since23:00you because of your age and that risk23:03goes up with every decade so he has23:05about a four or five percent chance of23:06having a monoclonal spike just by being23:09alive independent of this tumor23:12what else do you make of the possibility23:14that he has no criteria of systemic23:17effects of myeloma he has no23:18hypercalcemia no renal insufficiency no23:20anemia right and so that’s where i think23:23sami’s thought in the chat is really23:25important which is does he have not so23:27much a multiple myeloma but a version of23:30multiple myeloma that’s restrictive23:32called a plasmacytoma23:34now just be clear plasmacytoma is just a23:36collection23:38of abnormal plasma cells that doesn’t23:41meet criteria for multiple myeloma23:43because it’s there’s no crab criteria23:46and there’s less than 10 plasma cells23:49and most plasmacytomas occur along with23:51multiple myeloma where there’s just a23:53focal collection of plasma cells that23:55you can see radiographically but23:57sometimes they can be solitary23:59and in solitary it’s usually exactly24:01where this patient has their24:02plasmacytoma and here’s the problem24:04seventy percent of them go on to develop24:06multiple myeloma24:08so i think with the step is a lead to24:10say it might be true true and unrelated24:12and this person may turn out to have24:14osteosarcoma or they may actually turn24:16out to have a cryptic infection that24:17presented atypically and left the lung24:19so quickly before it left a signature24:21but with the s pep it’s hard not to24:23worry about multiple myeloma or more24:25likely because of the absence of lytic24:27lesions elsewhere and the absence of24:28crab criteria that you might have a24:30solitary plasmacytoma of the bone24:33which24:34practically speaking is no different24:36than multiple myeloma because within24:37three years he has a 70 chance of24:39getting it but i love alec24:42your evaluation is very practical here24:45it doesn’t matter if you’ve got tb or24:46brazil the truth is like when there’s a24:48problem that is kind enough to declare24:50itself by showing up in one specific24:52area just look at it it’ll tell you it24:54won’t hide there are very few things of24:56biopsy negative diseases in medicine or24:58very few and so given that we’re out of25:00time i’m hopeful that this biopsy is25:02very positive which i i know you alluded25:04to so i’ll pass them like to you25:06before that i just want to say i25:09completely didn’t think about a25:11plasmacytoma so sammy rg thank you for25:15reminding me that was fantastic25:20a great discussion um and uh you guys25:22are right on the money it was the blast25:24it came back it was very consistent with25:25the solitary plasmacytoma25:27so well done sammy and and charming and25:30nrg one25:32so25:33you know25:34hematology became involved after that25:36and uh fortunately his disease was very25:38isolated just to that lesion so he got25:41some physical therapy and ended up25:43getting radiation and he’s doing much25:45much better now25:46and uh there’s gonna pardon me monitor25:49him serially and determine you know if25:51he needs any additional therapies in the25:52future but um25:54thanks for letting me present and um i25:56always learn a lot when i’m here so uh25:58awesome26:01alec26:02funny i always also learn a lot when26:05you’re here coincidence26:07i i don’t think so um thank you all so26:10so much this was an amazing case i was26:13yeah i26:14completely didn’t think about26:15plasmocytomas at all it’s been a while26:17so i know my reading for today um sammy26:21great job rafa26:23jack thanks so much for presenting and26:25rafa for being teaching points and rj26:28always a pleasure any um any reflections26:30already before we pass it to our rafa26:33for26:35well i really just want to shed light on26:37uh you know what alec is doing alec is26:39it is26:40diving into the field of clinical26:42reasoning and as a junior faculty member26:44you should know and remember his name26:46anytime clinical reasoning comes up um26:48alex you’re doing absolutely tremendous26:49work i think it’s so um awesome to see26:52you here joining us on bmr alex is26:53getting his cases out there published26:55left right and center and my hope and26:57dreams are that we get alec to be a26:59discussant um on one of either a written27:01case or here at vmware soon so27:03a27:04yeah i just want to put a plug for those27:06of you listening on youtube and those of27:08you live that before you is a um27:11evolving expert and future legend in27:13clinical reasoning and you may not27:15appreciate that um27:17but we we certainly do we’ve known alex27:19since he was a r2 right are two or three27:21i forget archery r3 yeah final year27:24residency so it’s a treat to see you27:26like climbing up the ladder and i think27:28honestly27:29um your your persona and um your27:32relentless work in clinical reasoning27:34will only lead to one destination so27:36it’s great to see it happen27:38thank you all and i’ll pass the mic to27:40rafa to take us home the other are27:43so many hours27:45so thank you all uh incredible case and27:47discussion everybody uh congratulations27:50so we have this patient with back pain27:52and regular managed to think about27:54primary versus secondary causes also27:56when it comes to age for example you27:58don’t expect like a younger male patient28:00to have chronic back pain so age for28:02example is important here because it28:04could be dealing with and closing28:05spondylitis for example tempo is very28:08important as well so we don’t expect28:09like chronic back pain in our elderly28:11patient and just be fine with that the28:13most common cause is muscular muscular28:14musculoskeletal arrangements but we have28:17to look for any red flags these include28:20things like pain at night fever chills28:22weight loss significant past medical28:24history um maybe you’re dealing with a28:27patient with a cancer or28:28immunosuppression are no response28:30purpose therapy or neurological deficits28:33and when it comes to back pain you can28:34divide in different buckets um i’d like28:36to think about spinal stenosis condole28:38arthropathy any metastasis for example28:41prostate cancer that we discussed about28:42today vertebral osteomyelitis28:45degenerative causes like osteoarthritis28:47ventriculopathy in the setting of disc28:49herniation and another thing that28:51charming reminders is to think about28:52primary bone malignancy as well when it28:55comes to the basic labs um rabby uh gave28:57us this braille that look at the spsr29:00crp if television considered imaging29:02these patients with x-ray or mri if not29:05consider watch and observe and then we29:08started this patient actually had29:09elevated the platelets and it’s probably29:12a secondary cause to the inflammation29:14process that’s going on uh primary cost29:17of thrombosis could be polystyrene29:19average but less likely because you29:21would expect to see like high hemoglobin29:23leukocytes as well and then when it29:26comes to bone lesions we thought about29:28infection and malignancy um this patient29:30was from el salvador so we thought about29:32tb and brazil under the spill that tb29:35usually29:36um leads to the upper spine involvement29:39for cell low spine involvement and when29:41it comes to malignancy for the barge we29:43usually divide that into three buckets29:45osteoblast collisions for example29:47prostate cancer oscillating collisions29:49for example nasal multiple myeloma and29:51melanoma and mixed lesions in the side29:53of chia and breast metastases and then29:56there is this barrel that i love29:59patients uh older than 50 years old30:01there’s a chance of increasing of30:02fighting a benign monoclonal spike and30:05actually this chance progresses as this30:07patient uh get older and then we saw30:10that this patient actually had of30:11solitary plasmocytoma which is basically30:13multiple myeloma less30:15a30:17the crab symptoms that we usually30:19associate with multiple myeloma like30:21hypercalcemia renal injury anemia and30:24also bone lesions but there’s this30:27chance of progressing to multiple30:29myeloma within the years so thank you30:30everyone such an educational case and i30:32hope to see everyone tomorrow30:37amazing rafa as always such a boss see30:41you all tomorrow can’t wait have a great30:44rest of your day wherever you are