Today, I reviewed, linked to, and excerpted from Measurement of Blood Pressure in Humans: A Scientific Statement From the American Heart Association [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Hypertension. 2019 May;73(5):e35-e66. doi: 10.1161/HYP.0000000000000087.
All that follows is excerpted from the above resource.
Jump to
- Abstract
- BP Components
- BP Measurement in the Office
- Twenty-Four–Hour ABPM
- Home BP Monitoring
- Contrasting ABPM and HBPM
- Special BP Measurement Techniques
- BP Measurement in Other Settings
- BP Measurement Considerations in Special Populations
- BP Variability
- Protocols for the Validation of BP Monitors
- Device Calibration
- Summary
- Disclosures
- Footnotes
- References
Abstract
The accurate measurement of blood pressure (BP) is essential for the diagnosis and management of hypertension. This article provides an updated American Heart Association scientific statement on BP measurement in humans. In the office setting, many oscillometric devices have been validated that allow accurate BP measurement while reducing human errors associated with the auscultatory approach. Fully automated oscillometric devices capable of taking multiple readings even without an observer being present may provide a more accurate measurement of BP than auscultation. Studies have shown substantial differences in BP when measured outside versus in the office setting. Ambulatory BP monitoring is considered the reference standard for out-of-office BP assessment, with home BP monitoring being an alternative when ambulatory BP monitoring is not available or tolerated. Compared with their counterparts with sustained normotension (ie, nonhypertensive BP levels in and outside the office setting), it is unclear whether adults with white-coat hypertension (ie, hypertensive BP levels in the office but not outside the office) have increased cardiovascular disease risk, whereas those with masked hypertension (ie, hypertensive BP levels outside the office but not in the office) are at substantially increased risk. In addition, high nighttime BP on ambulatory BP monitoring is associated with increased cardiovascular disease risk. Both oscillometric and auscultatory methods are considered acceptable for measuring BP in children and adolescents. Regardless of the method used to measure BP, initial and ongoing training of technicians and healthcare providers and the use of validated and calibrated devices are critical for obtaining accurate BP measurements.
Keywords: AHA Scientific Statements; blood pressure; hypertension; monitoring, ambulatory.
BP Measurement in the Office
Overview
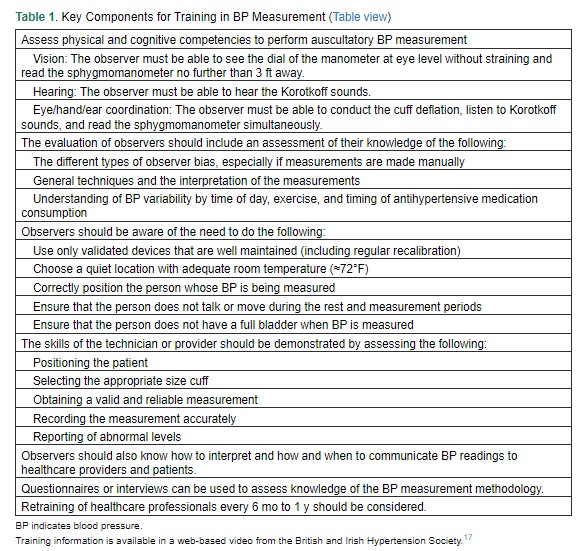
In the office setting, BP is measured noninvasively in 2 ways. The traditional method involves auscultation of the brachial artery with a stethoscope to detect the appearance and muffling or disappearance of the Korotkoff sounds, which represent SBP and DBP, respectively.14 Over the past 20 to 30 years, the oscillometric technique, wherein software within a device evaluates the oscillometric waveforms, commonly during BP cuff deflation, and uses algorithms to estimate BP, has been developed and refined.15 Regardless of who is measuring BP or the method used (eg, auscultatory or oscillometric), the accuracy of the BP readings relies on standardized techniques and appropriate observer training. Sources of BP measurement error include patient-related (eg, recent food consumption, movement), device-related (eg, using a noncalibrated or nonvalidated device) and procedure-related (eg, talking during the procedure or miscuffing) factors. The use of an inaccurate measurement technique is common, and a systematic review found a large bias associated with 27 of 29 potential sources of BP measurement error.16Table 1 lists key components of observer training for BP measurement.
Key Points for Accurately Measuring Office BP
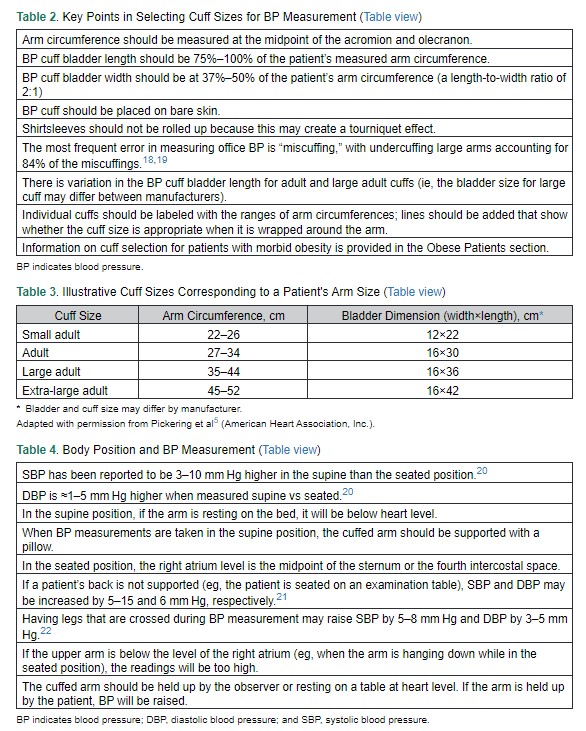
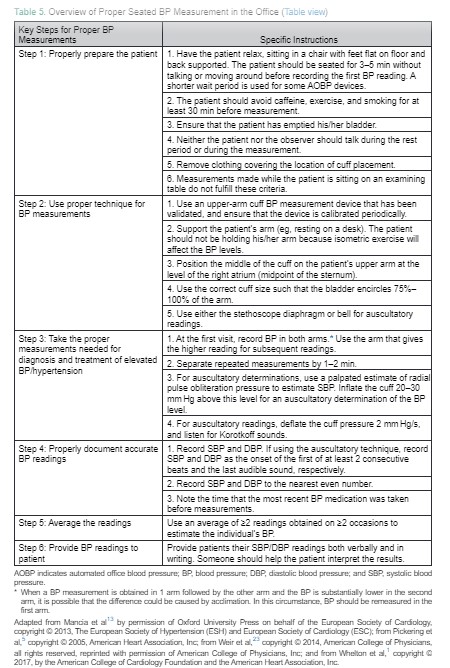
An initial step in measuring BP is determining the appropriate cuff size (Tables 2 and 3). BP measurement is most commonly made in either the seated or the supine position. Seated measurements are preferred given the large amount of data correlating BP obtained in this position with outcomes. Regardless of whether BP is measured in the seated or supine position, the BP cuff should be at the level of the patient’s right atrium (Table 4). Other key points related to proper BP measurement from the 2017 Hypertension Clinical Practice Guidelines are provided in Table 5. Using a cuff that is too small will result in an artificially elevated BP reading, and using a cuff that is too large will result in a reading that is artificially low.16 Other effects on SBP and DBP from not following measurement recommendations are provided in a recent systematic review.16
To determine cuff size, patients should measure their arm circumference at the midpoint of the upper arm. The bladder length should be 75% to 100% of the arm circumference, and bladder width should be 37% to 50% of the arm circumference. *
*For Accurate Blood Pressure Measurement, Cuff Size Matters
Kenny Lin, MD, MPH
Posted on August 21, 2023. American Family PhysicianCuff Placement and Stethoscope
The observer must first palpate the brachial artery in the antecubital fossa and place the center of the bladder length of the cuff (commonly marked on the cuff by the manufacturer) so that it is over the arterial pulsation of the patient’s bare upper arm. The lower end of the cuff should be 2 to 3 cm above the antecubital fossa. When an auscultatory measurement is being taken, this allows room for placement of the stethoscope. However, if the bladder is not long enough to sufficiently encircle the arm (75%–100% for auscultatory measurements), a larger cuff should be used, recognizing that if the cuff touches the stethoscope, artifactual noise will be generated.24 The cuff should be pulled taut, with comparable tightness at the top and bottom edges of the cuff, around the bare upper arm. To assess the appropriate tightness, 1 finger should fit easily at the top and bottom of the cuff; 2 fingers should fit but will be very snug. When taking an auscultatory measurement, the cuff should initially be inflated to at least 30 mm Hg above the point at which the radial pulse disappears. Cuff deflation should occur at a rate of 2 mm Hg per second or per heartbeat when the heart rate is very slow to obtain an accurate estimate of BP.
The Oscillometric Technique
Oscillometric devices are commonly used to measure BP in clinic, ambulatory, home, and hospital settings, with readings based on the amplitude of the oscillations recorded in the lateral walls of the upper arm. Most oscillometric devices estimate BP when the cuff is being deflated, but some devices obtain estimates on inflation. Mean arterial BP is estimated to be the cuff pressure when the oscillation amplitude is maximal, and then the SBP and DBP are computed.5,34,38 SBP and DBP estimation from mean arterial BP is commonly performed via fixed ratios of the maximal oscillation amplitude. Each oscillometric device uses a proprietary algorithm that is known only to the manufacturer. These algorithms can be modified by the device manufacturer, and there are no requirements for such changes to be reported. Therefore, different devices, even from the same manufacturer, are not interchangeable, and only those that have been independently validated with an established protocol should be used (see the Protocols for the Validation of BP Monitors section).39
Automated Office BP
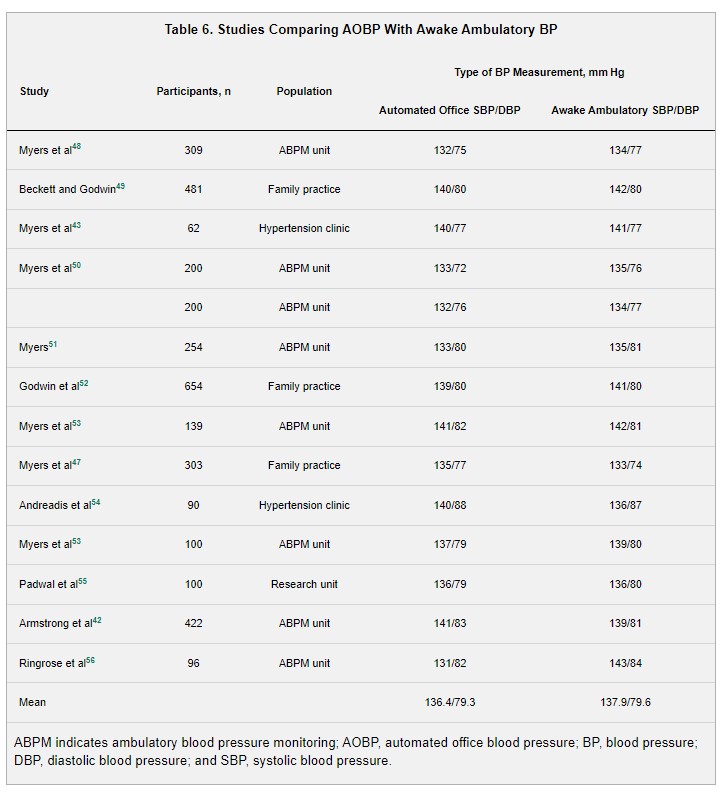
AOBP monitors refers to those with the capability to record multiple BP readings after a rest period with a single activation. Current AOBP devices provide an average of these readings, and it is not necessary to discard the first reading. AOBP can be performed with or without staff being present, which is referred to as attended and unattended AOBP, respectively. Valid unattended AOBP readings can be obtained with the patient resting quietly in an office examination room or waiting room,42 with readings taken in different locations reported to be comparable.43 Several AOBP oscillometric devices have been validated and used in research studies.44–46AOBP as an Alternative to Auscultatory BP in Clinical Practice
Several studies have reported that BP measured with AOBP versus the auscultatory method is closer to awake out-of-office BP levels measured with ambulatory BP monitoring (ABPM). . . . AOBP has also demonstrated a stronger association with subclinical CVD, including intima-media thickness of the carotid artery58 and left ventricular mass index, compared with BP measured with the auscultatory technique by a research technician.54 Among adults not taking antihypertensive medication, a graded increased risk for fatal and nonfatal CVD events has been reported with AOBP from an SBP of 110 to 119 to ≥160 mm Hg and from a DBP of 60 to 69 to ≥90 mm Hg.59,60 In adults taking antihypertensive medication, on-treatment SBP measured with an AOBP device without an observer present (unattended AOBP) in the range of 110 to 119 mm Hg has been associated with the lowest CVD event rate.61
AOBP in Population Studies and Clinical Practice
As a result of the limitations of routine auscultatory BP measurement in clinical practice, including reliance on the observer’s skills, white-coat effect, digit preference, and calibration issues, AOBP recently became the recommended method for diagnosing hypertension and managing BP among patients with hypertension in the Canadian guidelines.62 Its adoption into primary care has proved feasible in Canada with minimal increases in staff time and effort.63 The total time required for conducting AOBP is 4 to 6 minutes, including a 1-minute or no rest period before the first measurement, versus a 7- to 8-minute duration, including a 5-minute rest period before the first measurement, for auscultatory and semiautomated devices. A major advantage is the reduced need for staff presence during BP measurement. The Canadian guidelines include a recommendation for AOBP to be conducted with staff absent (unattended AOBP) from the room during BP measurement.62. . . . Considering the current shift away from manual BP measurement and the recommendation to obtain multiple BP readings at a single visit, AOBP may be preferred for use in clinical practice. Because having an observer present when BP readings are obtained may lead to inaccurate values (eg, if the patient or observer is talking), it is preferred to have the patient in a room alone for BP measurements (ie, unattended AOBP).
Number of Measurements During a Visit
For many people, the first BP measurement taken during an office visit is higher than subsequent measurements. A study of US adults estimated that 35% of people with SBP/DBP on their first BP measurement of 140 to 159/90 to 99 mm Hg had SBP/DBP <140/90 mm Hg when the average of 3 measurements was used.68 In addition, 24% of participants with SBP/DBP of 120 to 139/80 to 89 mm Hg based on their first clinic measurement had SBP/DBP <120/80 mm Hg based on the average of their second and third measurements. Only 3% of people with SBP/DBP <140/90 mm Hg based on a single measurement had SBP/DBP ≥140/90 mm Hg based on the average of 3 measurements. In a study of men taking antihypertensive medication, at least 5 BP measurements were needed to be 80% certain whether SBP was <140 mm Hg or not.69 The 2017 Hypertension Clinical Practice Guidelines recommend measuring BP ≥2 times at a clinic visit.1
Interarm Differences
Guidelines recommend that BP should be measured in each arm at an initial visit and that the arm with the higher BP should be used at subsequent visits.13a Persistent differences in measured BP between the arms that would be considered clinically significant (ie, SBP or DBP difference ≥10 mm Hg) are quite common. A large difference might be caused by coarctation of the aorta or upper-extremity arterial obstruction. A systematic review of simultaneously measured SBP in both arms found a pooled prevalence of an interarm difference in SBP ≥10 mm Hg of 11.2% (95% CI, 9.1–13.6) among those with hypertension and 3.6% (95% CI, 2.3–5.0) in the general population.70 Although poorly reproducible, except in the presence of arterial obstruction, larger interarm BP differences have been associated with increased risk for CVD events.71–73 When BP is measured sequentially in a person’s arms (ie, a measurement in 1 arm followed by the other arm) and the BP is substantially lower in the second arm, it is possible that the difference could be the result of acclimation. In this circumstance, BP should be remeasured in the first arm. When a persistent difference in BP between arms is present, the diagnosis of hypertension should be based on BP measured in the arm with the higher level.
Frequency of Visits
To increase hypertension awareness, it is reasonable to measure BP at every clinic visit. However, for screening for hypertension in adults, measuring BP annually as opposed to at every clinical visit improves specificity for diagnosing hypertension without a reduction in sensitivity.74 Adults 18 to 39 years of age with office-measured SBP/DBP <120/80 mm Hg who do not have other hypertension risk factors can space the screenings out to every 3 to 5 years. The US Preventive Services Task Force recommends annual BP screening for adults at increased risk for hypertension.2 This would include patients with elevated BP who are overweight or obese or black. For a patient with SBP/DBP ≥160/100 mm Hg at an office visit, the diagnosis of hypertension can be made and treatment can be initiated without follow-up readings.1 For most other adult patients, the finding of office BP consistent with hypertension at an initial visit should be confirmed at a follow-up visit within 1 month, with ≥2 BP measurements at each visit. In addition, the US Preventive Services Task Force and the 2017 Hypertension Clinical Practice Guidelines recommend confirmation of office BPs by ABPM or home BP monitoring (HBPM) for the initial diagnosis of hypertension and BP control (see the Twenty-Four–Hour ABPM and the Home BP Monitoring sections). In addition, it is reasonable to reassess BP after 3 to 6 months of nonpharmacological therapy among patients with elevated BP (SBP 120–129 mm Hg with DBP <80 mm Hg). For patients with established hypertension taking antihypertensive medication, the 2017 Hypertension Clinical Practice Guidelines recommend having patients return at approximately monthly intervals after initiating/titrating antihypertensive medication until their goal BP is reached.1 This aligns with the intervals for the first 3 months after randomization in the Systolic Blood Pressure Intervention Trial.75 Once BP is at goal, visits can be conducted at 3- to 6-month intervals.1
Reproducibility of Mean Office BP
Because BP varies beat-to-beat, perfect reproducibility of mean office BP is not possible. Routine office BP measurements obtained in clinical practice with the auscultatory method demonstrate substantial variability. Therefore, low reproducibility is present over visits conducted days to weeks (short term) and months to years (long term) apart.76–78 Evidence suggests that high-quality, standardized office BP measurements, as typically obtained in research studies, with the auscultatory or the oscillometric method have better reproducibility than routine office BP obtained in real-world practice settings.79–81 Although few data are available, AOBP has demonstrated high short-term reproducibility.43
Normative Values for Office BP
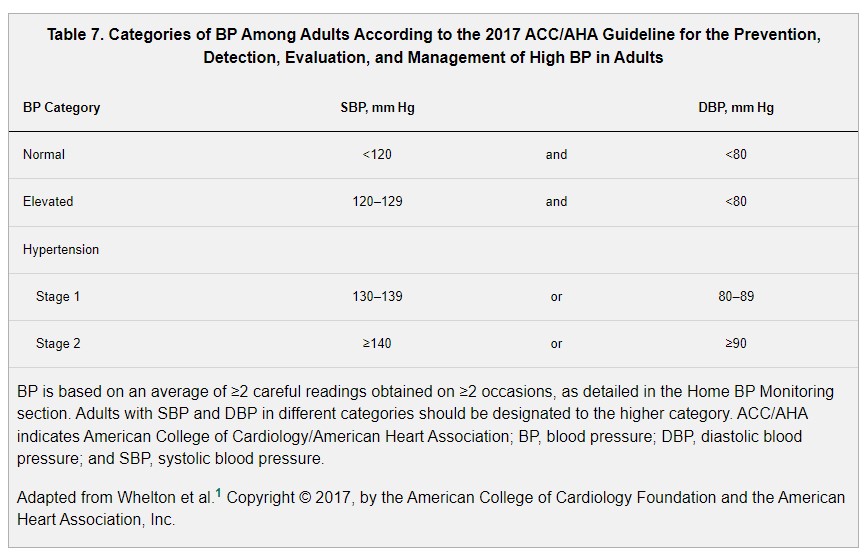
The 2017 Hypertension Clinical Practice Guidelines provided a new categorization of BP levels. This guideline defined BP categories of normal, elevated, or stage 1 or 2 hypertension (Table 7). SBP/DBP thresholds of 130/80 mm Hg now define the diagnosis of hypertension. Estimates from the 2011 to 2014 National Health and Nutrition Examination Survey indicate that 42.3% and 12.1% of US adults have normal and elevated BP, respectively, and 45.6% have hypertension.82