Resource (2) has links to recommended growth charts needed to assess growth and to diagnose failure to thrive from the Centers For Disease Control.
The following are excerpts of Resource (1) from the American Family Physician:
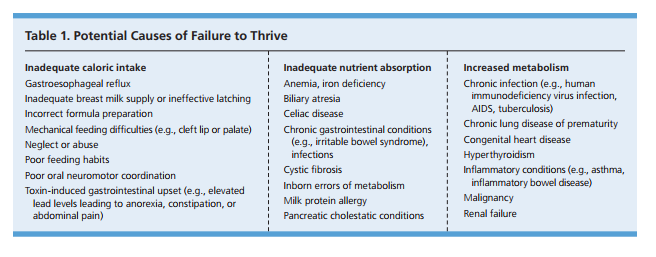
Failure to thrive (FTT) is an abnormal pattern of weight gain defined by the lack of sufficient usable nutrition and documented by inadequate weight gain over time. The decrease in the velocity of weight gain results in the child steadily falling off the expected weight curve on growth charts.1-3
Although there is no consensus on the definition of childhood FTT, the term is often used for infants and children with weight below the 5th percentile for sex and corrected age.15 Supporting definitions include weight for length below the 5th percentile; body mass index for age below the 5th percentile3; or a
sustained decrease in growth velocity, in which weight for age or weight for length/height falls by two major percentiles (percentile markers 95, 90, 75, 50, 25, 10, and 5) over time.15
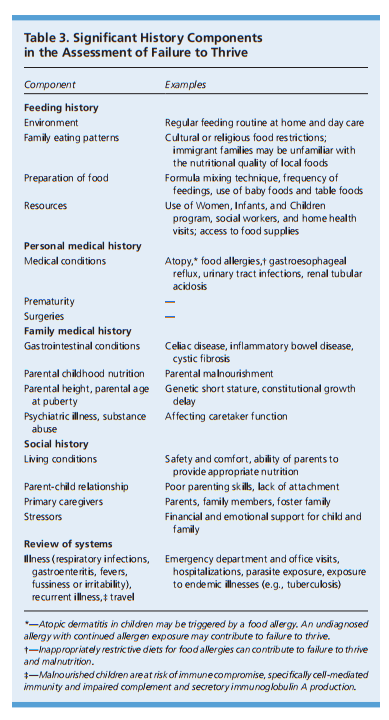
The key elements of the history include a nutritional evaluation and medical, family, and social histories (Table 3).
And a food diary can be very helpful in the evaluation.
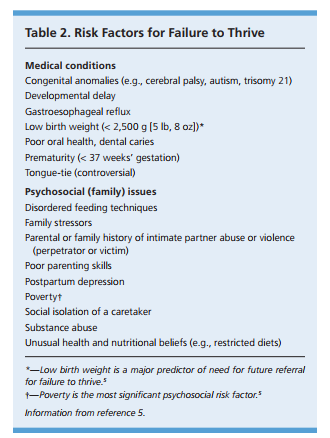
A brief developmental evaluation using any standard validated questionnaire helps to identify patients with potential developmental abnormalities contributing to FTT. Abnormal development may be an early indicator of an underlying medical condition, such as a neuromuscular disorder or a psychosocial problem, such as neglect, that can contribute to or exacerbate FTT. Also, children with FTT have a higher incidence of developmental delay.20[Emphasis Added] The assessment provides a baseline for ongoing monitoring of development that may be impacted by severe nutritional compromise. One example of a free tool for monitoring development is the Rourke Baby Record from Canada.
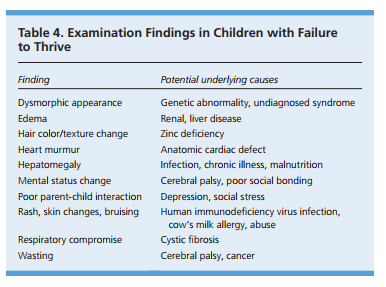
PHYSICAL EXAMINATION
The goals of the physical examination are identification of any chronic or acute illness, recognition of dysmorphology suggesting a genetic condition, assessment for normal development, and quantification of the degree of undernutrition. Table 4 includes key physical examination findings in children with FTT. Underlying medical problems need to be appropriately treated. The physical condition of the child and any comorbid conditions determine the subsequent steps in management.
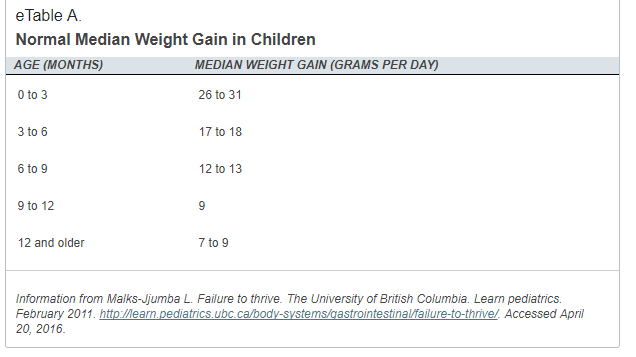
Catch-up growth will occur when the child gains at two to three times the average rate per age5 (eTable A).
eTable B shows one method for calculating catch-up calorie needs.
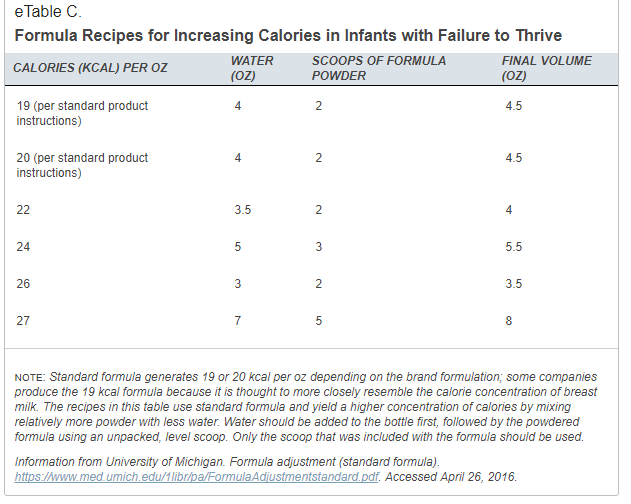
For infants, an evaluation of breastfeeding and lactation or an adjustment in formula concentration is indicated if inadequate caloric intake is responsible for FTT. eTable C shows formula recipes for increasing calories.
Without performing complicated calculations, most infants will tolerate increasing formula concentration from 19 to 24 kcal per oz. Caregivers of toddlers and older children should be counseled on nutrient-rich, healthy food choices, ideally provided in three meals and three snacks per day.5
Follow-up visits ranging from weekly to every few months are used to document weight, and the plan should be adjusted as the child progresses.
When weight is checked in the office, a routinely calibrated scale and consistent technique should be used.
Accelerated growth must be maintained for four to nine months to resolve FTT and achieve appropriate weight for height. Weight for height measurements above the 10th percentile with normal weight gain on two evaluations at least one month apart are reassuring for successful treatment.5 Relapses are possible, and continued observation is needed after successful completion of the frequent visit schedule. The risk of relapse is increased if the underlying etiology is not adequately addressed. Once FTT is resolved, patients require standard well visits with emphasis on monitoring for nutrition and growth.9,16
Accelerated growth must be maintained for four to nine months to resolve FTT and achieve appropriate weight for height. Weight for height measurements above the 10th percentile with normal weight gain on two evaluations at least one month apart are reassuring for successful treatment.5 Relapses are possible, and continued observation is needed after successful completion of the frequent visit schedule. The risk of relapse is increased if the underlying etiology is not adequately addressed. Once FTT is resolved, patients require standard well visits with emphasis on monitoring for nutrition and growth.9,16
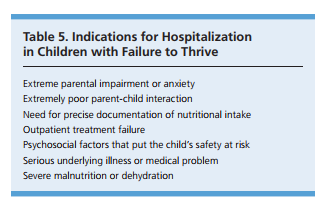
Hospitalization shouldbe considered if the child is at severe health risk. Hospitalization or subspecialist referral should be considered if intensive outpatient
treatment is ineffective after three to four months, or sooner for newborns.3
Children with complex medical, developmental, and social problems may show weight gain in the hospital setting because of the support of the highly trained multidisciplinary medical staff. Weight gain in the hospital does not necessarily confirm inadequate feeding or care by the family as the cause of FTT. Successful hospitalization requires careful integration of the child’s usual caretakers in the patient’s care and discharge planning [Emphasis Added].
Resources:
(1) Failure to Thrive: A Practical Guide [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Am Fam Physician. 2016 Aug 15;94(4):295-9.
(2) Growth Chart Recommendations From The Centers For Disease Control
- Use the WHO growth standards to monitor growth for infants and children ages 0 to 2 years of age in the U.S.
- Use the CDC growth charts for children age 2 years and older in the U.S.
(3) Formula adjustment (standard formula) [PDF]. Information from University of Michigan. This resource is from the Resource (1) article, eTable C above.