The place to get started for learning about Food Allergy, Food Intolerance, and Celiac Disease is the outstanding podcast and show notes, #95: Food allergy, food intolerance and celiac disease MAY 14, 2018 By MATTHEW WATTO, MD from The Curbsiders
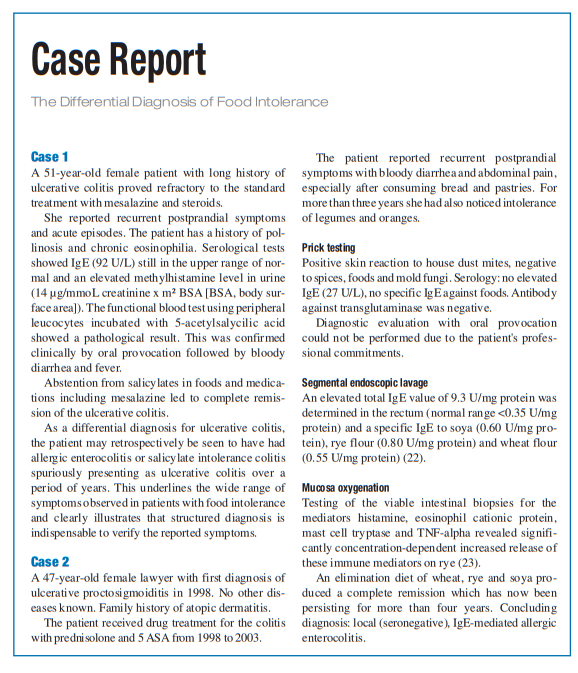
This post consists of excerpts from Resource (1) below, The differential diagnosis of food intolerance [PubMed Abstract] [Full Text HTML] [Full Text PDF]:
Summary
More than 20% of the population in industrialized countries suffer from food intolerance or food allergy.
The majority of cases of food intolerance (15% to 20%) are due to non-immunological causes. These causes range from pseudoallergic reactions to enzymopathies, chronic infections, and psychosomatic reactions that are associated with food intolerance. The prevalence of true food allergy, i.e., immunologically mediated intolerance reactions, is only 2% to 5%.
The differential diagnosis of food intolerance is broad. Therefore, a structured diagnostic algorithm with input from multiple clinical disciplines should be applied. The treatment consists of eliminating the offending substance from the diet as well as medications and psychosomatic support, when indicated.
Differential diagnosis: non-immunologically
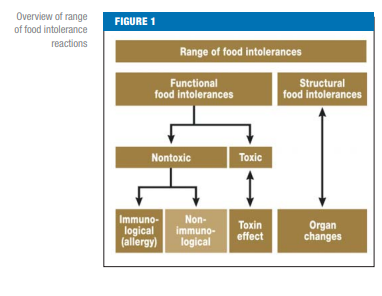
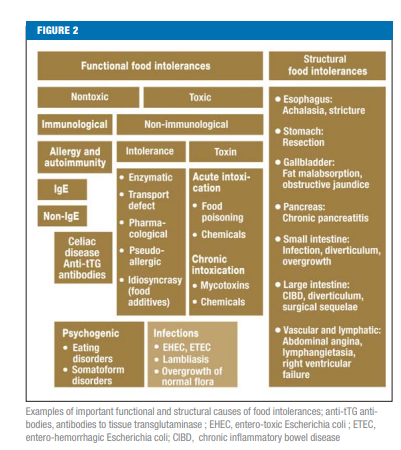
mediated food intolerancesSince the population prevalence of functional and structural,
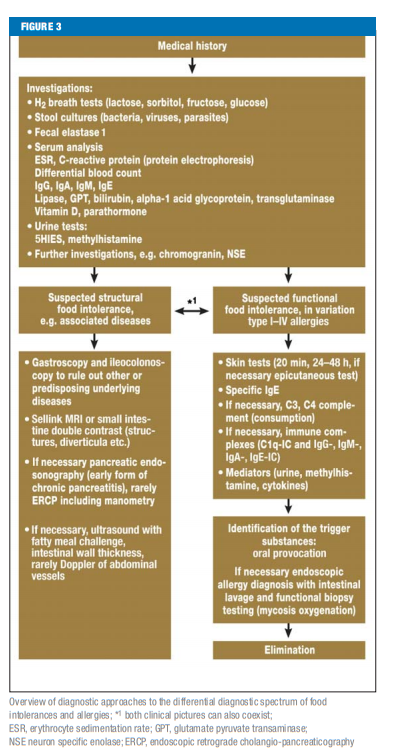
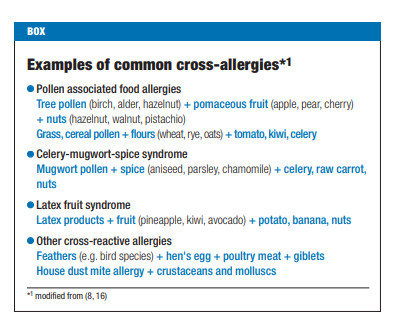
non-toxic and non-immunologically mediated clinical presentations (Figures 1 and 2 [above]) are much commoner (15% to 20%) than the immunologically mediated true allergies (2% to 5%) or toxic disease mechanisms, diagnostic evaluation should initially consider the nonimmunologically mediated differential diagnoses when it is uncertain what is causing the patient’s symptoms (e.g. carbohydrate malabsorption, neurodermatitis, pancreatic insufficiency, mastocytosis, [Figure 3]). This should always be performed before embarking upon detailed immunological investigation aimed at detecting the presence of a systemic or local food allergy. This also appears relevant in view of the frequent association of carbohydrate malabsorption, histamine intolerance, or infections with atopic diseases or food allergy.The full gamut of diagnostic modalities outlined in Figure 3 will not be required for every patient but should be applied on a
case by case basis with reference to the history, clinical findings, and possible differential diagnoses, as well as previous findings, in a cost conscious manner (4, 8, 11).Carbohydrate malabsorption
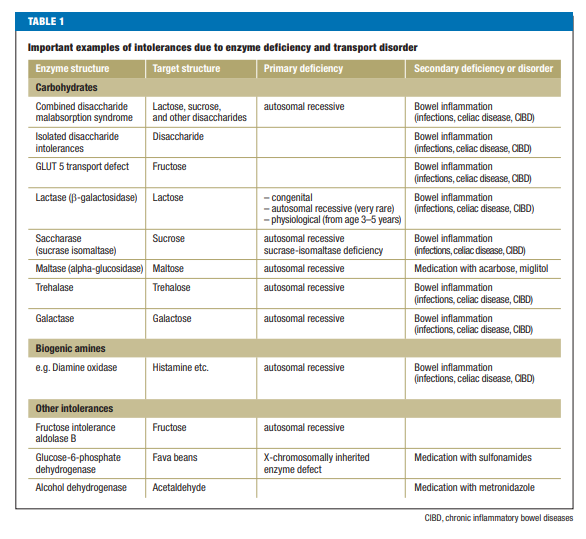
Carbohydrate absorption is significantly affected by disorders
such as lactase deficiency (intolerance of milk sugar) and diseases affecting the transport of certain mono- and disaccharides. Impairments of the digestion and absorption of simple carbohydrates are the commonest non-immunological food intolerances in the European population (lactose, fructose, sorbitol malabsorption etc. [Table 1]).Small bowel bacterial overgrowth
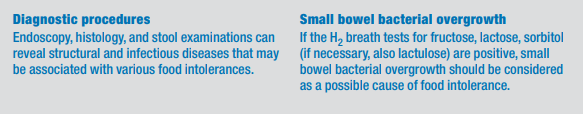
If the H2 breath tests for fructose, lactose and sorbitol
(and possible lactulose) are positive, bacterial overgrowth
of the small intestine should be considered as a
possible cause of the food intolerance. As with carbohydrate
malabsorption, this condition often leads to
meteorism, flatulence, diarrhea, and pain in a nonspecific
pattern involving a variety of foods. Patients
with postoperative changes, peristaltic disorders, diabetes
mellitus, and patients who are medicated with
immunosuppressives or proton pump inhibitors are
especially affected. An H2 breath test for glucose should
be performed to rule out small bowel bacterial overgrowth.Histamine Intolerance
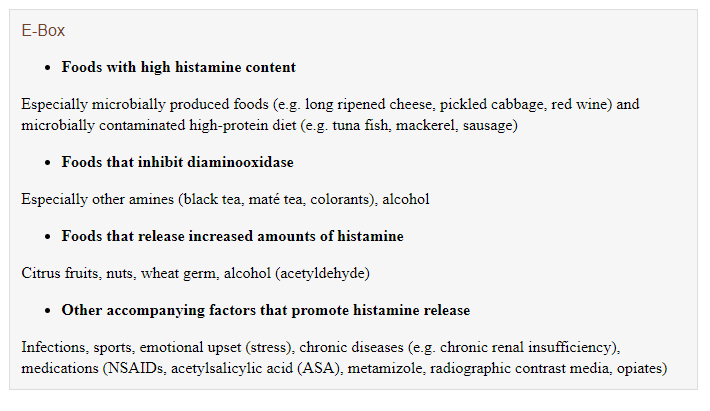
Histamine intolerance is caused by a disorder of the
metabolism of mainly exogenously supplied histamine
(histamine-rich foods and semiluxuries). This is most
commonly attributed to a deficiency of the enzyme
diaminoxidase (DAO) which is responsible for the
extracellular biotransformation of histamine (12, 13).
But histamine-N-methyltransferase (HNMT) responsible
for intracellular histamine breakdown may also be
involved. About 1% of the total German population of
82 Mill. is affected by histamine intolerance, 80% being
middle-aged women (13).A slight increase in histamine concentration above the normal range already causes incipient vasodilatation, increased secretion of gastric fluid and mucus, and contraction of the smooth muscles. A further increase leads to tachycardia, arrhythmias, and typical cutaneous reactions. There may also be hypotension, bronchospasm and, with a rapid rise in histamine concentration, shock or cardiac arrest (12, 13). The gastric acid secretion and smooth muscle contraction which already starts when there are slight increases in histamine levels explains why many people with food intolerances and allergies in whatever form have unspecific abdominal symptoms such as dyspepsia, a sensation of bloating and tension or pain. Typical trigger factors of histamine intolerance are listed in the e-Box (12, 14).
Salicylate Intolerance
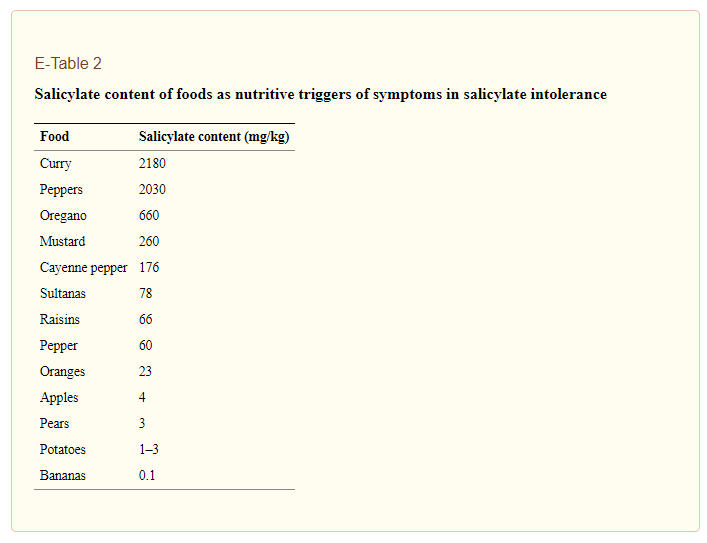
The prevalence of salicylate intolerance in Europe is 2.5% (8). The classical symptoms of salicylate intolerance are respiratory complaints (blocked or runny nose, sinusitis, nasal polyposis, bronchial asthma), but can also lead to gastrointestinal complaints with meteorism, flatulence, diarrhea and, rarely, to colitis with strictures and ulcers (5, 14). The pathogenesis of salicylate intolerance is based on an inhibition of cyclooxygenase-1 by salicylates and other non-steroidal pain medications, but also by salicylate-containing foods and other acids (such as benzoic acid or colorants) resulting in reduced prostaglandin synthesis (5).
In intolerant individuals this leads to activation of the leukotriene metabolism with increased formation of LTB4 and/or LTC4-E4.
This condition is detected by a blood cell test (heparinized blood) with incubation of 5-acetylsalicylic acid and arachidonic acid or by provocation tests (nasal, bronchial, oral [5]).
The recommended treatment is abstinence from the inducing substances; the most important foods concerned are listed in e-Table 2.
In intolerant individuals this leads to activation of the leukotriene metabolism with increased formation of LTB4 and/or LTC4-E4.
This condition is detected by a blood cell test (heparinized blood) with incubation of 5-acetylsalicylic acid and arachidonic acid or by provocation tests (nasal, bronchial, oral [5]).
The recommended treatment is abstinence from the inducing substances; the most important foods concerned are listed in e-Table 2.
If dietary therapy alone is insufficient, treatment with leukotriene receptor blockers or deactivation with acetylsalicylic acid should be attempted (5) (see supplementary case report).
Differential diagnosis of immunologically
mediated food intolerance: food allergyAmong the food intolerances and immunologically
mediated diseases, food allergy exhibits the greatest
complexity. This is due to the heterogeneous pattern of
clinical symptoms associated with food allergies
(including intra-individually). Diagnostic assessment
should also include the much more common nonimmunological
intolerances and diseases of other etiology.
Since it is rarely clear at the patient’s first visit to a
medical practice whether a food intolerance is of nonimmunological
or immunological etiology or is due to a
combination of the two mechanisms, diagnosis of food
allergy should focus not only on identifying a specific
trigger factor but should also include a detailed evaluation
of the possible differential diagnoses and therefore
attempt to distinguish the patient’s condition from other
chronic diseases.Stepwise diagnostic procedure for food allergies
Specific allergological routine diagnosis begins with
taking a dietary history, completing a nutrition diary,
performing skin tests (e.g. prick test) for food extracts,
environmental antigens, mould fungi, spices etc., assay
of total IgE and the suspected allergen specific IgE antibodies
in serum, in order to detect evidence of IgE specific
sensitization (4, 8–11, 20). If clinically unequivocal
postprandial reactions are observed which are consistent
with the results of skin tests and antigen specific IgE
sensitization, this diagnostic approach can in many
cases already exactly define and identify the IgE-mediated
allergic disease (1, 4, 8, 10, 20). With the typical combination
of intestinal and extraintestinal symptoms immediately
after allergen ingestion with monovalent or oligovalent
sensitization, oral provocation testing in atopy
(IgE-mediated allergy) is confirmatory in nature but is
still regarded as the diagnostic gold standard (9–11, 16).
If the elimination diet is unequivocally successful with
this constellation, oral provocation as a confirmatory
reaction is unnecessary from the clinical perspective.[The section on Stepwise Diagnosis has detailed notes on evaluation for allergic diseases. See pp 365 -367 of the PDF. In view of it’s complexity, consider referral to an allergist.]
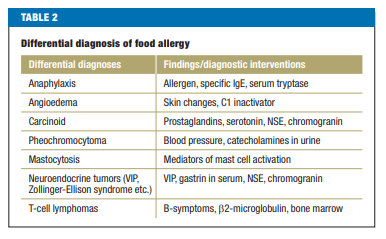
Differential diagnosis of diseases associated with food intolerances
If non-specific evidence of food reactions is found,
other conditions which may present with symptoms
similar to those seen in intolerances or allergies should
be ruled out, such as chronic inflammatory bowel diseases,
chronic pancreatitis, irritable bowel syndrome,
eosinophilic gastroenteritis, systemic mastocytosis,
celiac disease, and microscopic colitis[For a discussion of the above illnesses see pp. 366 + 367 of the PDF]
Additional Resources:
(1) The differential diagnosis of food intolerance [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Dtsch Arztebl Int. 2009 May;106(21):359-69; quiz 369-70; 4 p following 370. doi: 10.3238/arztebl.2009.0359. Epub 2009 May 22.