Today, I review, embed, and excerpt from Dr. Amal Mattu’s YouTube video, Cardiogenic Syncope – For the Faint of Heart | The Heart Course from The Center for Medical Education.
All that follows is from the above resource.
Cardiogenic Syncope – For the Faint of Heart by Amal Mattu, MD
Dr. Mattu reminds us that every patient with syncope requires a carefully interpreted 12-lead eckg.
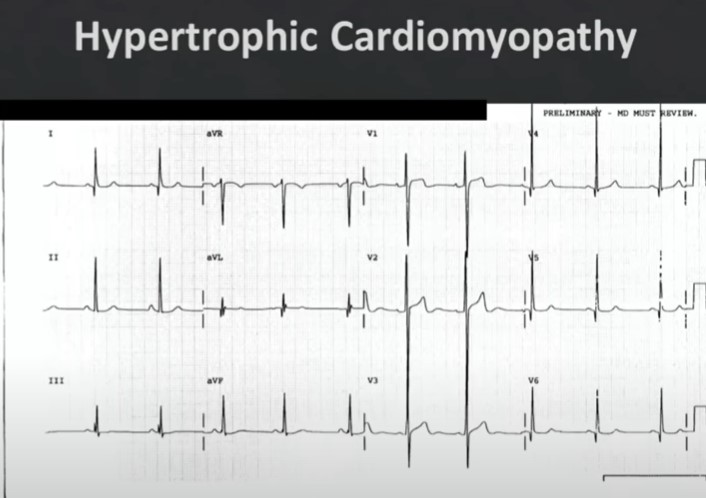
2:03
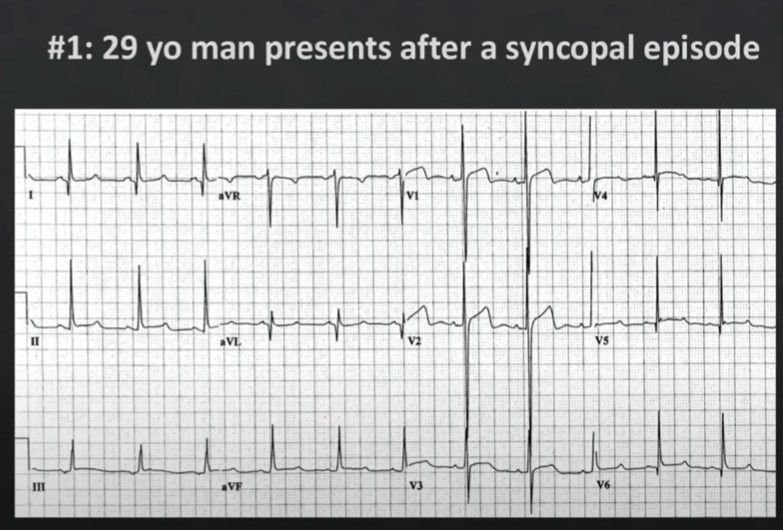
2:42
The patient was discharged to home after the above ecg.
The patient had a cardiac arrest at home and could not be resuscitated.
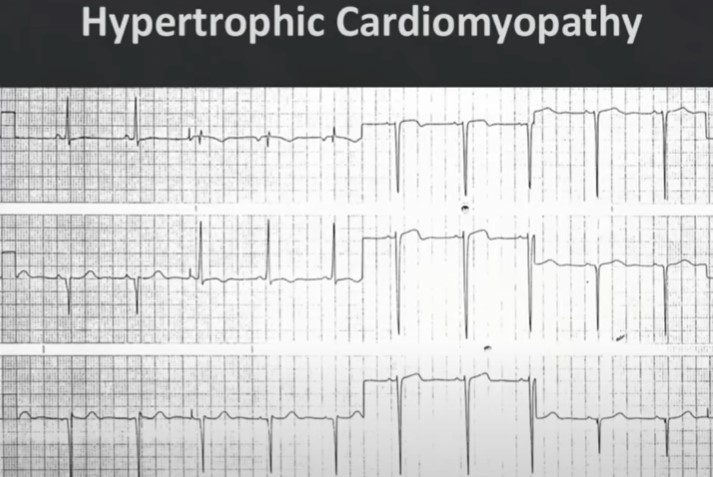
4:07 The above ecg showed:
4:00 – 5:55 Discussion
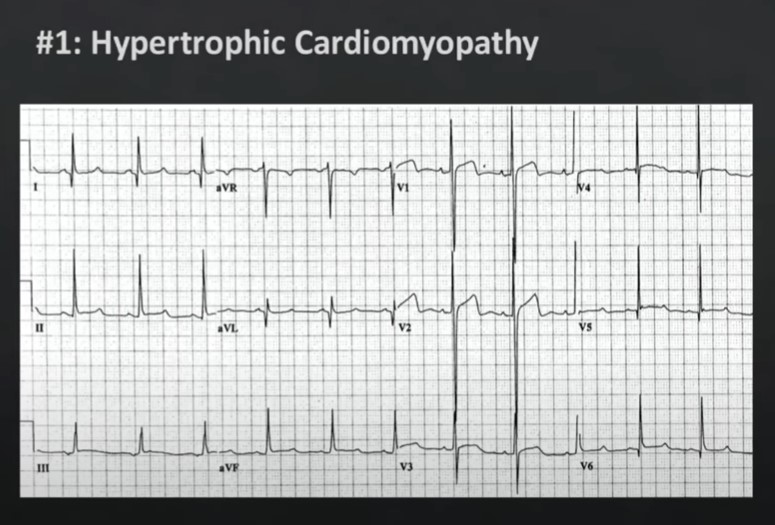
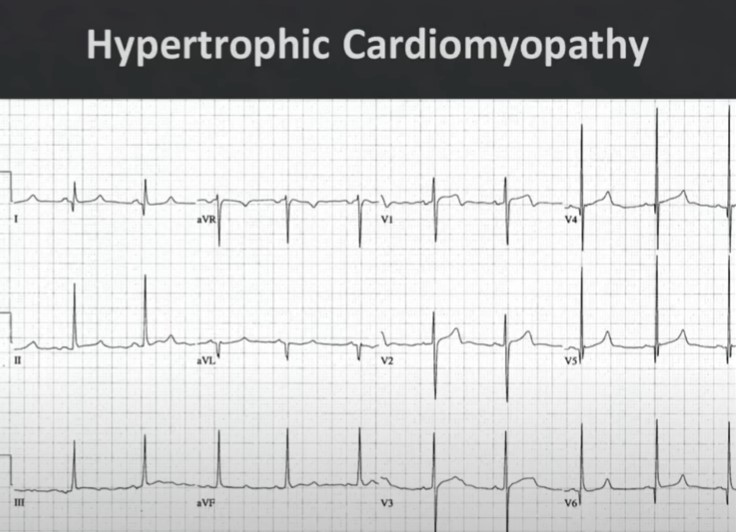
The diagnosis here is hypertrophic cardiomyopathy. Now one of the problems here with hypertrophic cardiomyopathy is most people don’t learn how to diagnose hypertrophic cardiomyopathy on the 12 lead.Even the cardiologists don’t typically learn this unless you’re talking about maybe a cardiologist who teaches the courses or writes the books on ekgs and the reason is most cardiologists learn to diagnose this on echo exactly on doppler echo they don’t learn the ekg findings.But you and I as emergency physicians, we’ve got to know the ekg findings.So what is it that you’re looking for? Discussion Continues
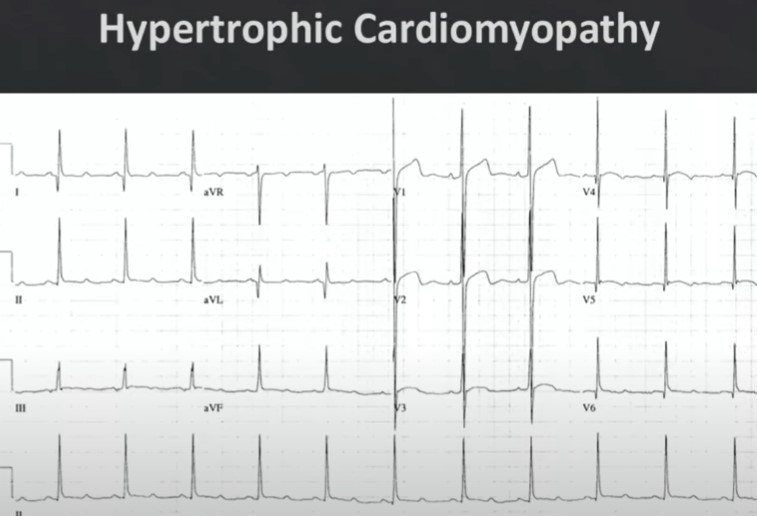
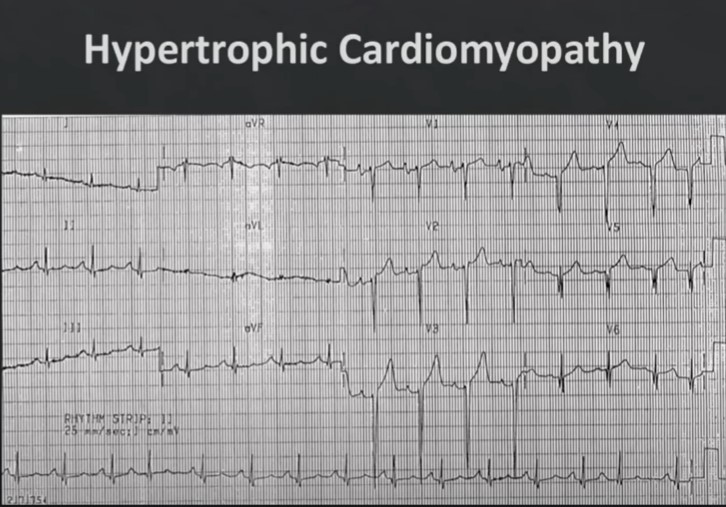
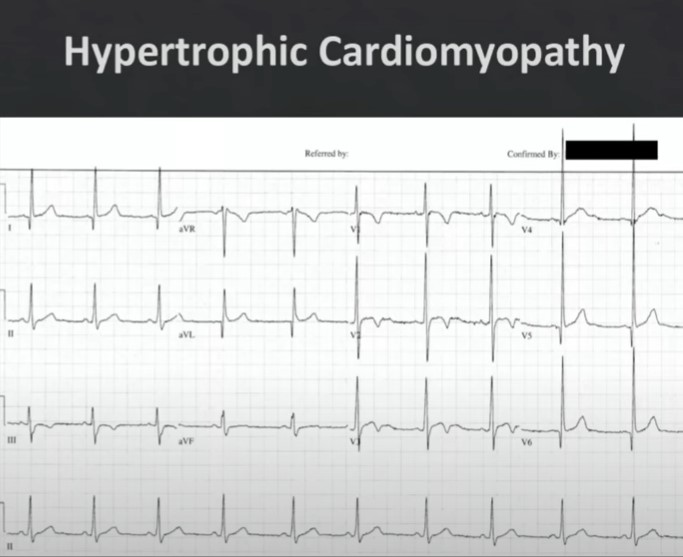
5:55 – 8:50 For the rest of the discussion on hypertrophic cardiomyopathy.
5:55 Another example of ECG of Hypertrophic Cardiomyopathy
6:11 Another example of ECG of Hypertrophic Cardiomyopathy
6:24 Another example of ECG of Hypertrophic Cardiomyopathy: Abnormal T waves
6:55 Another example of ECG of Hypertrophic Cardiomyopathy
7:07 Another example of ECG of Hypertrophic Cardiomyopathy7:39 Another example of ECG of Hypertrophic Cardiomyopathy8:19
Dr. Mattu summarizes what we have learned and what we need to do:
cardiomyopathy you get that patient off to a cardiologist as quickly as possible in the meantime you tell them no
exertion and if there’s any delay you put them on some beta blockers beta blockers or
negative ionotropes no exertion and negative ion tropes beta blockers until they see the cardiologist and get a
doppler echo and you know what you just save a young kid’s life by knowing what to look for so again hypertrophic
cardiomyopathy look for high voltage and deep narrow cues especially lateral leads the vast majority of these are
males but we have seen some cases in women young women as well and your diagnostic test of choice is getting the
doppler echo all right so we’ll let that sink in just take a little mental break for a second so let’s recap what is it
that you’re looking for on the 12 lead of a syncope patient you’re looking for signs of ischemia you’re looking for
dysrhythmias in av blocks we’ve added hypertrophic cardiomyopathy to the list of things that you always look for.
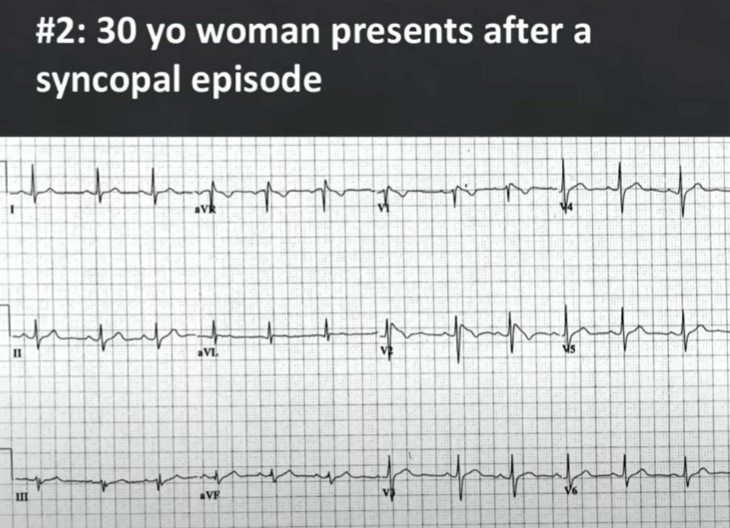
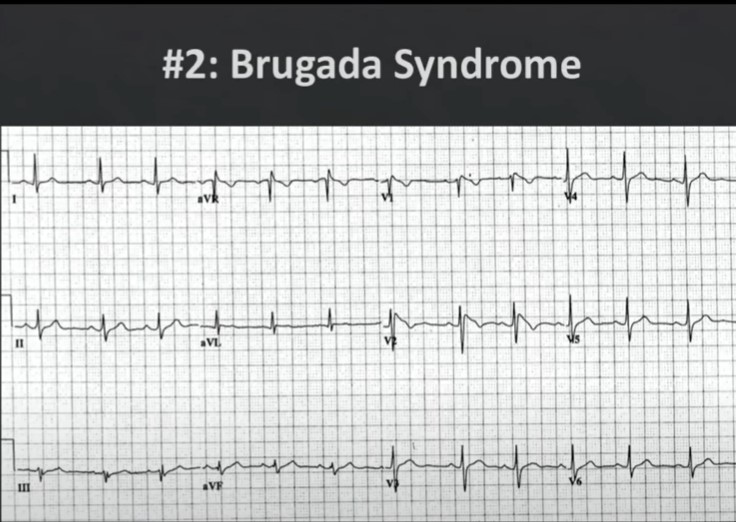
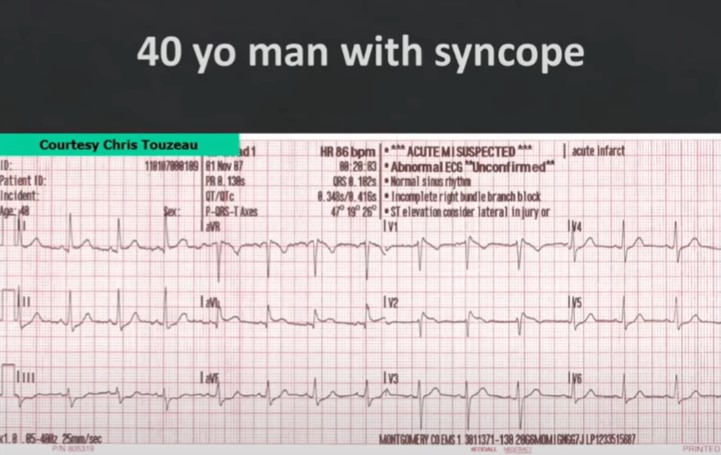
8:53 Case 2
9:52
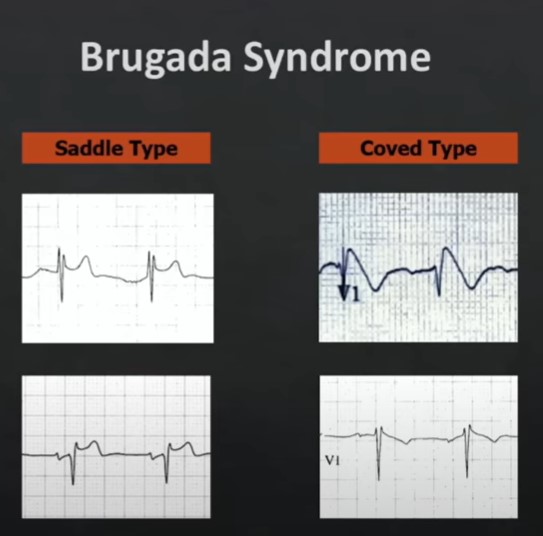
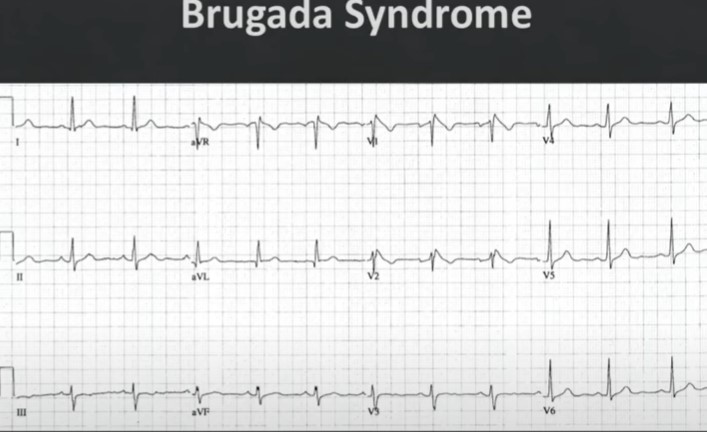
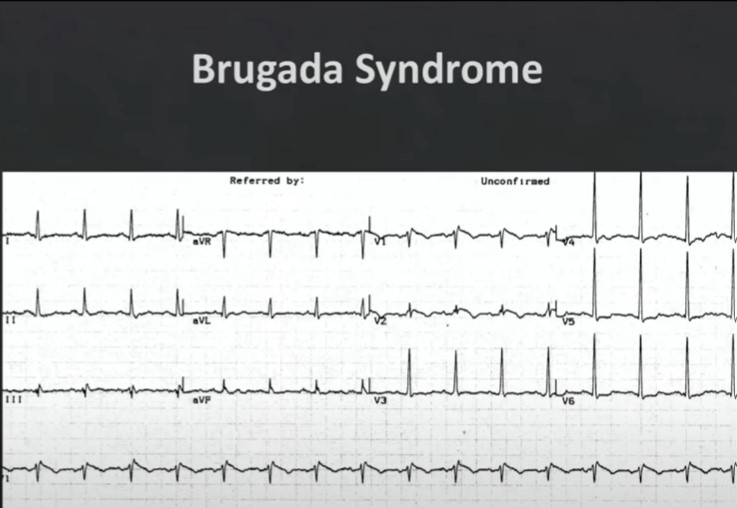
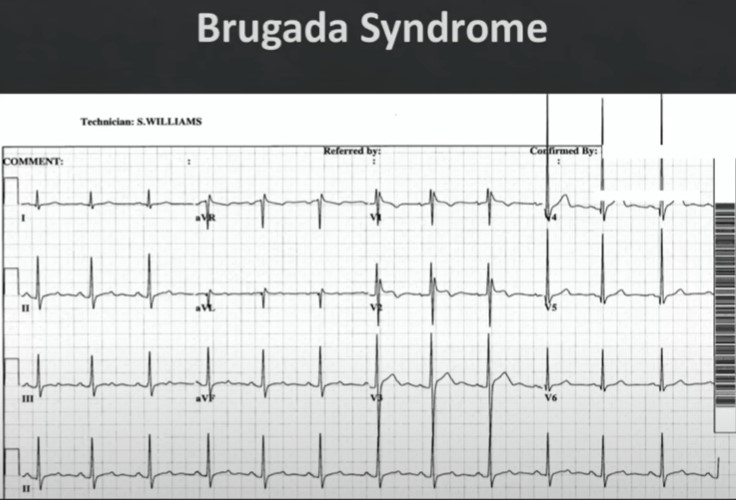
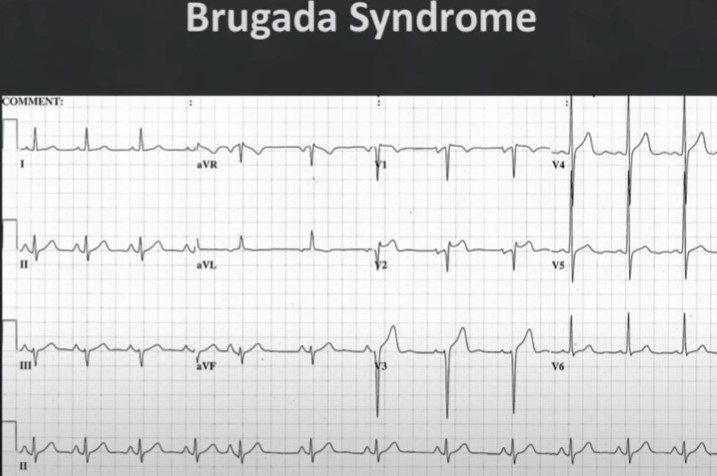
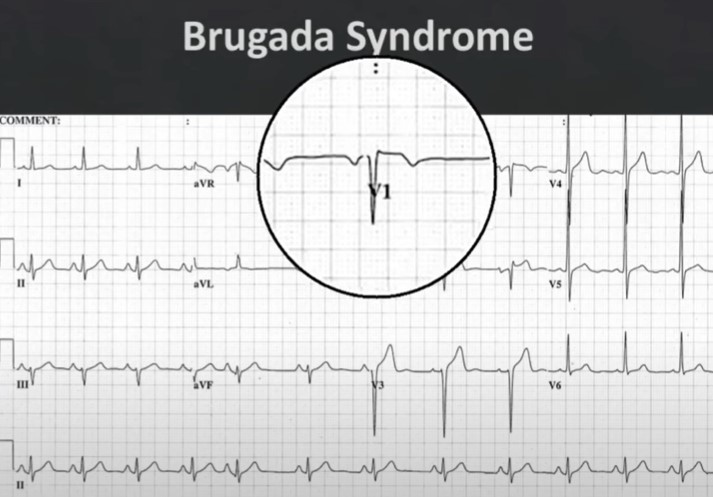
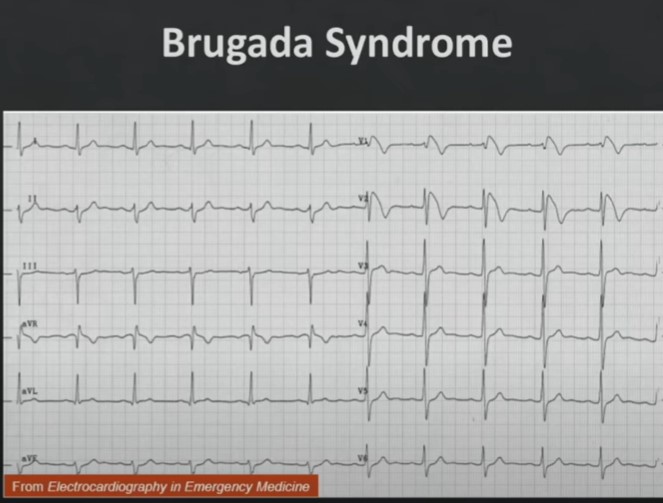
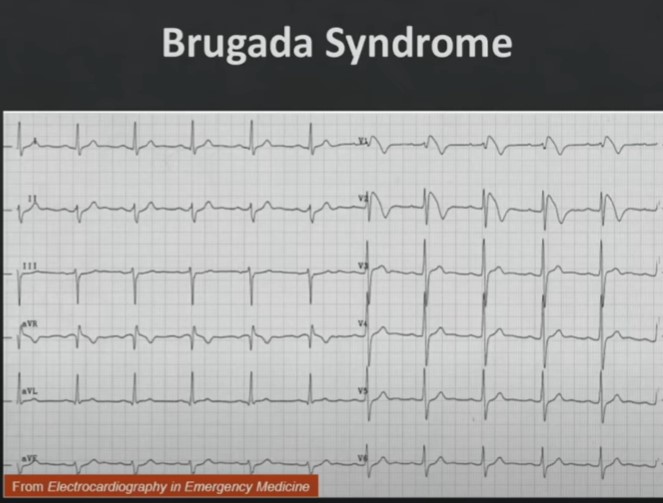
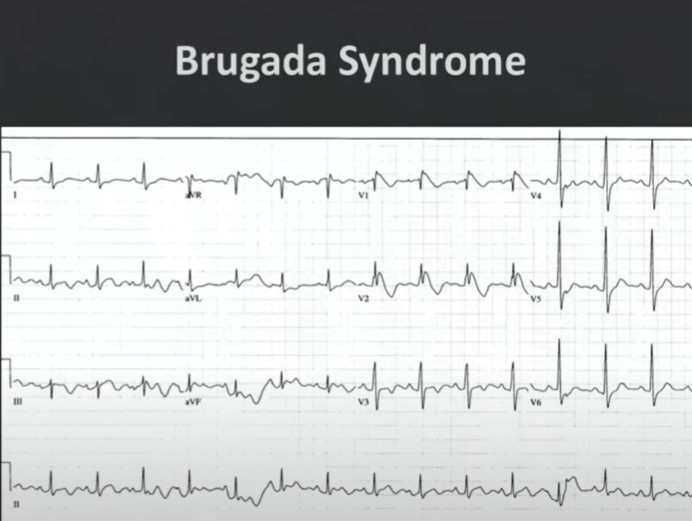
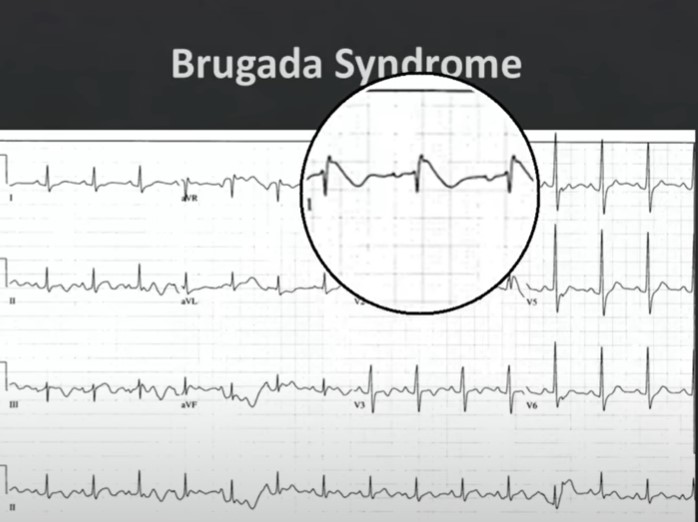
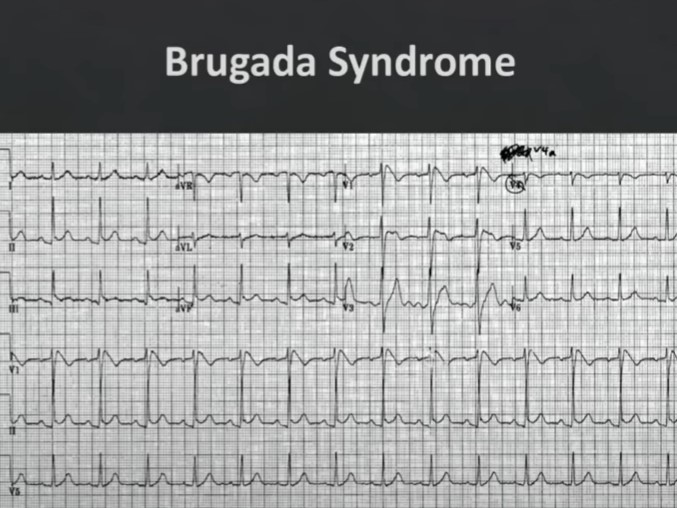
11:4012:40 Another Example15:40 Another Case16:55 Another Example. And this is a bit more subtle.17:12 Same ECG as 16:55 above. You see that incomplete right bundle pattern with a little bit of elevation of the ST elevation terminating in T wave inversion. This is not normal for a right bundle branch block.
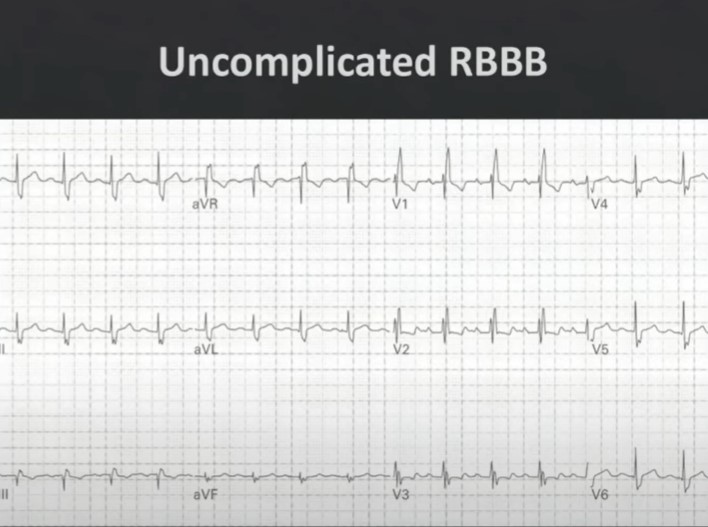
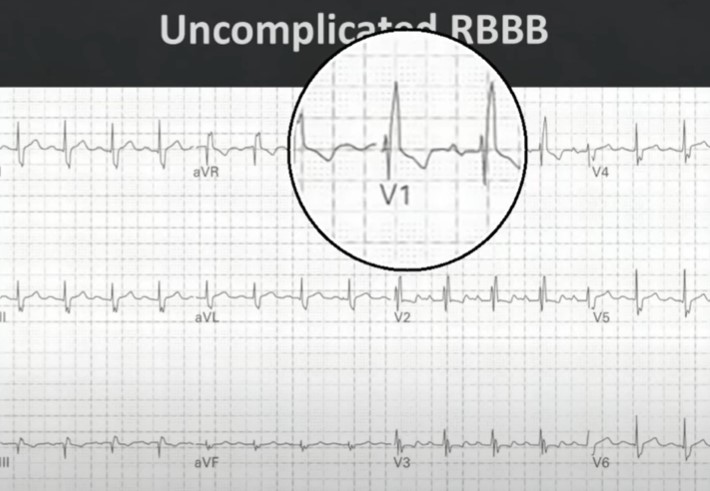
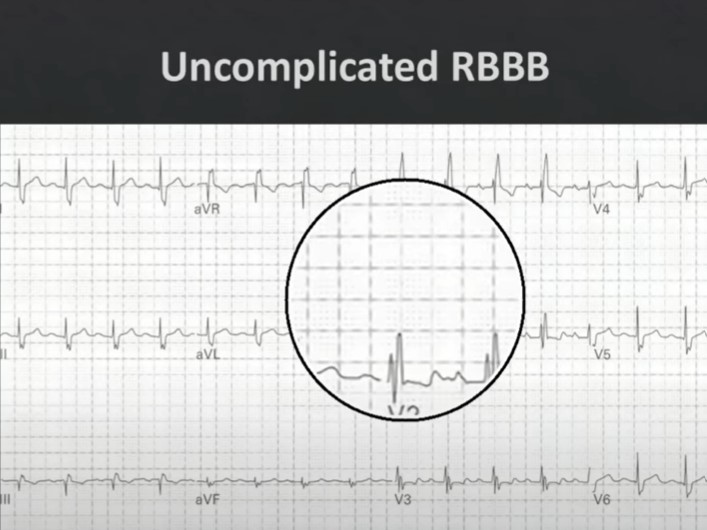
17:16 For comparison, this is what a normal right bundle branch block looks like. Normally with a RBBB or an incomplete RBBB you’ll have a little bit of ST depression in V1 and V2. So if you ever see a RBBB or incomplete RBBB in V1 and V2 with ST elevation, especially with syncope or near syncope, think of Brugada syndrome and get prompt referral to electrophysiologist for definitive diagnosis.17:23 Same ECG as 17:16 . . . with ST depression in V1 and V2. So if you ever see a RBBB or incomplete RBBB in V1 and V2 with ST elevation, especially with syncope or near syncope, think of Brugada syndrome and get prompt referral to electrophysiologist for definitive diagnosis.
17:24 Same ECG as 17:16 and 17:23
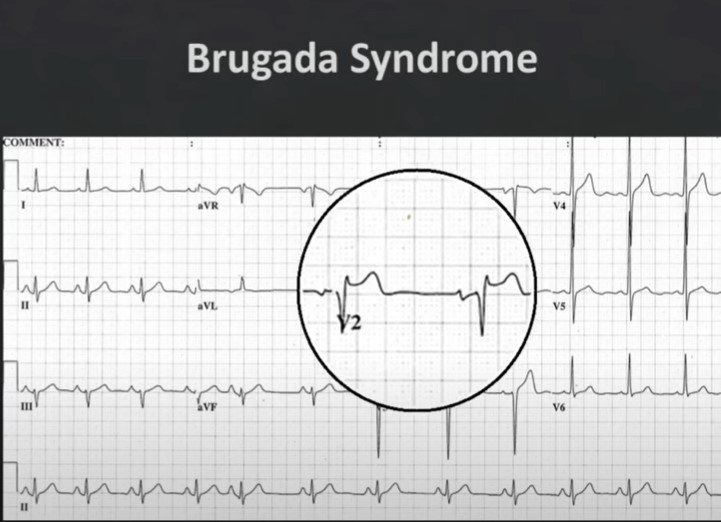
17:50 This one is more subtle. There is an incomplete right bundle with ST elevation and T wave inversion.17:51: Same ECG as 17:50: There is an incomplete Right Bundle with ST elevation terminating in an inverted T-wave.
17:56: Same ECG as 17:50 and 17:51: There is that saddle morphology in V2. And this turned out to be positive for Brugada Syndrome.
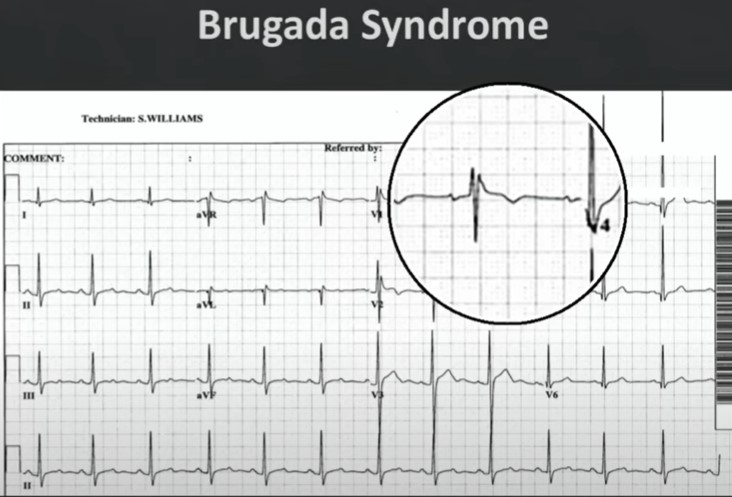
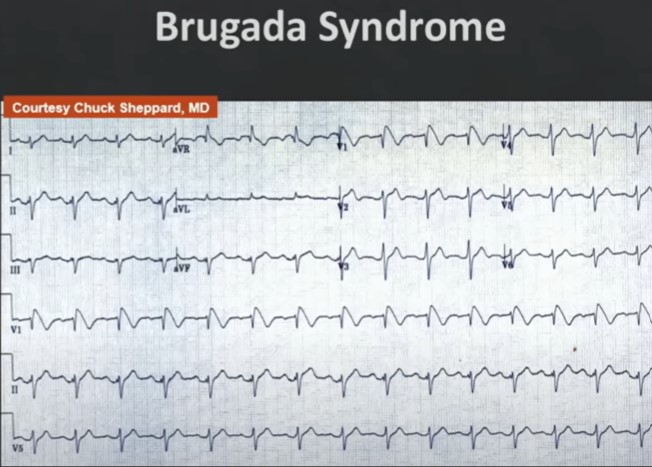
18:04: Here is another Brugada limited to V1. But this is a very classic morphology in V1. This is a young person who was having intermittent near-syncopal episodes. And Dr. Sheffield made the diagnosis.18:13: Here is another Brugada with very classic incomplete RBBB in V1 and V2 with that convex upward ST-elevation. Send that patient to an electrophysiologist and you are going to save a life.18:14: Classic Brugada. Incomplete Right Bundle with the convex upward ST-elevation. Send that patient to an electrophysiologist and you’ll save a life.
18:24: This patient was diagnosed at a community hospital18:31: Same ECG as 18:24. V1 is very classic for Brugada Syndrome. Transferred to tertiary center where an electrophysiologist confirmed diagnosis and inserted an ICD.The next day, the ECG was over-read by a general cardiologist as ST elevation possible MI. The general cardiologist did not know about Brugada Syndrome. So if you have an option refer to an electrophysiologist.19:30: Another very classic example in V1.20:37: It is estimated that Brugada Syndrome may be responsible for 4 to 5% of all medical cardiac arrests.21:08: The computer will often miss Brugada Syndrome as below: