The best place to start for a review of the new 2017 hypertension guidelines are these two podcasts from the American College Of Cardiology:
Eagle’s Eye View: Your Weekly CV Update From ACC.org (Week of November 13) [Link is to the podcast]:
This week’s View is part 1 of a two-part discussion of key points to remember from the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults.
Eagle’s Eye View: Your Weekly CV Update From ACC.org (Week of November 20) [Link is to the podcast]:
This week’s View is part 2 of a two-part discussion of the principles of drug therapy from the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults.
This is the fourth of nine posts extracting the highlights of the new 2017 hypertension guidelines (Resource 2). The nine posts are:
- 1 – Definition And Measurement Of High Blood Pressure – Extracts From The New 2017 Hypertension Guidelines. Posted on Nov 23, 2017
- 2 – Evaluation And Causes Of Hypertension – Extracts From The New 2017 Hypertension Guidelines. Posted on November 24, 2017
- 3 – Treatment Of Hypertension – Extracts From The New 2017 Hypertension Guidelines. Posted on November 24, 2017
- 4 – Treatment of Hypertension In Patients With Comorbidities – Extracts From The New 2017 Hypertension Guidelines. Posted on November 25, 2017
- 5 – Treatment of Hypertension In Special Patient Groups – Extracts From The New 2017 Hypertension Guidelines. Posted on November 26, 2017
- 6 – Treatment Of Resistant Hypertension – Extracts From The New 2017 Hypertension Guidelines. Posted on November 26, 2017
- 7 – Treatment Of Hypertensive Emergencies – Extracts From The New 2017 Hypertension Guidelines. Posted on November 26, 2017
- 8 – Patients Undergoing Surgical Procedures – Extracts From The New 2017 Hypertension Guidelines. Posted on November 26, 2017 – Pending
- 9 – Treatment of Hypertension To Prevent Cognitive Decline And Dementia – Extracts From The New 2017 Hypertension Guidelines. Posted on November 26, 2017
Resources
2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for
the Prevention, Detection, Evaluation, and Management of High Blood Pressure in
Adults [PubMed Citation] [Full Text PDF]. Hypertension. 2017 Nov 13. pii: HYP.0000000000000065. doi: 10.1161/HYP.0000000000000065. Epub ahead of print
2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. [PubMed Citation] [Full Text PDF].
The following are extracts from the executive summary of the 2017 Hypertension Guidelines (Resource 2):
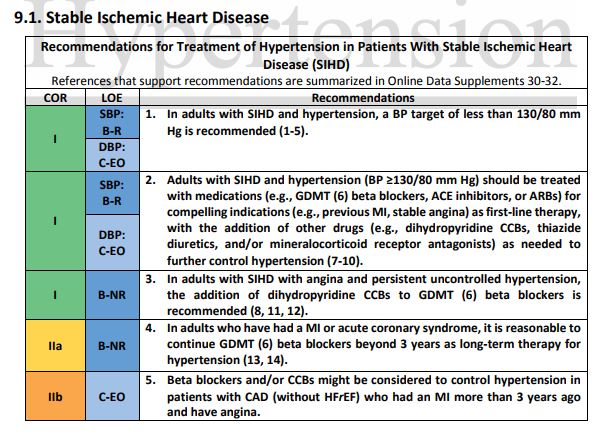
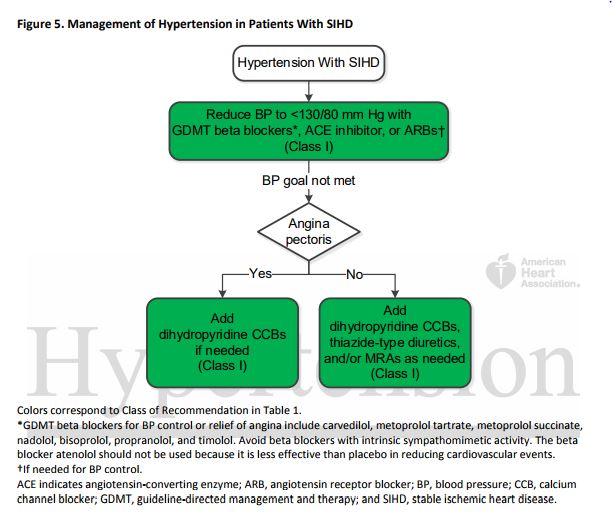
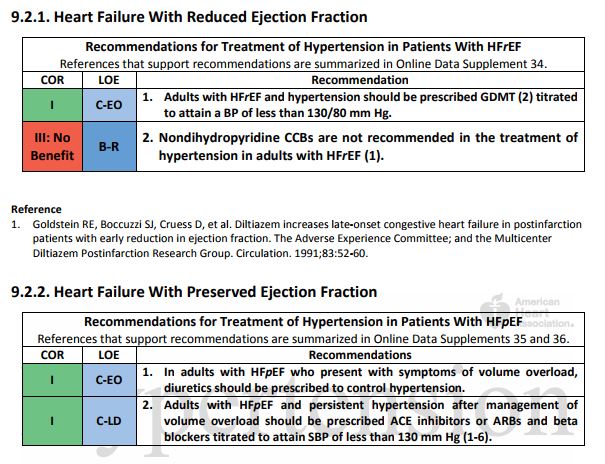
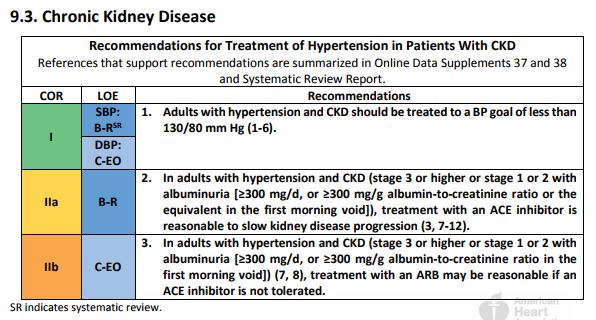
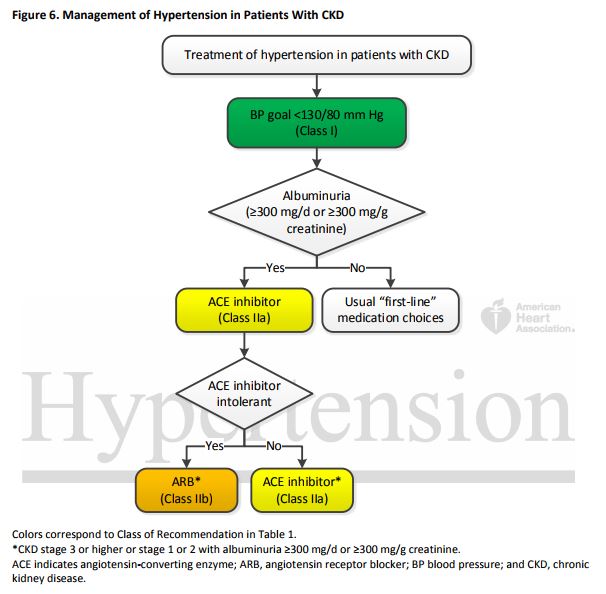
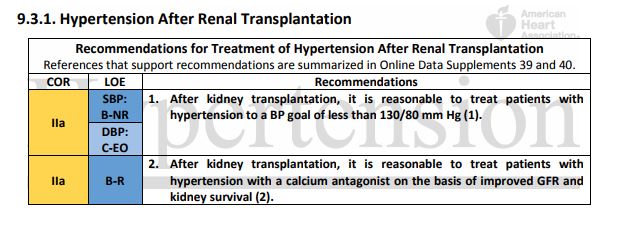
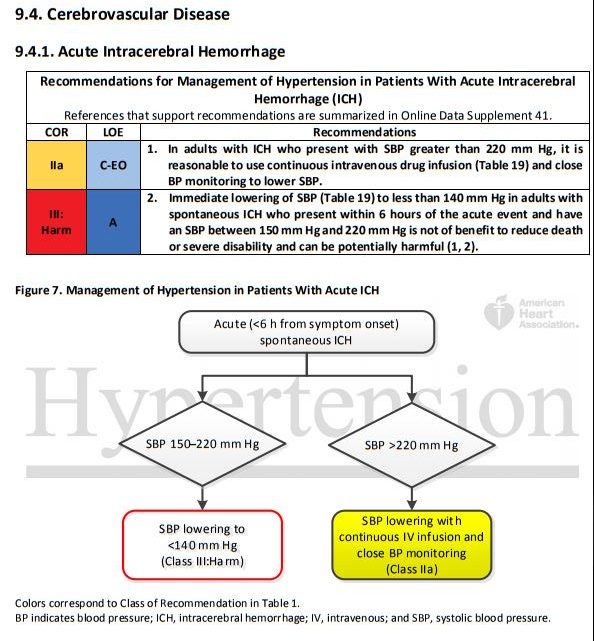
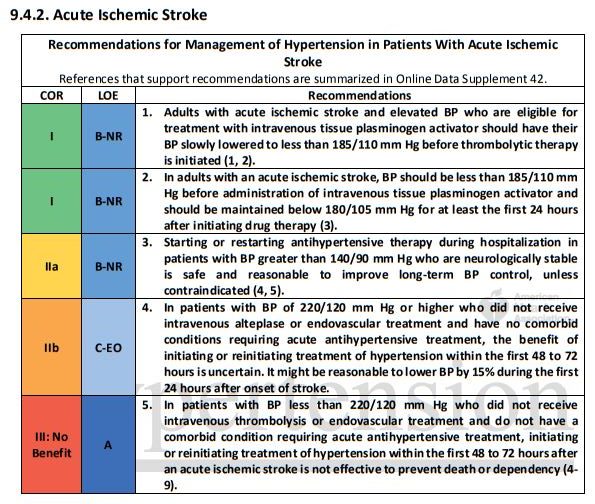
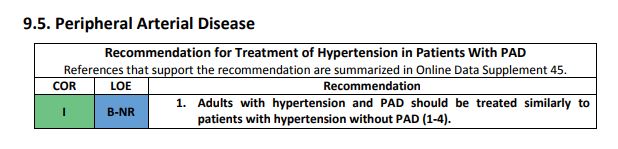
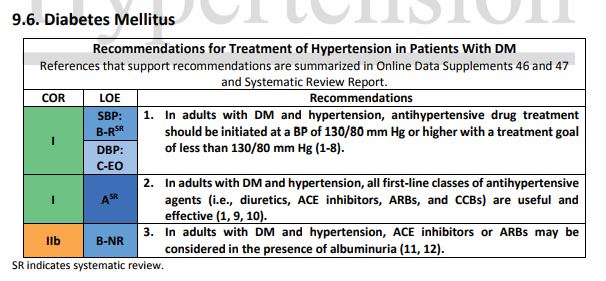
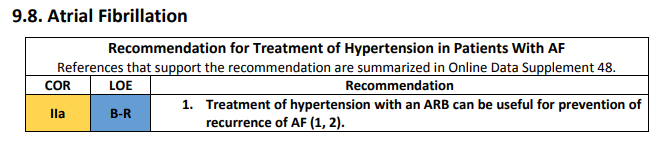
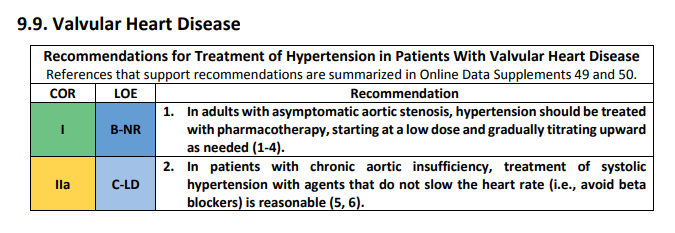
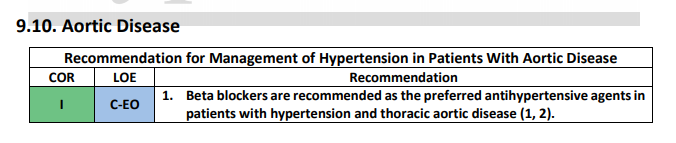
9. Hypertension in Patients With Comorbidities
Certain comorbidities may affect clinical decision-making in hypertension. These include ischemic heart disease, HF with reduced ejection fraction (HFrEF), HFpEF, CKD (including renal transplantation), cerebrovascular disease, AF, PAD, DM, and metabolic syndrome (1). As noted in Section 8.1.2, this guideline generally recommends use of BP-lowering medications for secondary prevention of CVD in patients with clinical CVD (CHD, HF, and stroke) and an average BP ≥130/80 mm Hg and for primary prevention of CVD in adults with an estimated 10-year ASCVD risk of ≥10% and an average SBP ≥130 mm Hg or an average DBP ≥80 mm Hg. Although we recommend use of the ACC/AHA Pooled Cohort Equations (https://tools.acc.org/ASCVDRisk-Estimator/) to estimate 10-year risk of ASCVD to establish the BP threshold for treatment, the vast majority of adults with a co-morbidity are likely to have a 10-year risk of ASCVD that exceeds 10%. In some instances, clinical trial confirmation of treatment in patients with comorbidities is limited to a target BP of 140/90 mm Hg. In addition, the selection of medications for use in treating high BP in patients with CVD is guided by their use for other compelling indications (e.g., beta blockers after MI, ACE inhibitors for HFrEF), as discussed in specific guidelines for the clinical condition (2-4). The present guideline does not address the recommendations for treatment of hypertension occurring with acute coronary syndromes.