What follows are links to and excerpts from Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Eur Heart J. 2013 Sep;34(33):2636-48, 2648a-2648d. doi: 10.1093/eurheartj/eht210. Epub 2013 Jul 3.
Clinical Presentation
Myocarditis presents in many different ways, ranging from mild symptoms of chest pain and palpitations associated with transient ECG changes to life-threatening cardiogenic shock and ventricular arrhythmia (Table 3). The disease may affect individuals of all ages, although it is most frequent in the young. This diversity of clinical scenarios implies that the diagnosis of myocarditis requires a high level of suspicion early in the course of the disease and the use of appropriate investigations to identify its cause. In all cases of suspected myocarditis, it is mandatory to exclude coronary artery disease and other cardiovascular, e.g. hypertension, or extra-cardiac non-inflammatory diseases that could explain the clinical presentation. Rarely patients with other cardiovascular disorders such as coronaryartery disease,cardiomyopathy, and hypertensive heart disease present with a clinical deterioration caused by myocarditis that is mistakenly attributed to the natural history of the preexisting disease. If this is stronglycsuspected by the clinician, further investigation including EMB may be appropriate.
Diagnosis of Myocarditis
Non-invasive imaging techniques such as cardiac magnetic resonance (CMR) imaging can be useful in making the diagnosis of myocarditis and for monitoring disease progression, but we strongly endorse the concept that EMB should be the gold standard for the diagnosis of definite myocarditis.1–3However,this implies that allpatients with suspected
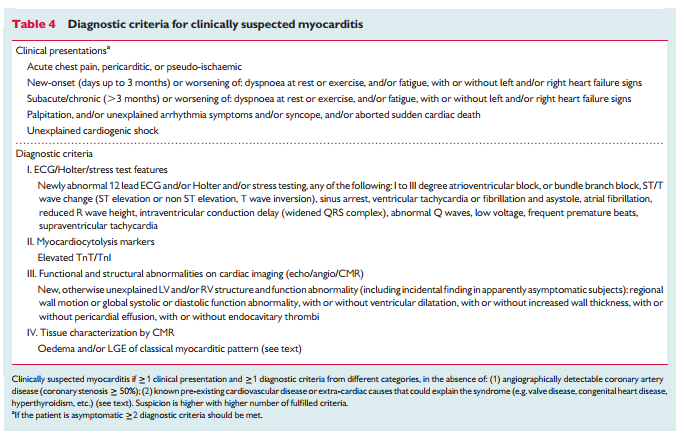
myocarditis should undergo an EMB which is not routine practice; moreover, current guidelines recommend EMB only in a limited number of clinical scenarios that do not include some common presentations of myocarditis, in particular, pseudo-infarction.120 In order to improve recognition of myocarditis in clinical practice and to aid selection of patients that require further diagnostic evaluation and treatment, we propose new criteria for clinically suspected myocarditis for which biopsy analysis is recommended (Table 4). These criteria are based upon consensus of experts and require validation in future multicentre registries and randomized trials in patients who have undergone EMB.Medical centres that cannot safely perform EMB or do not have access to state-of-the-art CMR should refer patients with clinically suspected myocarditis to a tertiary referral unit experienced in EMB and CMR, particularly when patients present with haemodynamic instability or life-threatening arrhythmia [Emphasis Added].
Proposed criteria for clinically suspected myocarditis
In this position statement, we propose new criteria for the diagnosis of clinically suspected myocarditis. These are based on a clinical presentation consistent with the diagnosis (Table 3) and the presence of one or more abnormalities on non-invasive testing (Table 4).
Myocarditis should be suspected in the presence of: 1 or more of the clinical presentations in Table 4, with or without ancillary features (see below),
and
1 or more of the diagnostic criteria from different categories (I to IV) in Table 4
or
when the patient is asymptomatic, 2 or more diagnostic criteria from different categories (I to IV).
Ancillary features which support the clinical suspicion of myocarditis include:
- Fever ≥38.08C at presentation or within the preceding 30 days with or without evidence of a respiratory (chills, headache, muscle aches, general malaise) or gastrointestinal (decreased appetite, nausea, vomiting, diarrhoea) infection;
- peri-partum period121;
- previous clinically suspected or definite myocarditis (according to the criteria set in Table 4);
- personal and/or family history of allergic asthma, other types of allergy, extra-cardiac autoimmune disease, toxic agents;
- family history of DCM, myocarditis (according to the present criteria).
Firstline tests in patients with a clinical presentation consistent with myocarditis [See pages 2641 – 2645 for detailed discussion of each of the recommendations.]
Recommendations
- Standard 12-lead electrocardiogram should be performed in all patients with clinically suspected myocarditis
- All patients with clinically suspected myocarditis should undergo a standard trans-thoracic echocardiogram at presentation.
- Trans-thoracic echocardiogram should be repeated during hospitalization if there is any worsening of haemodynamics.
- Nuclear imaging is not routinely recommended in the diagnosis of myocarditis, with the possible exception of suspected cardiac sarcoidosis.
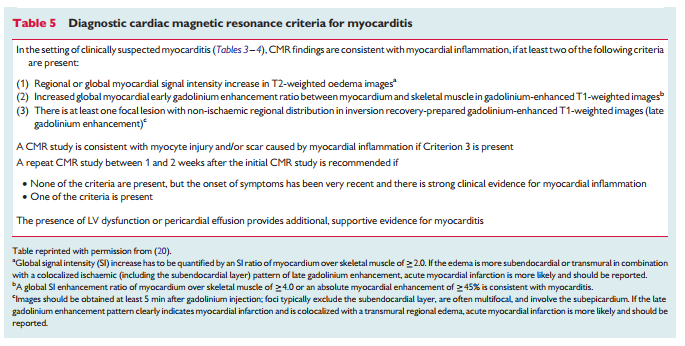
- Cardiovascular magnetic resonance findings consistent with myocarditis should be based on Lake-Louise criteria (Table 5) [See Table 5 after #13 of this list].
- Cardiovascular magnetic resonance may be considered in clinically stable patients prior to EMB. Cardiovascular magnetic resonance does not replace EMB in the diagnosis of myocarditis and should not delay EMB in life-threatening presentations.
- Troponins, erythrocyte sedimentation rate, reactive C protein levels should be assessed in all patients.
- Routine viral serology testing is not recommended.
- Serum samples should be assessed, if possible, for cardiac aabs, if one (or more) of the published tests is available (Table 2), according to specific centre expertise. Disease specific aabs should preferably be tested
- All patients with clinically suspected myocarditis should be considered for selective coronary angiography and EMB
- Tissue obtained from EMB should be analysed using histology, immunohistochemistry, and viral PCR (on heart tissue and a blood sample).
- At least three myocardial samples, each 1–2 mm in size, should be taken (from the right or from the left ventricle) and immediately fixed in 10% buffered formalin at room temperature for light microscopy; additional samples should be taken, snap frozen in liquid nitrogen, and stored at 2808C, or stored in RNA later tubes at room temperature, for viral PCR.2,149
- Endomyocardial biopsy may be repeated if necessary to monitor response to aetiology-directed therapy, or if a sampling error is suspected in a patient with unexplained progression of heart failure.
Second level investigations in clinically suspected myocarditis
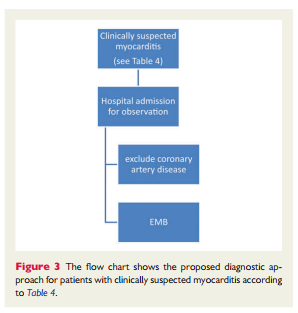
In patients fulfilling the diagnostic criteria for clinically suspected myocarditis, we recommend selective coronary angiography and EMB (Figure 3). This recommendation also applies to patients with an acute coronary syndrome-like presentation (with or without ST segment elevation),increased cardiac troponins, preserved ventricular systolic function with or without features suggestive of myocarditis on CMR (Figure 1).20 At present, there are limited data on the prognostic implications ofCMR findings inthis context,and this common scenario was not included in a recently published AHA/ACC/HFSA scientific statement on EMB.120 Therefore, in the absence of robust prospective data (in suspected myocarditis with pseudo-infarct presentation and normal coronary arteries), the definitive diagnosis of myocarditis should still be based on EMB (Figure 3).
Endomyocardial biopsy
Endomyocardial biopsy confirms the diagnosis of myocarditis and identifies the underlying aetiology and the type of inflammation (e.g. giant cell, eosinophilic myocarditis, sarcoidosis) which imply different treatments and prognosis (Figure 1).1 – 3,11,14 – 16 Importantly, EMB is also the basis for safe (infection negative) immunosuppression and antiviral treatment. If EMB is performedbyexperienced teams, its complication rate is low (0–0.8).9,18,139,148
The recent scientific statement on EMB gave highest levels of recommendations in the life-threatening clinical presentations.120 However, the diagnostic, prognostic, and therapeutic value of EMB was based on the Dallas histopathologic criteria and did not include immunohistochemistry and viral genome analysis (Figure 1). These are established tools which should be used to achieve an aetiological diagnosis.9,14 – 16,18,19,22,26,30 – 32,100,101,103,133,137,138
To optimize diagnostic accuracy and reduce sampling error in focal myocarditis, EMB should be performed early in the course of the disease and multiple specimens should be taken.2
Resources:
(1) Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Eur Heart J. 2013 Sep;34(33):2636-48, 2648a-2648d. doi: 10.1093/eurheartj/eht210. Epub 2013 Jul 3.