In this post, I link to and excerpt from Dr. Josh Farkas’ Internet Book Of Critical Care [Link is to the Table of Contents] chapter, ARDS*, Sept. 28, 2021.
*Note to readers: I excerpt from resources that I review because doing so helps me to fix the information in my memory. My excerpts omit much important information, so you should review Dr. Farkas’ chapter directly.
All that follows is from the above resource.
CONTENTS
- Rapid Reference
- Diagnosis of ARDS
- Why is the patient in ARDS?
- ARDS pathophysiology: Intrapulmonary shunting
- Treatment: Basics
- Treatment: Non-intubated patient
- Treatment: Intubated patient
- Podcast
- Questions & discussion
- Pitfalls
rapid reference
intubated ARDS patient: therapeutic package
investigate & treat underlying cause (more)
Often the most important intervention!
steroid (more)
- Consider if PaO2/FiO2 <200 mm (27 kPa) & no contraindication.
- Avoid if the cause of ARDS is known & steroid-unresponsive.
- Possible regimen: dexamethasone 20 mg qd x5d, then 10 mg qd x5d.
conservative fluid strategy (more)
- If volume overloaded or recently fluid-loaded, consider diuresis.
- If euvolemic, target even or slightly negative balance.
lung-protective ventilation (more)
- Usually volume-cycled ventilation utilized (although APRV is another option).
- Tidal volume 6 cc/kg to start:
- May reduce to 4 cc/kg if needed to keep plateau <30 cm.
- May increase to 8 cc/kg if difficulty tolerating & plateau <30 cm.
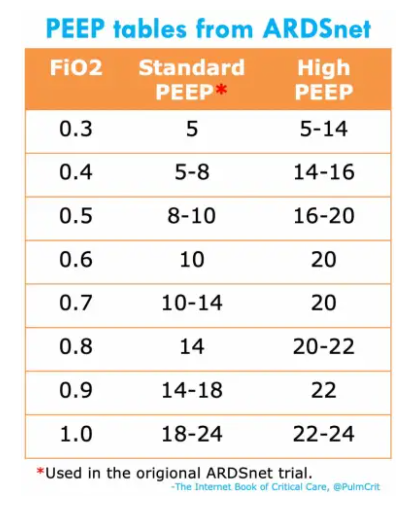
- Consider high PEEP table if P/F is <200 mm (27 kPa), or in morbid obesity.
permissive hypercapnia (more)
- Target pH roughly >~7.2 (unless elevated ICP or RV failure).
- Treat any metabolic acidoses.
- Consider IV bicarbonate to increase the bicarbonate to ~30-35 mM (if needed to achieve adequate pH without lung-injurious ventilation).
adequate multimodal analgosedation
- Typical regimen might include:
- Moderate propofol infusion.
- Opioid boluses PRN.
- Atypical antipsychotic.
- Pain-dose ketamine gtt.
- Scheduled acetaminophen.
- Propofol and opioid will reduce respiratory drive and improve ventilator synchrony (but avoid prolonged high-dose exposure to these agents).
- (More on sedation & analgesia.)
proning (more)
- Consider after >12 hours of optimization on ventilator.
- Indicated if PaO2/FiO2 <150 mm (20 kPa) and FiO2 ≧0.6 and no contraindications.
nutrition (more)
- Start early enteral nutrition (even if proned and/or paralyzed).
definition of ARDS
Start here