In addition to the resource below please review
- A Novel Method for Estimating Right Atrial Pressure With Point-of-Care Ultrasound [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Larry Istrail 1, Joseph Kiernan 2, Maria Stepanova 3. J Am Soc Echocardiogr. 2023 Mar;36(3):278-283. doi: 10.1016/j.echo.2022.12.008. Epub 2022 Dec 13.
- Here is the link to the YouTube video, Jugular Venous Pressure (JVP) Exam using Point-of-care Ultrasound (POCUS), by the author of the above article. POCUS Med Ed. “Jan 1, 2023. With Point-of-care ultrasound (POCUS), you can measure the JVP accurately in every patient regardless of their BMI using this method. This has been validated against right heart cath right atrial pressure measurements and is within 3 mmHg in most patients.
- Validation study: https://bit.ly/3YXlH6F
- The Pocus Manifesto: https://amzn.to/3EZoEu5
- For more on POCUS see https://www.pocusmeded.com/
- For a summary of the above article please see Links To And Excerpts From “A Novel Method for Estimating Right Atrial Pressure With Point-of-Care Ultrasound”
Posted on December 16, 2023 by Tom Wade MD - The above article has been cited by
-
World J Cardiol. 2024 Feb 26;16(2):73-79. doi: 10.4330/wjc.v16.i2.73.PMID: 38456073 Free PMC article. Review.
-
Int J Cardiovasc Imaging. 2023 Dec;39(12):2437-2450. doi: 10.1007/s10554-023-02941-8. Epub 2023 Sep 8.PMID: 37682418 Free PMC article.
-
- There are 103 similar articles in PubMed.
- Here is the link to the YouTube video, Jugular Venous Pressure (JVP) Exam using Point-of-care Ultrasound (POCUS), by the author of the above article. POCUS Med Ed. “Jan 1, 2023. With Point-of-care ultrasound (POCUS), you can measure the JVP accurately in every patient regardless of their BMI using this method. This has been validated against right heart cath right atrial pressure measurements and is within 3 mmHg in most patients.
Today, I review and excerpt from the Entrance Section of
- The “5Es” of emergency physician-performed focused cardiac ultrasound: a protocol for rapid identification of effusion, ejection, equality, exit, and entrance [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Acad Emerg Med. 2015 May;22(5):583-93. doi: 10.1111/acem.12652. Epub 2015 Apr 22.
All that follows is from the above resource.
Entrance
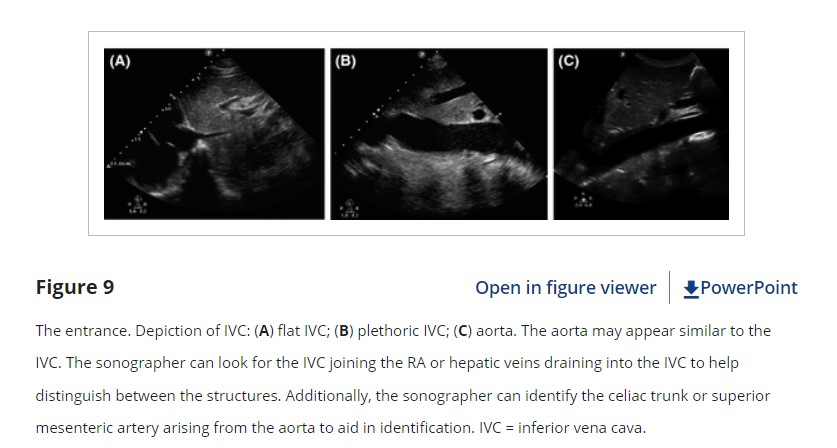
The fifth and final “E” in our protocol is for entrance to the heart or assessment of the IVC. The usefulness and reliability of IVC assessment and its correlation to central venous pressure, fluid status, and fluid responsiveness has been studied extensively over the past several years. While controversy exists over the correlation of IVC measurements to other quantitative measures of RA pressure, the qualitative assessment of the IVC may be clinically helpful, particularly if it is plethoric or noncollapsible or notably flat.52 IVC plethora is highly sensitive for tamponade as well as congestive heart failure.22, 53 By contrast, a flat or highly collapsible IVC correlates well with acute blood loss and hypovolemia (Figure 9).54, 55 While the majority of cardiac views should be performed first to provide context for IVC findings, early assessment of the IVC can help to quickly differentiate causes of shock, chest pain, and dyspnea.3
Techniques for Assessing Entrance
While the first 4Es can often be obtained from a parasternal view, assessment of the IVC requires a subcostal or subxiphoid approach. The SXLA provides a longitudinal view of the IVC and has been shown to have the best inter-rater reliability.56 The SX4C can also show the IVC in short axis, although craniocaudal movement of the IVC during respiration should be considered.57
The IVC should be assessed in terms of overall size and collapsibility. Both size and collapsibility can also be measured quantitatively, although the significance of exact numbers is questionable. IVC diameter is typically measured at its largest diameter (end expiration) at about 2 cm distal to the junction of the IVC and RA or 1 cm distal to the where the hepatic veins join the IVC. An IVC diameter of ≥2 cm, especially with minimal or no collapsibility, is considered plethoric and correlates with increased RA pressure. An IVC of <1 cm, particularly with complete collapse, is considered flat and indicates low preload and potential fluid responsiveness.58, 59 An IVC diameter between 1 and 2 cm is typically normal, but estimation of preload can be improved by including the degree of collapsibility, also known as the “caval index,” which ranges from 0 to 1. The percent collapsibility (caval index × 100) is calculated as the difference between the inspiratory and expiratory diameters divided by the inspiratory diameter. A high caval index (high percent collapse) indicates lower preload.
Pearls and Pitfalls of Entrance
When in a long-axis plane, inadvertently sliding off the center of the vessel produces a cylinder tangent effect, which may underestimate the size of the IVC and overestimate its collapse. Obtaining short-axis and long-axis views of the IVC may help avoid this. The IVC also moves both anterolaterally and craniocaudally with inspiration, and this translocation should be taken into account during visualization or measurements.57
Another pitfall is mistaking the descending aorta for the IVC when scanning in a long-axis plane. The IVC may appear to pulsate or vary with respiration; the aorta has a thicker wall and is positioned to the patient’s left. In a transverse or axial plane, the IVC should be seen on the left of the screen, to the patient’s right. Following the IVC proximally through the liver parenchyma should reveal the hepatic veins joining the IVC before it enters the RA, while the aorta will travel behind the heart. Therefore, an IVC in long axis will “curve up” on the left side of the screen making a “happy whale sign” whereas the aorta in long axis will “curve down” on the left side of the screen as seen in Figure 9.
The diameter of the IVC should be used in conjunction with the collapsibility to improve accuracy of preload estimation. For example, an IVC of 1.5 cm with a high caval index may be considered indicative of lower preload, while an IVC of 1.8 cm with a low caval index may indicate higher preload. In these latter situations, repeating IVC assessment after an intervention such as fluid administration may provide more valuable information.
Conclusions
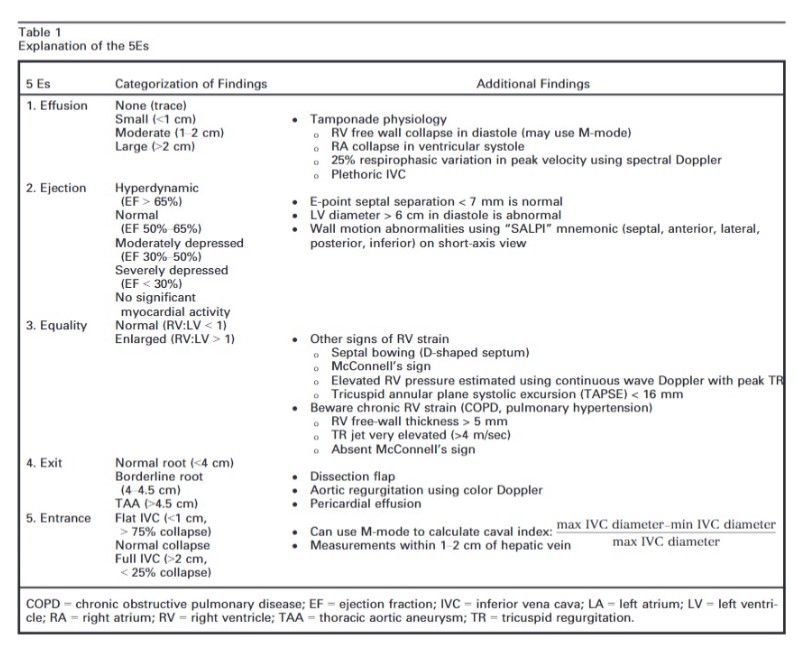
The intent of this article is to codify elements of the cardiac US exam that we have found to be most relevant to patients presenting with acute or emergent complaints (Table 1). A recent international consensus statement defined FOCUS as being goal-directed, problem-oriented, limited in scope, simplified, time-sensitive and repeatable, qualitative and semiquantitative, performed at the point of care, and usually performed by clinicians.6 The 5Es described in this article meet all of these criteria. However, the international statement addressed the use of FOCUS in “all clinical settings” and included the assessment of chronic cardiac disease, as well as gross valvular abnormalities and large intracardiac masses, without assessment of the thoracic aorta.
In our experience the 5Es encompass the cardiac US findings most applicable in patients who present emergently with hypotension, dyspnea, syncope, penetrating thoracic trauma, chest pain, or other acute complaints where diagnosis may be aided by visualization of the heart. While gross valvular abnormalities and intracardiac masses are important if they are seen, they are less common and less acute and tend to be less immediately deadly than acute thoracic aortic disease, which accounts for more than twice as many deaths as abdominal aortic aneurysm rupture.51The 5Es are not meant to provide an absolute boundary for EP FOCUS, which will likely continue to evolve, but are intended to provide a framework for the acquisition and interpretation of the most relevant and applicable components of echocardiography in the emergent setting. We hope that adoption and subsequent application of the 5Es in EDs will help to standardize and effectively teach the echo findings that may allow EPs to save lives and expedite the care of patients with potentially life-threatening illness. We thank Jane Hall, PhD, for preparing Figures 4, 6, and 8. We also thank Daniel Wadsworth Groves, MD, for manuscript review. Supporting Information
Filename Description acem12652-sup-0001-VideoClipS1.mp4MPEG-4 video, 9.8 MB Video Clip S1. First E: effusion. acem12652-sup-0002-VideoClipS2.mp4MPEG-4 video, 5.1 MB Video Clip S2. Second E: ejection fraction. acem12652-sup-0003-VideoClipS3.mp4MPEG-4 video, 8.7 MB Video Clip S3. Third E: equality. acem12652-sup-0004-VideoClipS4.mp4MPEG-4 video, 3.6 MB Video Clip S4. Fourth E: exit. acem12652-sup-0005-VideoClipS5.mp4MPEG-4 video, 2.1 MB Video Clip S5. Fifth E: entrance. Please note: The publisher is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing content) should be directed to the corresponding author for the article.