Although Kawasaki Disease is the most common cause of acquired pediatric heart disease in the United States, world-wide, acute rheumatic fever is the most common cause.
Every doctor learned about Rheumatic Fever in medical school and memorized the Jones criteria for it’s diagnosis. The big change is that the new revised Jones criteria recommend using echo doppler as one of the major criteria for the diagnosis of of subclinical carditis – meaning mitral insufficency or aortic insufficiency diagnosed by echo doppler even if auscultation is normal. Reference (2)
The following is from Reference (1) below:
Rheumatic fever (RF) is a systemic illness that may occur following group A beta hemolytic streptococcal (GABHS) pharyngitis in children. Rheumatic fever and its most serious complication, rheumatic heart disease (RHD), are believed to result from an autoimmune response; however, the exact pathogenesis remains unclear. Studies in the 1950s during an epidemic on a military base demonstrated 3% incidence of rheumatic fever in adults with streptococcal pharyngitis not treated with antibiotics.[1] Studies in children during the same period demonstrated an incidence of only 0.3%. The incidence of rheumatic fever after GABHS infection is thought to be decreased to less than 1%. Cardiac involvement is reported to occur in 30-70% of patients with their first attack of rheumatic fever and in 73-90% of patients when all attacks are counted.
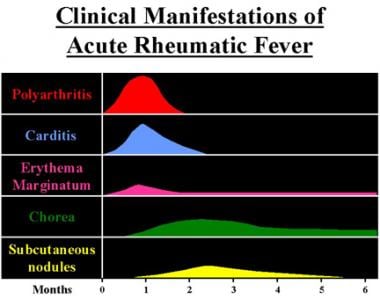
Clinical manifestations and time course of acute rheumatic fever are shown in the image below.
Acute RHD often produces a pancarditis, characterized by endocarditis, myocarditis, and pericarditis. Endocarditis is manifested as mitral and aortic valve insufficiency. Severe scarring of the valves develops during a period of months to years after an episode of acute rheumatic fever, and recurrent episodes may cause progressive damage to the valves. The mitral valve is affected most commonly and severely (65-70% of patients); the aortic valve is affected second most commonly (25%).Rheumatic fever is now uncommon among children in the United States. The incidence of rheumatic fever and RHD was thought to be decreased in the United States and other industrialized countries during the past 80 years. The prevalence of RHD in the United States was less than 0.05 per 1000 population, . . .In contrast to trends in the United States, rheumatic fever and RHD have not decreased in developing countries. Retrospective studies in developing countries demonstrate the highest figures for cardiac involvement and the highest recurrence rates of rheumatic fever.[7] Worldwide, there are over 15 million cases of RHD, with 282,000 new cases and 33,000 deaths from this disease each year.[8]The modified Jones criteria for initial acute rheumatic fever
Revised in 1992 and again in 2016, the modified Jones criteria provide guidelines for making the diagnosis of rheumatic fever.[9, 10] The Jones criteria differentiate between low risk populations (incidence of acute rheumatic fever in ≤2 per 100,000 school-aged children or all-age rheumatic heart disease prevalence of ≤1 per 1000 population per year), vs. moderate and high risk populations (where the groups may experience an incidence of 153 to 380 cases per 100,000 patients per year in the 5-14 year old age group).[11] . The new criteria also include a role for echocardiography in addition to a clinical assessment of the heart for a diagnosis of carditis. The new guidelines are in closer alignment with other international guidelines such as those from the World Health Organization.
The modified Jones criteria for initial acute rheumatic fever require the presence of 2 major, or 1 major and 2 minor criteria for the diagnosis of rheumatic fever.
The modified Jones criteria for recurrent rheumatic fever require the presence of 2 major, or 1 major and 2 minor, or 3 minor criteria for the diagnosis of rheumatic fever.
Having evidence of previous group A streptococci pharyngitis is also necessary. An exception to the requirement for evidence of previous group A streptococci pharyngitis can be made in patients with chorea and clinical or subclinical (echo diagnosis) evidence of carditis. When minor manifestations alone are present, the exclusion of other more likely causes of the clinical presentation is recommended before a diagnosis of an acute rheumatic fever recurrence is made.
Major diagnostic criteria
- Carditis-clinical and/or subclinical (echo)
- Polyarthritis (monoarthritis or polyarthralgia are adequate to achieve a major diagnostic criteria in Moderate/High-risk populations; for polyarthralgia exclusion of other more likely causes is also required)
- Chorea
- Subcutaneous nodules
- Erythema marginatum
Minor diagnostic criteria
- Fever ≥38.5o C (≥38o C to achieve a minor diagnostic criteria in Moderate/High-risk populations)
- Polyarthralgia (Monoarthralgia is adequate to achieve a minor diagnostic criteria in Moderate/High-risk populations)
- Prolonged PR interval for age on electrocardiography
- Elevated peak erythrocyte sedimentation rate during acute illness ≥60 mm/h and/or C-reactive protein ≥3.0 mg/dl
Notable exceptions to strict adherence to the Jones criteria
- Chorea: It may occur late and be the only manifestation of rheumatic fever, thus it may be impossible to document previous group A streptococci pharyngitis.
- Indolent carditis: Patients presenting late to medical attention months after the onset of rheumatic fever may have insufficient support to fulfill the criteria.
- Newly ill patients with a history of rheumatic fever, especially rheumatic heart disease who have supporting evidence of a recent GAS infection and who manifest either a single major or several minor criteria: Distinguishing recurrent carditis from preexisting significant RHD may be impossible.
Evidence of previous GAS pharyngitis (One of the following must be present):
- Positive throat culture or rapid streptococcal antigen test
- Elevated or rising streptococcal antibody titer (anti-streptolysin O titer or anti-DNASEB)
Major clinical manifestations
- Arthritis
- Polyarthritis is the most common symptom and is frequently the earliest manifestation of acute rheumatic fever (70-75%).
- Characteristically, the arthritis begins in the large joints of the lower extremities (ie, knees, ankles) and migrates to other large joints in the lower or upper extremities (ie, elbows, wrists).
- Affected joints are painful, swollen, warm, erythematous, and limited in their range of motion. The pain is out of proportion to clinical findings.
- The arthritis reaches maximum severity in 12-24 hours and persists for 2-6 days (rarely more than 4 wk, but has been reported to persist 44 d) at each site and is migratory but not additive.
- The arthritis responds rapidly to aspirin, which decreases symptoms in affected joints and prevents further migration of the arthritis.
- Polyarthritis is more common and more severe in teenagers and young adults than in younger children.
- Patients suffering multiple attacks may exhibit destructive arthritis (Jaccoud arthritis).
- Carditis
- Pancarditis is the most serious complication and the second most common complication of rheumatic fever (50%).
- In advanced cases, patients may experience of dyspnea, mild-to-moderate chest discomfort, pleuritic chest pain, edema, cough, or orthopnea.
- Upon physical examination, carditis is most commonly revealed by a new murmur and tachycardia that is out of proportion to the fever. New or changing murmurs traditionally have been considered necessary for a diagnosis of rheumatic valvulitis. The murmurs of acute rheumatic fever are from valve regurgitation, and the murmurs of chronic rheumatic fever are from valve stenosis.
- Congestive heart failure (CHF) may develop secondary to severe valve insufficiency or myocarditis. Physical findings associated with heart failure include tachypnea, orthopnea, jugular venous distention, rales, hepatomegaly, a gallop rhythm, and peripheral swelling and edema. A pericardial friction rub indicates that pericarditis is present. Increased cardiac dullness to percussion, muffled heart sounds, and a paradoxical pulse are consistent with pericardial effusion and impending pericardial tamponade. Confirm this clinical emergency with ECG, and evacuate the effusion by pericardiocentesis if it is producing hemodynamic compromise.
- In the newest version of the revised Jones Criteria morphologic and Doppler findings on echocardiogram may supersede auscultatory findings for carditis. Acute morphologic changes in the mitral valve may include annular dilation, chordal elongation, chordal rupture resulting in flail leaflet with severe mitral regurgitation, or prolapse or beading/nodularity of the leaflet tips. Doppler findings should demonstrate regurgitation in at least 2 views, with a pansystolic jet in at least 1. Chronic changes in the mitral valve should show leaflet thickening and calcification, with restricted motion. There may also be evidence of chordal thickening and fusion. Changes in the aortic valve may include prolapse, coaptation defect, and thickening of the leaflets, with restricted motion. Doppler findings should demonstrate regurgitation in at least 2 views, with a pansystolic jet in at least 1.
- Chorea: In the absence of a family history of Huntington chorea or findings consistent with systemic lupus erythematosus, the diagnosis of acute rheumatic fever is almost certain. A long latency period exists between streptococcal pharyngitis (1-6 mo) and the onset of chorea, and a history of an antecedent sore throat frequently is not obtained. Patients with chorea often do not demonstrate other Jones criteria. Chorea is slightly more common in females than males. Chorea is also known as rheumatic chorea, Sydenham chorea, chorea minor, and St Vitus dance.
- Poststreptococcal movement disorders
- Described poststreptococcal movement disorders have included pediatric autoimmune neuropsychiatric disorder associated with streptococcal infections (PANDAS) and Tourette syndrome.
- Daily handwriting samples can be used as an indicator of progression or resolution of disease. Complete resolution of the symptoms typically occurs, with improvement in 1-2 weeks and full recovery in 2-3 months; however, incidents have been reported in which symptoms wax and wane for several years.
- The PANDAS disorder appears to have a relapsing-remitting symptom complex characterized by obsessive-compulsive personality disorder. Patients with Sydenham chorea and obsessive-compulsive symptoms tend to show aggressive, contamination, and somatic obsessions and checking, cleaning, and repeating compulsions. Neurologic abnormalities include cognitive defects and motoric hyperactivity. The symptoms may also include emotional lability, separation anxiety, and oppositional behaviors, and they are prepubertal in onset.
- Some have proposed that the streptococcal infection triggers the formation of antibodies that cross-react with the basal ganglia of genetically susceptible hosts in a manner similar to the proposed mechanism for Sydenham chorea and causes the symptom complex.
- Erythema marginatum: This characteristic rash, also known as erythema annulare, occurs in 5-13% of patients with acute rheumatic fever. Erythema marginatum begins as 1-cm to 3-cm diameter, pink-to-red nonpruritic macules or papules located on the trunk and proximal limbs but never on the face. The lesions spread outward to form a serpiginous ring with erythematous raised margins and central clearing. The rash may fade and reappear within hours and is exacerbated by heat. Thus, if the lesions are not observed easily, they can be accentuated by the application of warm towels, a hot bath, or the use of tangential lighting. The rash occurs early in the course of the disease and remains long past the resolution of other symptoms. Erythema marginatum (shown in the image below) has also been reported in association with sepsis, drug reactions, and glomerulonephritis.
The tricuspid valve is deformed in only 10% of patients, almost always in association with mitral and aortic lesions, and the pulmonary valve is rarely affected. Severe valve insufficiency during the acute phase may result in congestive heart failure (CHF) and even death (1% of patients). Whether myocardial dysfunction during acute rheumatic fever is primarily related to myocarditis or is secondary to CHF from severe valve insufficiency is not known. When pericarditis is present, it rarely affects cardiac function or results in constrictive pericarditis.Chronic manifestations occur in adults with previous RHD from residual and progressive valve deformity. RHD is responsible for 99% of mitral valve stenosis in adults, and it may be associated with atrial fibrillation from chronic mitral valve disease and atrial enlargement
Resources:
(1) Pediatric Rheumatic Fever Updated: Jun 28, 2016 from reference.medscape.com
(2) Revision of the Jones Criteria for the Diagnosis of Acute Rheumatic Fever in the Era of Doppler Echocardiography: A Scientific Statement From the American Heart Association [PubMed Abstract] [Full Text HTML] [Download Full Text PDF]. Circulation. 2015 May 19;131(20):1806-18.