Today, I review, link to, and excerpt from The Journal Of Cardiovascular Development And Disease’s “Coronary CT Angiography in the Emergency Department: State of the Art and Future Perspectives” [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. J Cardiovasc Dev Dis. 2025 Jan 27;12(2):48. doi: 10.3390/jcdd12020048.
All that follows is from the above resource.
Abstract
About 5% of annual access to emergency departments (EDs) and up to 25–30% of hospital admissions involve patients with symptoms suggestive of acute coronary syndrome (ACS). The process of evaluating and treating these patients is highly challenging for clinicians because failing to correctly identify an ACS can result in fatal or life-threatening consequences. However, about 50–60% of these patients who are admitted to the hospital because of chest pain are found to have no ACS. Coronary computed tomographic angiography (CCTA) has emerged as a proposed new frontline test for managing acute chest pain in the ED, particularly for patients with low-to-intermediate risk. This narrative review explores the potential of adopting an early CCTA-based approach in the ED, its significance in the era of high-sensitivity troponins, its application to high-risk patients and its prognostic value concerning atherosclerotic burden and high-risk plaque features. Additionally, we address clinical and technical issues related to CCTA use for triaging acute chest pain in the ED, as well as the role of functional testing. Finally, we aim to provide insight into future perspectives for the clinical application of CCTA in the ED.
Keywords: coronary computed tomographic angiography, emergency department, acute chest pain, acute coronary syndrome, coronary artery disease 1. Introduction
About 5% of annual access to the emergency department (ED) and up to 25–30% of hospital admissions involve patients with symptoms suggestive of acute coronary syndrome (ACS) [1]. The process of evaluating and treating these patients is highly challenging for clinicians because failing to correctly identify an ACS can result in fatal or life-threatening consequences [2]. However, about 50–60% of patients presenting with acute chest pain are found to have no ACS [3,4]. This over-triage carries considerable economic consequences, with related costs of around USD 14 billion for the United States healthcare system [5]. Furthermore, this overcrowding in the ED has been associated with worse clinical outcomes for acute chest pain patients, making rapid triage essential for both health and economic reasons [6,7]. From this perspective, coronary computed tomography angiography (CCTA) has been proposed to enhance decision-making in the ED for patients with no known previous coronary artery disease (CAD). Considering the high accuracy of CCTA in ruling out CAD, it allows a rapid evaluation of the degree of coronary atherosclerosis, drastically reducing the time-to-discharge of patients without significant CAD and ensuring more appropriate referral for invasive coronary angiography (ICA) and myocardial revascularization [8,9,10,11].
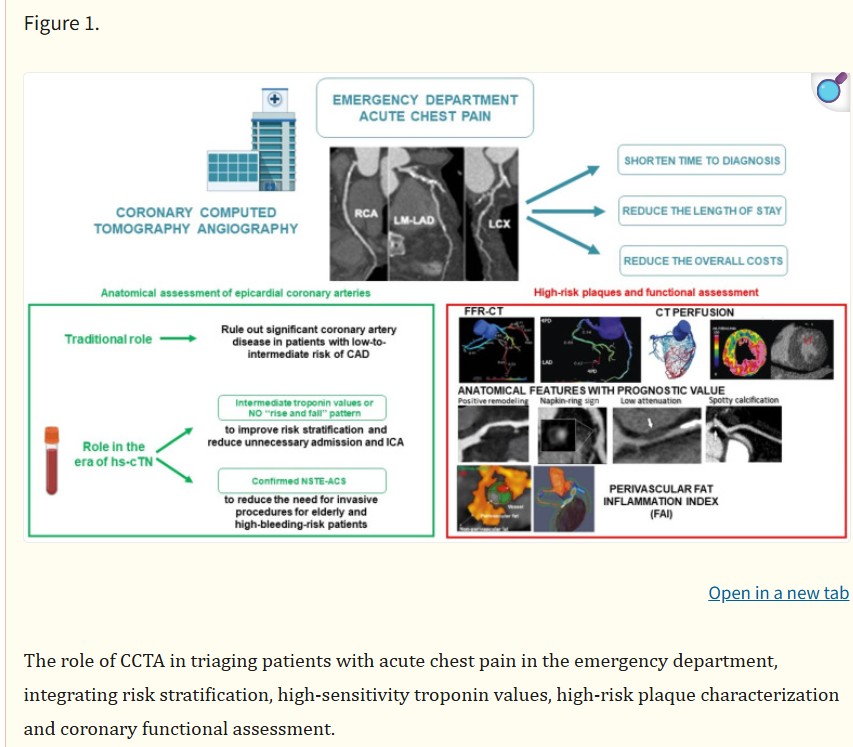
In this review, we explore the potential of an early CCTA-based strategy for patients with chest pain in the ED setting, its significance in the era of high-sensitivity troponins and its application for high-risk patients. Additionally, we discuss the prognostic value of the atherosclerotic burden, the high-risk plaque features and the role of functional testing in the acute setting.
2. Coronary CT Angiography-Based Approach in the Emergency Department
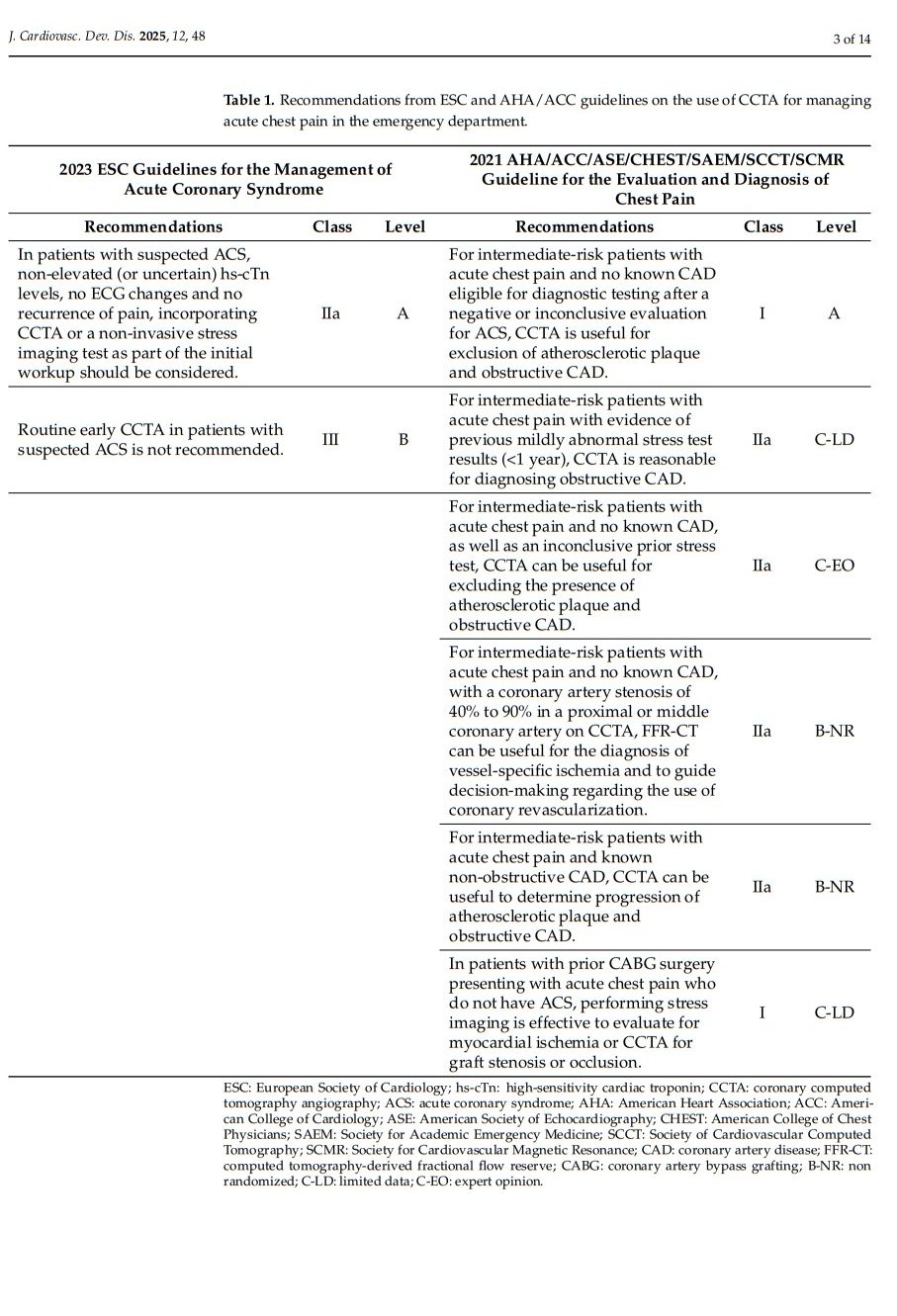
Extensive recent evidence and current guidelines support CCTA as a first-line imaging strategy for the rapid triage of low-to-intermediate risk patients presenting with acute chest pain to the ED (Table 1). The main advantages of an anatomical CCTA-based approach in the ED setting include its ability to (1) quickly rule out significant CAD in low-to-intermediate-risk patients thanks to its high sensitivity and negative predictive value; (2) shorten the time-to-diagnosis; (3) decrease the ED length-of-stay; (4) reduce the overall cost of care.
Firstly, data from the ROMICAT trial showed that, among patients presenting to the ED with acute chest pain and in whom the initial assessment was inconclusive, CCTA accurately excluded ACS in 71% of cases, demonstrating the absence of significant CAD (with a negative predictive value of 100%) [9]. Other studies suggest that a CCTA-based strategy for low-to-intermediate-risk patients presenting with suspected ACS allows for the safe and rapid discharge of about 50% of these patients, who would otherwise be admitted [8,9,10,11].
Secondly, both in the ROMICAT II trial and in the CT-STAT trial, the CCTA implementation in patients presenting with typical chest pain led to a 44% and 55% reduction in time-to-diagnosis, respectively, compared with rest/stress myocardial perfusion imaging (MPI) [12,13].
Thirdly, the ROMICAT II trial demonstrated that using CCTA significantly reduced ED length-of-stay by approximately 7 h and led to a higher rate of direct discharge from the ED, enhancing efficiency without compromising patient outcomes [13]. Similarly, in the CT-COMPARE trial, the implementation of CCTA was associated with a reduction in ED length-of-stay by approximately 6 h [14]. In all these studies, CCTA was used as a complement to clinical assessments, including troponins and risk scores. These parameters were crucial for stratifying patient risk and interpreting CCTA findings. Combining CCTA with traditional markers, rather than using CCTA alone, may enhance early triage and discharge decisions, providing a comprehensive patient evaluation and improving diagnostic accuracy. Furthermore, it is important to note that the study population primarily consisted of individuals with a low-to-intermediate risk profile and with a mean age under 60 years, which may influence the accuracy metrics. Across these studies, the sensitivity and specificity data are influenced by the prevalence of CAD, patient age and associated calcification levels. Older populations, with a higher burden of calcification, are more likely to experience higher false-positive rates. This context should be considered when interpreting the diagnostic accuracy metrics reported for CCTA in these trials and applying the result to older populations.
Lastly, in the CT-COMPARE trial, a CCTA-based strategy in patients presenting to the ED with acute chest pain led to a 20% reduction in hospital costs compared with the ECG exercise stress test [14]. This cost reduction encompassed all inpatient and outpatient costs associated with the index admission, including labor, diagnostics, pathology, pharmaceuticals, bed days and consumables, while excluding societal and opportunity costs. These findings were confirmed by the CT-STAT trial which demonstrated a 38% reduction in overall healthcare costs for patients assigned to the CCTA group compared to those in the MPI group [12]. Economic evaluations of CCTA often rely on key assumptions regarding the cost of the procedure, including reimbursement rates, operational efficiency and resource allocation within healthcare systems. These analyses also account for downstream cost savings from avoiding unnecessary hospital admissions, invasive procedures or additional testing. However, variations in local pricing, scanner availability and staffing requirements can significantly influence the economic outcomes.
Furthermore, CCTA offers several advantages compared to other diagnostic techniques available for managing patients with suspected ACS. In particular, it can detect the presence of other causes of chest pain (i.e., coronary artery abnormalities, aortic dissection and extra-cardiac causes), thus allowing clinicians to promptly initiate appropriate treatments [15,16].
2.1. Coronary CT Angiography in the Era of High-Sensitivity Troponins
Over the years, conventional cardiac troponin (cTn) tests have been largely replaced by high-sensitivity cardiac troponin (hs-cTn) assays in most centers. These hs-cTn assays have a higher negative predictive value (NPV), so normal levels can effectively exclude the presence of an ACS in ED patients presenting with acute chest pain [17,18]. However, the trade-off of this increased sensitivity is reduced specificity, meaning that hs-cTn assays can yield positive results not only in cases of myocardial infarction but also in various critical conditions associated with myocardial injury [19,20]. In these cases, the addition of CCTA beyond high-sensitivity troponin assays may be necessary to determine the underlying cause of chest pain and guide appropriate management.
In a study conducted in 500 patients, the use of CCTA was associated with less outpatient testing and lower direct medical costs compared to standard optimal care encompassing hs-cTn assays [21]. However, the BEACON study showed that CCTA did not improve the identification of patients, with significant CAD requiring coronary revascularization, nor did it reduce hospital stay or increase the rate of direct discharge from the ED [21].
Other studies provided promising evidence for the potential benefits of integrating CCTA into the ED setting, particularly for patients with intermediate levels of hs-cTn or without a significant “rise and fall” pattern [22,23].
The PRECISE-CTCA study showed that in patients presenting to the ED because of acute chest pain, in whom intermediate hs-cTn concentrations were found (between 5 ng/L and the sex-specific 99th percentile), there is a higher probability of CAD compared to those with low hs-cTn concentrations (<5 ng/L). In this specific subgroup of patients, CCTA may help identify those with occult CAD or with high-risk plaques, thereby improving clinical outcomes [24].
In a study by Ferencik et al., early advanced CCTA assessment (involving not only the degree of stenosis but also the plaque features) combined with hs-cTn evaluation may improve risk stratification and diagnostic accuracy in patients with suspected ACS and intermediate hs-cTn levels [25]. In these patients, the absence of coronary stenosis ≥ 50% and high-risk plaque ruled out ACS (ACS rate 0%), whereas patients with both stenosis ≥ 50% and high-risk plaque were at high risk for ACS (ACS rate 69.2%).
Finally, the COURSE trial is an ongoing study that aims to determine whether an early CCTA may be more efficient than standard care in patients with inconclusive high-sensitivity troponin results. Preliminary goals include reducing unnecessary hospital admissions and ICA [26].
2.2. Coronary CT Angiography for the Subgroup of High-Risk Patients
Although CCTA finds its greatest application in ED patients at low-to-intermediate risk, it might also be useful in high-risk patients presenting with acute chest pain.
Several studies have investigated the role of CCTA in patients presenting to the ED with a clinical picture of non-ST-segment elevation acute myocardial infarction (NSTEMI), demonstrating that CCTA may significantly reduce the need for ICA in a large number of cases [22,27]. It is especially advantageous for patients at greater risk of complications from invasive procedures, such as older individuals or those with a high risk of bleeding [27].
In the VERDICT trial, CCTA maintains high accuracy to rule out clinically significant CAD (defined as stenosis ≥ 50%) in patients with documented NSTEMI with a per-patient NPV of 91% [28]. Furthermore, it was observed that approximately one-third of patients with NSTEMI had no clinically significant CAD, indicating the potential role of coronary CTA to safely defer ICA in nearly one-third of these high-risk cases, with no increase in major adverse cardiovascular events (MACE) after a median follow-up of 4 years [28].
Other studies confirmed these results, showing that an early CCTA may reduce the need for ICA in NSTEMI patients by approximately 30 to 40%, compared with routine clinical care [29].
2.3. The Prognostic Value of Atherosclerosis Burden and High-Risk Plaques
Over the last few years, CCTA has gained additional prognostic value beyond merely assessing the severity of coronary stenosis. Indeed, CCTA performed in the ED setting also enables the evaluation of atherosclerotic burden and the presence of high-risk plaque features, both of which are associated with unfavorable outcomes (Figure 1).