This post discusses the Lung Ultrasound Profiles of the BLUE protocol from BLUE-protocol and FALLS-protocol: two applications of lung ultrasound in the critically ill [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Chest. 2015 Jun;147(6):1659-70. doi: 10.1378/chest.14-1313.
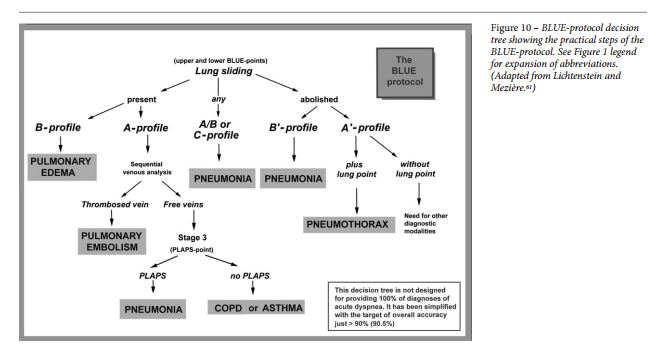
The Lung Ultrasound Profiles are used in the decision tree from the article:
The interpretation of lung ultrasound in acute respiratory failure requires the mastery of ten lung ultrasound signs [See post Lung Ultrasound Signs]:
- Normal lung surface
- bat sign
- lung sliding
- A-lines
- Pleural effusion
- Quad sign
- Sinusoid sign
- Lung consolidation
- Fractal sign (also called the shred sign)
- Tissue-like sign
- Interstitial syndrome
- Lung rockets
- Pneumothorax
- Stratosphere sign
- lung point sign
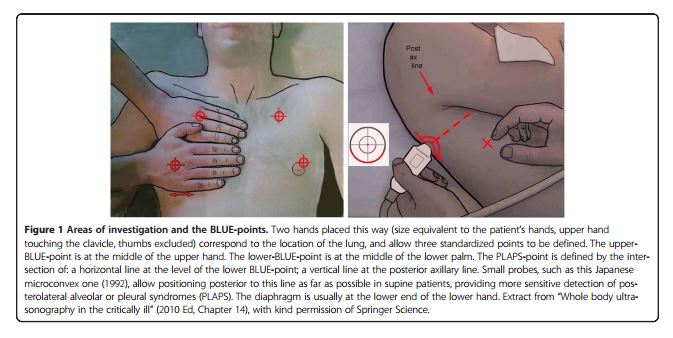
These lung signs are determined at standard points on the chest (Ref 4 below):
There are eight lung profiles discussed in the article:
- A-profile
- Anterior A-lines present with lung sliding
- A’-profile
- Anterior A lines present with absent lung sliding
- B-profile
- Lung sliding with lung rockets
- B’-profile
- Absent lung sliding with lung rockets
- A/B-profile
- Unilateral lung rockets
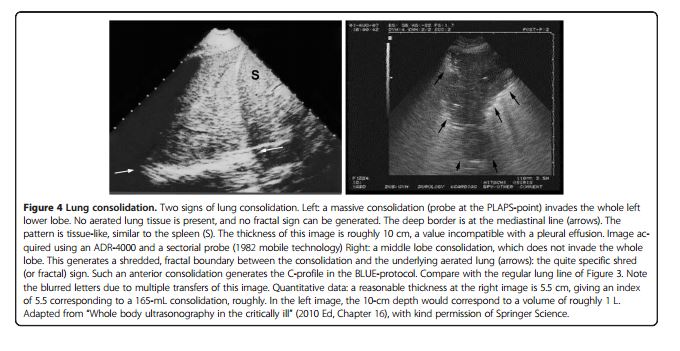
- C-profile – See fig 4 below from Reference 4
- “Anterior lung consolidation regardless of number and size up to simply a thick irregular pleural line”
- Posterior consolidations are seen in hemodynamic pulmonary edema or pulmonary embolism
- “PLAPS” profiles*: “At the posterior chest wall, lung consolidations and pleural effusions are assessed together for simplicity because both disorders usually come together, hence the practical term “PLAPS”
- “The A-no-V-PLAPS-profile is connected with pneumonia.”
- “The A-profile with no DVT and no PLAPS (ie, nude profile) is linked with asthma and COPD (two bronchial diseases with similar therapy combined for simplification.”
Lung Consolidation from Reference 4:
The following are excerpts from the above article:
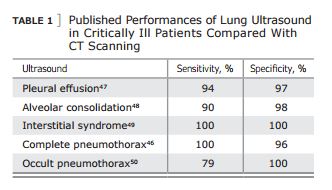
. . . all acute, life-threatening [lung] disorders are superficial. This allows to standardize the field ( Table 1 ).
The BLUE-protocol was developed based on the study of 300 consecutive adults with acute respiratory failure who were admitted to our ICU and given a diagnosis. The most frequent cause of respiratory failure was:
- pneumonia (32%)
- followed by acute hemodynamic pulmonary edema (24%);
- exacerbated COPD (18%);
- severe asthma (13%);
- pulmonary embolism (8%);
- pneumothorax (4%);
- and countless rare causes, including easy-to-diagnose ones, such as massive pleural eff usion (3%).
- We excluded rare, unknown, and multiple diagnoses because they generate methodologic issues.
The BLUE-protocol is integrated within the control of acute respiratory failure, which requires an understanding of anatomy, physiology, pathophysiology, clinical signs, traditional imaging, and the biology of dyspnea. Th e BLUE-protocol is fully based on pathophysiology.
Additional Resources:
(1) BLUE-protocol and FALLS-protocol: two applications of lung ultrasound in the critically ill [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Chest. 2015 Jun;147(6):1659-70. doi: 10.1378/chest.14-1313.
(2) Lung Ultrasound in the Critically Ill Neonate [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Curr Pediatr Rev. 2012 Aug;8(3):217-223.
(3) Clinically integrated multi-organ point-of-care ultrasound for undifferentiated respiratory difficulty, chest pain, or shock: a critical analytic review ([PubMed Abstract] [Full Text HTML] [Full Text PDF]. J Intensive Care. 2016 Aug 15;4:54. doi: 10.1186/s40560-016-0172-1. eCollection 2016.)
(4) Lung ultrasound in the critically ill. Ann Intensive Care. 2014 Jan 9;4(1):1. doi: 10.1186/2110-5820-4-1. [PubMed Abstract] [Full Text HTML] [Full Text PDF]