The following article, PulmCrit- Epinephrine challenge in sepsis: An empiric approach to catecholamines April 25, 2016 by Dr. Josh Farkas, has an outstanding approach to vasopressors. What follows is from this outstanding post [Read the whole post as there is much more in it–as always, these are just my study notes]:
Introductory case
A 55-year-old woman was admitted with toxic shock syndrome. Her norepinephrine requirement was labile, fluctuating between 15 mcg/min and 30 mcg/min. Bedside echocardiogram showed a dilated inferior vena cava without respiratory variability, and a normal ejection fraction. On examination her extremities were cool and her urine output was marginal.
Epinephrine 4 mcg/min was added, with an improvement in blood pressure, perfusion, and urine output. She reported feeling better, and over the next hour the norepinephrine was weaned off. Her lactate increased from 2 mM to 6 mM. The ICU team was pleased with this epinephrine-induced rise in lactate, a positive prognostic sign. Sure enough, she continued to improve and was weaned off vasopressors entirely over the next 18 hours.
Variable end-organ sensitivity
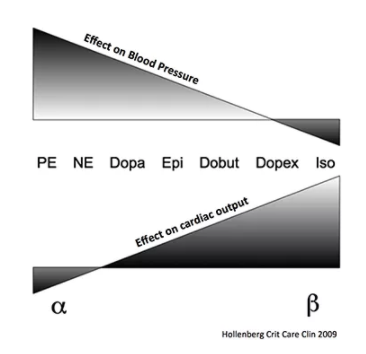
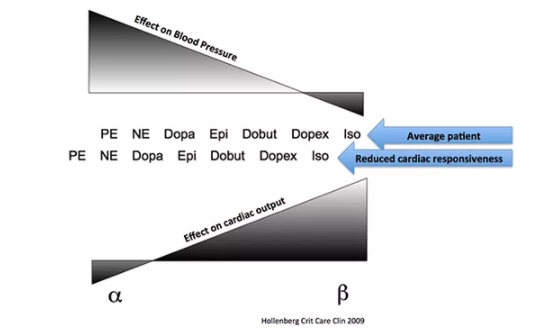
The differences between various catecholamines results from the ratio of stimulation of alpha-receptors vs. beta-receptors (adjacent figure). However, patients vary in the responsiveness of their heart and vasculature. For example, reduced cardiac sensitivity to beta-agonists is common in advanced sepsis, due to receptor down-regulation. Refractory vasodilation is also well described.
Relative differences in end-organ sensitivity affect the way vasopressors function. For example, norepinephrine typically has predominantly vasoconstrictive effects with a small amount of isotropy. In a patient with reduced cardiac responsiveness to beta-agonist stimulation, this could cause the vasoconstrictive effects of norepinephrine to predominate even further. In this scenario, norepinephrine would have nearly the same effect as a pure vasoconstrictor such as phenylephrine:
Evaluating epinephrine responsiveness: The epinephrine challenge
Baseline hemodynamics and echocardiography provide static hemodynamic variables which usually cannot predict epinephrine responsiveness (7). Thus, the only way to be certain of how a patient will respond to epinephrine is to administer epinephrine. One potential exception might be a patient with marked tachycardia and a hyperkinetic ventricle.
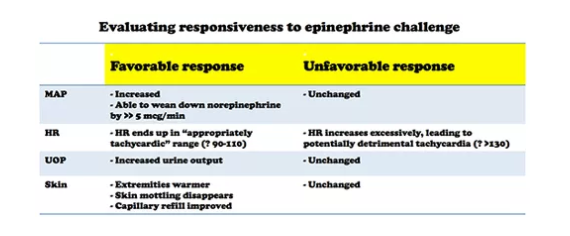
The best way to determine epinephrine responsiveness may be to simply start a low dose epinephrine infusion (e.g. 4 mcg/min)(8). The patient’s response to epinephrine may be judged based on clinical variables (table below). Although measuring cardiac output could also be performed, this is not my usual clinical practice (9).
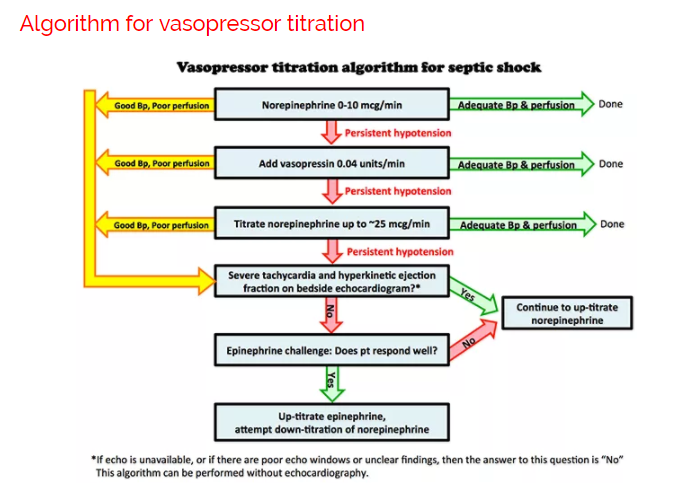
Above is one possible approach to titrating vasopressors in septic shock. Vasopressin is started earlier than in most algorithms (10). More notable features of the algorithm are:
- Epinephrine is trialed relatively early (before the patient is frankly “failing” norepinephrine).
- Many algorithms involve sequential addition of different vasopressors. However, it may also be useful to down-titrate vasopressors to which the patient responds poorly.
Summary:
- Epinephrine and norepinephrine are both acceptable, evidence-based approaches to hemodynamic support in septic shock.
- Individual patient responsiveness to vasopressors is variable and unpredictable.
- Some patients respond better to epinephrine than norepinephrine.
- For patients who are not responding well to norepinephrine, it is reasonable to empirically trial a low dose of epinephrine (“epinephrine challenge”).
The following article, Chawla: Vasopressors- Time to target new receptors? [Show notes from Vidcast] [Vidcast On Vimeo] July 14, 2016 from The Maryland Critical Care Project, is outstanding [Again, read the whole show notes]. Here are some excerpts:
Rules of Critical Care
Defend blood pressure
- “True” hypotension is an emergency
- MAP<65 needs attention IMMEDIATELY
- Hypotension → Decreased DBP → Decreased coronary blood flow → Cardiac ischemia → Decreased CO → Hypotension (repeat)
- Short durations hurt brain, kidneys, heart
- Longer durations of hypotension = worse outcomes
- Push dose, immediate fluids, etc.
- FIX IT!
You MUST diagnose shock
- Always identify which type of shock!*
- Stabilize/Defend BP
- Assessment of CO → Diagnose shock type
- Volume trial → Look for CO improvement
[*Types of Shock: Obstructive, Distributive, Hypovolemic, or/and Cardiogenic
- Obstructive: pulmonary embolus, cardiac tamponade, tension pneumothorax
- Distributive: Septic shock, neurogenic shock
- Hypovolemic: Bleeding, Fluid Loss From Dehydration
- Cardiogenic: Cardiomyopathy from ischemia, sepsis, and other causes.]
The choice of vasopressors is not always clear
Be sure to read all five of Dr. Farkas’ posts in Resources below for an outstanding and relatively brief review of vasopressors.
And of course Dr. Weingart’s podcasts, 138 and 201, are great.
Resources:
Early norepinephrine to stabilize MAP in septic shock October 6, 2014 by Dr. Josh Farkas of PulmCrit
Renoresuscitation: Sepsis resuscitation designed to avoid long-term complications December 7, 2014 by Dr. Josh Farkas PulmCrit
PulmCrit- Epinephrine challenge in sepsis: An empiric approach to catecholamines April 25, 2016 by Dr. Josh Farkas of PulmCrit
Renal microvascular hemodynamics in sepsis: a new paradigm
December 2, 2014 by Dr. Josh Farkas of PulmCrit
Pulmcrit – Renoresuscitation, vasopressin, vepinephrine, and VANISH
August 15, 2016 by Dr Josh Farkas of PulmCrit
The role of vasoactive agents in the resuscitation of microvascular perfusion and tissue oxygenation in critically ill patients [PubMed Abstract] [Full Text HTML] [Full Text PDF] Intensive Care Med. 2010 Dec; 36(12): 2004–2018. Published online 2010 Sep 2. doi: 10.1007/s00134-010-1970-x PMCID: PMC2981743
EMCrit 201 – Deeper on Vasopressors and Athos 3 with Mink Chawla [Link is to podcast and show notes] June 12, 2017 by Scott Weingart from EMCrit.org.
Podcast 138 – Vasopressor Basics [Link is to the show notes and podcast] December 1, 2014 by Scott Weingart from EMCrit.org