Because I have mostly practiced in critical access hospitals, my focus has always been how can we keep the critically ill patient alive and potentially salvageable until the helicopter arrives.
And the immediate appropriate treatment of shock is an important topic for clinicians working in critical access hospitals.
It is critical to defend the Mean Arterial Pressure (MAP). Do something immediately (meaning vasopressors) when the MAP goes low while you figure out the cause of the problem and treat it.*
*See Resource (4) EMCrit 201 – Deeper on Vasopressors and Athos 3 with Mink Chawla
June 12, 2017 by Scott Weingart
So first I’ll review (1) PulmCrit- Epinephrine challenge in sepsis: An empiric approach to catecholamines April 25, 2016 by Dr. Josh Farkas, which has an outstanding approach to the use of vasopressors. I’ve reviewed this post before in Practical Vasopressors And More In Septic Shock – Help From Drs. Farkas, Weingart, and Others Posted on June 17, 2017 by Tom Wade MD but it fits with (2) so I’ll review it again.
Then I’ll review (2) PulmCrit- High dose vasopressors: Never surrender
June 4, 2018 by Josh Farkas
And finally I’ll link to Dr. Weingart’s podcast (3) Podcast 87 – Mind of the Resuscitationist: Stop Points November 26, 2012.
As always these extracts are my study notes to help fix Dr. Farkas’ posts in my mind.
Here are extracts from (1) PulmCrit- Epinephrine challenge in sepsis: An empiric approach to catecholamines April 25, 2016 by Dr. Josh Farkas [but review the entire post – note to myself]:
Introductory case
A 55-year-old woman was admitted with toxic shock syndrome. Her norepinephrine requirement was labile, fluctuating between 15 mcg/min and 30 mcg/min. Bedside echocardiogram showed a dilated inferior vena cava without respiratory variability, and a normal ejection fraction. On examination her extremities were cool and her urine output was marginal.Epinephrine 4 mcg/min was added, with an improvement in blood pressure, perfusion, and urine output. She reported feeling better, and over the next hour the norepinephrine was weaned off. Her lactate increased from 2 mM to 6 mM. The ICU team was pleased with this epinephrine-induced rise in lactate, a positive prognostic sign. Sure enough, she continued to improve and was weaned off vasopressors entirely over the next 18 hours.
Foundational concept #1: Vasopressors don’t always behave according to the textbook.
Individual patients vary considerably in how they respond to vasopressors. Two factors in particular may contribute to this variability.
Endogenous sympathetic response
Variable end-organ sensitivity
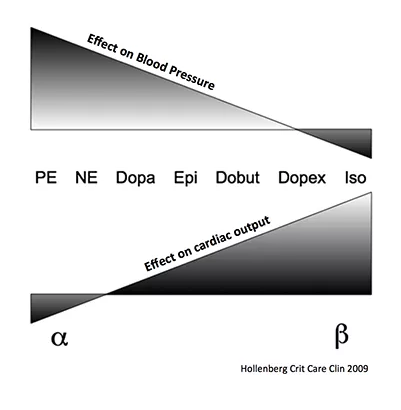
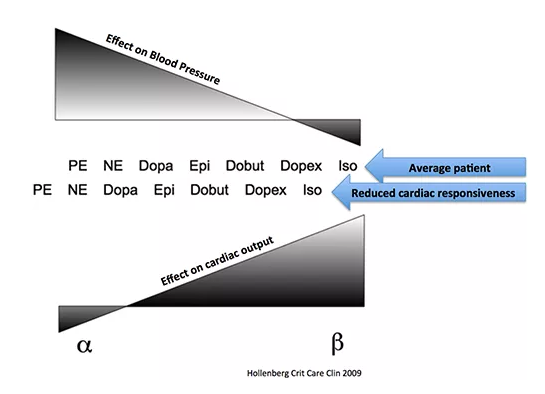
The differences between various catecholamines results from the ratio of stimulation of alpha-receptors vs. beta-receptors (figure below). However, patients vary in the responsiveness of their heart and vasculature. For example, reduced cardiac sensitivity to beta-agonists is common in advanced sepsis, due to receptor down-regulation. Refractory vasodilation is also well described.
Relative differences in end-organ sensitivity affect the way vasopressors function. For example, norepinephrine typically has predominantly vasoconstrictive effects with a small amount of isotropy. In a patient with reduced cardiac responsiveness to beta-agonist stimulation, this could cause the vasoconstrictive effects of norepinephrine to predominate even further. In this scenario, norepinephrine would have nearly the same effect as a pure vasoconstrictor such as phenylephrine:
Foundational concept #2: Norepinephrine and epinephrine are both evidence-based vasopressors for use in sepsis.
Although norepinephrine is typically first-line in septic shock, epinephrine is also a reasonable choice.
Groups of patients respond similarly to norepinephrine vs. epinephrine, but this doesn’t mean that individual patients will have the same response to either drug (an assumption exemplifying the flaw of averages). On the contrary, it is likely that some patients respond better to norepinephrine, while other patients respond better to epinephrine.
Groups of patients respond similarly to norepinephrine vs. epinephrine, but this doesn’t mean that individual patients will have the same response to either drug (an assumption exemplifying the flaw of averages). On the contrary, it is likely that some patients respond better to norepinephrine, while other patients respond better to epinephrine.
Foundational concept #3: The epinephrine hyper-responsive patient
Average responsiveness to norepinephrine vs. epinephrine
On average, equal doses of norepinephrine or epinephrine are required to achieve blood pressure targets.
The phenomenon of epinephrine hyper-responsiveness
Some patients seem to be especially responsive to epinephrine, with the following features: (3)
- They don’t respond very well to norepinephrine, often requiring high doses of norepinephrine. Sometimes the norepinephrine dose will fluctuate widely, suggesting that the norepinephrine isn’t very effective. While on norepinephrine, they may have poor perfusion.
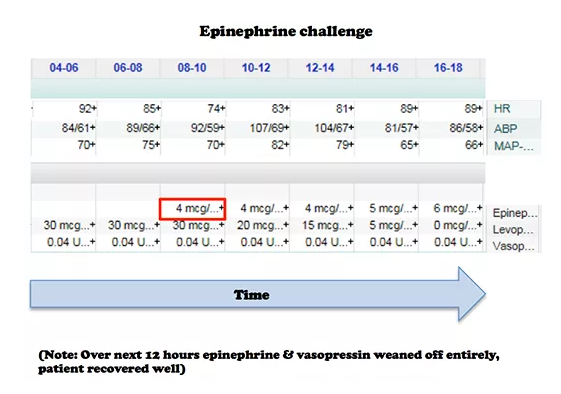
- They are very responsive to epinephrine. For example, the image below shows a patient who was transitioned from 30 mcg/min of norepinephrine to 6 mcg/min of epinephrine. Following transition to epinephrine, these patients often have improved perfusion.
- There is often an increase in lactate levels following the initiation of epinephrine, which is a positive prognostic sign (discussed below)(4).
Why are some patients epinephrine hyper-responsive?
The physiology of epinephrine hyper-responsiveness is likely multifactorial, perhaps with varying contributions from the following factors.
Factor #1: High endogenous alpha-adrenergic tone? A patient who is already quite vasoconstricted may respond poorly to additional exogenous alpha-adrenergic stimulation.
Factor #2: Relative bradycardia? Occasional patients in septic shock are encountered who have inappropriately normal heart rates (e.g. 50-70 b/m), even despite being on norepinephrine. This could relate to a deficiency of endogenous beta-adrenergic tone, or perhaps an over-reactive carotid baroreceptor response to alpha-adrenergic stimulation (5). Regardless, such patients might benefit from the stronger chronotropic effects of epinephrine.
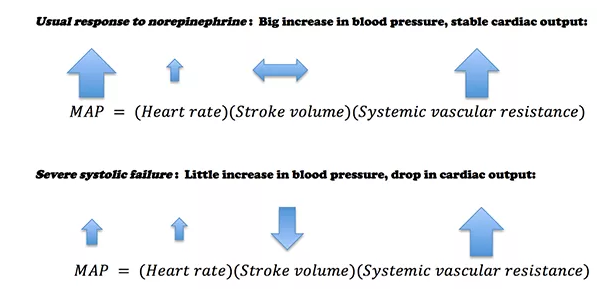
Factor #3: Occult systolic failure? An occasional septic patient has a normal ejection fraction, but after starting norepinephrine the ejection fraction drops. Why? Such patients have likely had systolic dysfunction all along. Initially their untreated vasodilation reduced their afterload, increasing their ejection fraction. Norepinephrine normalizes the afterload, thereby unmasking this systolic dysfunction.
Patients with occult systolic failure may experience less improvement in blood pressure in response to norepinephrine. In extreme cases, their cardiac output could even drop as the norepinephrine is titrated up (6):
Observational studies show that when patients with septic shock are treated with norepinephrine, some experience a decreased cardiac output (Hamzaoui 2010, Meadows 1988, Martin 1999).
Evaluating epinephrine responsiveness: The epinephrine challenge
Baseline hemodynamics and echocardiography provide static hemodynamic variables which usually cannot predict epinephrine responsiveness (7). Thus, the only way to be certain of how a patient will respond to epinephrine is to administer epinephrine. One potential exception might be a patient with marked tachycardia and a hyperkinetic ventricle.
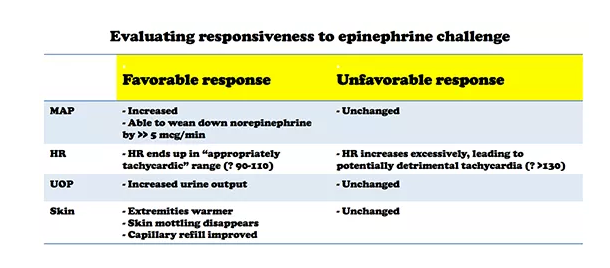
The best way to determine epinephrine responsiveness may be to simply start a low dose epinephrine infusion (e.g. 4 mcg/min)(8). The patient’s response to epinephrine may be judged based on clinical variables (table below). Although measuring cardiac output could also be performed, this is not my usual clinical practice (9).
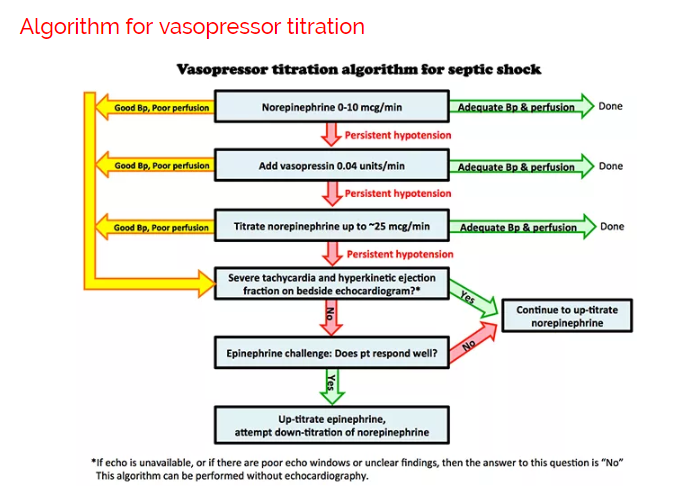
Above is one possible approach to titrating vasopressors in septic shock. Vasopressin is started earlier than in most algorithms (10). More notable features of the algorithm are:
- Epinephrine is trialed relatively early (before the patient is frankly “failing” norepinephrine).
- Many algorithms involve sequential addition of different vasopressors. However, it may also be useful to down-titrate vasopressors to which the patient responds poorly.
Here is an extract of (2) PulmCrit- High dose vasopressors: Never surrender
June 4, 2018 by Josh Farkas but you must read the whole post.
And finally after completely reviewing Resource (2)
This post is for use by only the most expert of clinicians – in a critical access hospital I would only consider using this strategy with help and agreement from the critical care specialist at the tertiary care where the patient is being transferred to.
Caution about using high-dose vasopressors
The above studies [reviewed in Dr. Farkas post] show a strong correlation between high-dose vasopressors and mortality. This is probably because the need for high-dose vasopressors correlates with greater disease severity, not because high-dose vasopressors cause mortality. Nonetheless, the need for high-dose vasopressors should never be taken lightly. This is generally a treatment of last resort. Whenever high-dose vasopressors are needed, meticulous evaluation is needed (ideally including echocardiography) with particular attention to the following questions:
- Is blood pressure truly that low? Consider placement of a femoral or axillary arterial catheter to transduce central arterial pressure.
- Is there a role for volume resuscitation or inotropic support? Some patients who respond poorly to norepinephrine may do better with epinephrine (see: epinephrine challenge).
- Is there occult right ventricular failure that could be treated (e.g. with pulmonary vasodilation)?
- Is there low cardiac output and impaired perfusion (e.g. mottling)? In that case, additional vasoconstriction may simply aggravate matters.
- Is there a failure of surgical source control or incorrect antibiotic selection?
- Is the patient on adequate adjunctive therapy (stress-dose steroid, possibly thiamine/ascorbate)?
- Is there a pH abnormality that merits correction (e.g. treatment of hyperchloremic metabolic acidosis with bicarbonate)?
- Is there autoPEEP or elevated intra-abdominal pressure which is impairing venous return?
- Is the patient on any medications which may be reducing the blood pressure (e.g. propofol, dexmedetomidine)?
- Is there clinically significant hypocalcemia?
Having reviewed Resources (1) and (2) above it is a good idea to listen to Dr. Weingart’s podcast Resource (3) Podcast 87 – Mind of the Resuscitationist: Stop Points [things to consider when you need to add a second vasopressor] November 26, 2012. This podcast reinforces with a clinical case, the points that Dr. Farkas made above in his posts.
Here are some excerpts from Dr. Weingart’s Stop Points podcast:
When you’re getting ready to add a second vasopressor, these are the points to consider and things to do:
Stop Points
- Volume – [Are you sure the paatient is adequately volume loaded]
- Calcium – [Check the ionized calcium as catecholamines won’t work in the face of low ionized calcium]
- Bleeding – [Is there occult bleeding that you haven’t diagnosed yet]
- Adrenal Insufficiency – [Consider stress dose of IV Solu-Cortef]
- Hypothyroidism – [See Myxedema Coma or Crisis
Updated: Mar 27, 2017 and Myxedema Coma or Crisis Treatment & Management Updated: Mar 27, 2017 from emedicine.medscaape.com.- Wacky stuff [Listen to the podcast]
Next Dr. Weingart states you should perform a RUSH exam [Link is to his show notes and podcast – definitely want to review this.
Resources:
(1) PulmCrit- Epinephrine challenge in sepsis: An empiric approach to catecholamines April 25, 2016 by Dr. Josh Farkas
(2) PulmCrit- High dose vasopressors: Never surrender
June 4, 2018 by Josh Farkas
(3) Podcast 87 – Mind of the Resuscitationist: Stop Points
November 26, 2012 by Scott Weingart
(4) EMCrit 201 – Deeper on Vasopressors and Athos 3 with Mink Chawla
June 12, 2017 by Scott Weingart