In this post, I excerpt from Dr. Josh Farkas’ Internet Book Of Critical Care [link is to the Table Of Contents] chapter, IBCC – SCAPE (Sympathetic Crashing Acute Pulmonary Edema) *, Sept 21, 2021.
*Note to myself and my readers: I excerpt from resources that I review because doing so helps me to fix the information in my memory. My excerpts omit much important information, so you should review Dr. Farkas’ chapter directly.
All that follows is from the above resource.
SCAPE (Sympathetic Crashing Acute Pulmonary Edema) is a specific form of severe heart failure which is seen predominantly in the emergency department and intensive care unit (as opposed to the outpatient cardiology clinic). Consequently, there is a tendency to overlook SCAPE in articles and chapters about heart failure.
SCAPE is critical to recognize and intervene upon, because it is a vicious cycle. Left alone, it will tend to worsen and ultimately precipitate intubation. However, with aggressive management, the vicious cycle can be reversed – leading to a prompt and satisfying clinical improvement.
CONTENTS
- Rapid Reference
- SCAPE vs subacute pulmonary edema
- Diagnosis
- Triggers of SCAPE
- Principles of treatment
- Podcast
- Questions & discussion
- Pitfalls
rapid reference
SCAPE dx & rx checklist
central clinical findings of SCAPE (more)
- Rapid onset of severe dyspnea.
- Hypoxemia.
- Hypertension (SBP >160 mm and/or MAP > 120 mm).
- Diffuse rales (sometimes with pink frothy sputum).
- POCUS shows diffuse B-lines.
rx #1: CPAP/BiPAP (more)
- Either works fine (the key is a high expiratory pressure).
- Rapidly uptitrate pressures, to target:
- CPAP of ~15-18 cm.
- BiPAP of ~18/15 cm.
- If not tolerated, consider IV fentanyl.
rx #2: nitroglycerine (more)
- (1) Bolus of 1,000-2,000 mcg over ~2 minutes (e.g., 400-800 mcg/min for 2.5 min).
- (2) Start infusion at ~100-300 mcg/min.
- (3) Aggressively uptitrate to 800 mcg/min if needed, targeting Bp reduction (SBP <~140 mm).
- (4) After SCAPE episode breaks, aggressively wean down nitroglycerine to avoid hypotension.
rx #3: if refractory hypertension (more)
- Rapid reduction in Bp is essential (e.g., SBP <~140).
- CPAP/BiPAP plus nitroglycerine infusion are usually adequate. If not, then consider:
- (#1) Clevidipine gtt (preferably) or nicardipine gtt.
- (#2) Enalaprilat, 1.25 mg IV (may repeat q15 minutes to a maximal dose of 5 mg).
- (#3) Low-dose fentanyl (if uncontrolled pain or air hunger).
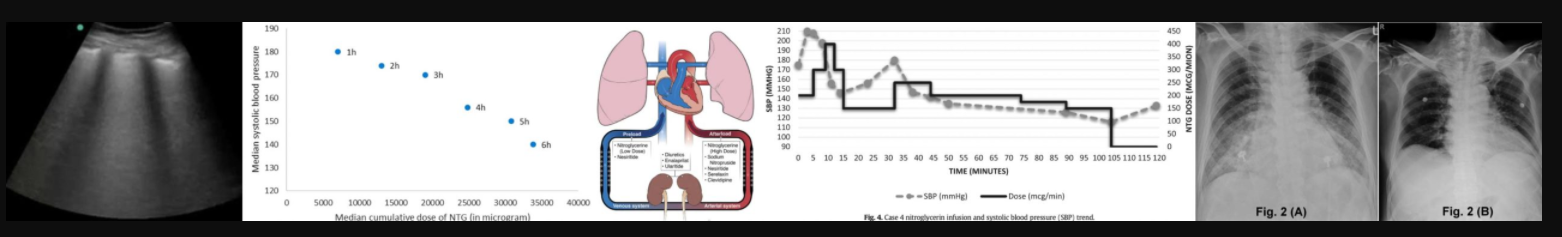
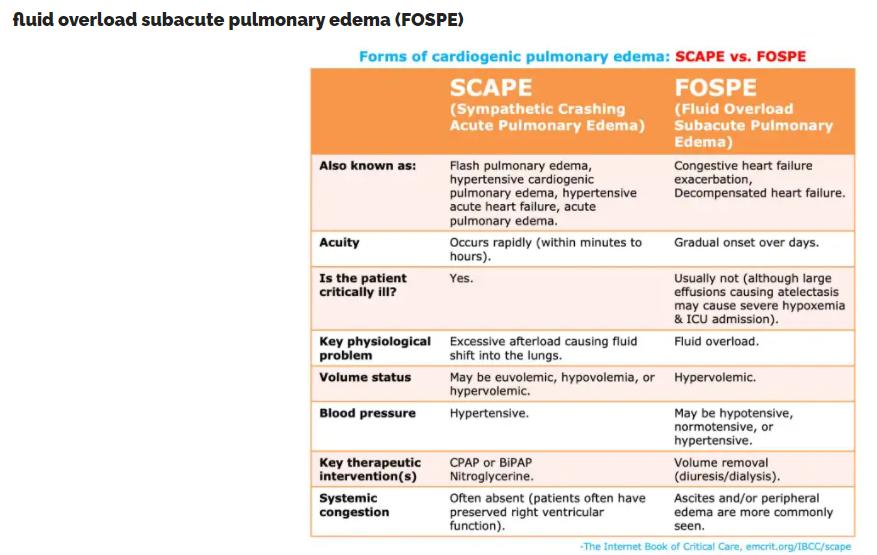
SCAPE vs subacute pulmonary edema
- SCAPE occurs due to a vicious spiral involving increasing sympathetic outflow, excessive afterload, and progressively worsening heart failure. Since SCAPE is a vicious spiral, this may develop very rapidly (hence the terminology “flash pulmonary edema”). With aggressive therapy, it may resolve very rapidly as well.
- The central, defining pathophysiological feature of SCAPE is pathologically elevated afterload due to systemic vasoconstriction and hypertension.
- SCAPE patients may be euvolemic or hypovolemic. The problem is a shift of fluid into the lungs, rather than hypervolemia.
- FOSPE occurs in patients who develop gradual volume overload. This is compared with SCAPE in the table above.
- SCAPE and FOSPE aren’t mutually exclusive. For example, some patients can have SCAPE superimposed upon FOSPE (i.e., gradual volume accumulation over time, which eventually reaches a tipping point and triggers an acute episode of SCAPE). Some authors have proposed that SCAPE and FOSPE represent two extreme forms of pulmonary edema, with some patients lying in between.(29478124)
- Differentiating SCAPE vs. FOSPE is clinically important, because the treatment is different.
nomenclature
- SCAPE is known by a variety of different terms throughout the scientific literature, most notably:
- Flash pulmonary edema (this is becoming less popular).
- Hypertensive acute heart failure (preferred terminology in hypertension journals).
- SCAPE (increasingly utilized in emergency medicine and critical care journals).
- SCAPE is currently the preferred terminology, since it is clear and unique.
- SCAPE patients often meet the criteria for “hypertensive emergency” (i.e., severe hypertension plus target organ dysfunction). However, SCAPE represents a unique entity which requires uniquely tailored therapy. For example, SCAPE develops very rapidly so patients can be promptly lowered to their baseline blood pressure (unlike many patients with hypertensive emergency, who have more gradual elevation of blood pressure and consequently require a more gradual therapeutic reduction). More on hypertensive emergency here.
diagnosis
defining clinical features of SCAPE (34215472)
- Rapid onset of respiratory distress (e.g., usually within <6 hours).
- Marked tachypnea and dyspnea.
- Hypoxemia.
- Hypertension (generally SBP>160 mm and/or MAP>120 mm).(31327485, 29776826)
- Diffuse rales on auscultation.
- Pink, frothy sputum may be seen.
- Clinical features of sympathetic activation:
- Diaphoresis, pallor, appearing extremely unwell.
- Tachycardia.
- Agitation.
- Patients may have a history of recurrent episodes of SCAPE.
POCUS
- Aside from history and examination, POCUS is the most powerful tool for the diagnosis of SCAPE.
- Lung sonography:
- Cardiogenic pulmonary edema generates a pattern of diffuse B-lines throughout the chest, with a thin pleural interface (unlike non-cardiogenic pulmonary edema, which often causes a patchy distribution of B-lines and a thickened pleural interface including patches of subpleural consolidation). Small bilateral pleural effusions may further support the diagnosis of cardiogenic pulmonary edema.
- Ultrasonography is extremely sensitive for cardiogenic pulmonary edema. If a diffuse pattern of B-lines is not seen in a patient with acute dyspnea, cardiogenic pulmonary edema may be immediately and confidently excluded as the cause of the patient’s dyspnea.
- Cardiac ultrasonography should generally reveal some form of heart failure, for example:
- Systolic heart failure, with reduced left ventricular ejection fraction.
- Diastolic heart failure may be suggested by left ventricular hypertrophy and a dilated left atrium.
Note that SCAPE patients may be hypovolemic, hypervolemic, or euvolemic. Therefore, the IVC will not necessarily be distended (nor will the patient necessarily have distended jugular veins).
chest X-ray
- Chest X-ray may also be used as a diagnostic tool. However, X-ray is less sensitive for acute pulmonary edema compared to thoracic ultrasonography. Some patients with SCAPE may not have an unequivocally abnormal chest X-ray.
- Chest x-ray findings may include:
- Bilateral, fluffy infiltrates centered in the hila (“bat wing pulmonary edema”).
- Kerley B lines (fluid in the interlobular septa causing fine lines perpendicular to the pleura).
- Pleural effusion(s).
- Lack of an alternative diagnosis (e.g., absence of pneumothorax or lobar pneumonia).
diagnostic pitfall: other forms of respiratory distress cause hypertension
- Any form of severe respiratory failure may lead to distress and hypertension. Therefore, don’t assume that the combination of respiratory failure plus hypertension necessarily implies a diagnosis of SCAPE.
- In uncertain situations, it is reasonable to initiate treatment for SCAPE while simultaneously investigating for other problems.
- One of the hallmarks of SCAPE is rapid improvement with therapy. For patients who aren’t turning around rapidly, evaluate carefully for alternative or additional problems, for example:
- Wrong diagnosis (patient has ARDS, not cardiogenic pulmonary edema).
- Underlying problem (cardiogenic edema is due to acute STEMI or valvular regurgitation)
brain natriuretic peptide (BNP)
- There is no evidence that BNP testing adds clinical information above and beyond the combination of clinical judgement and POCUS for patients with heart failure.(29887195) This is particularly true of SCAPE patients, wherein the diagnosis is generally not subtle.
- Pragmatically, the turn-around time of the BNP test is too long to be clinically useful for the immediate bedside management of SCAPE.
SCAPE is a bedside clinical diagnosis which must be reached within minutes (on the basis of history, examination, and POCUS).
Again, I remind myself and my readers that the above excerpts are incomplete and to be sure and review the complete chapter on the IBCC site.