The following are some pearls from the 2003 MMWR Managing Acute Gastroenteritis Among Children: Oral Rehydration, Maintenance, and Nutritional Therapy*.
“Dehydration and electrolyte losses associated with untreated diarrhea cause the primary morbidity of acute gastroenteritis. Diarrhea can be among the initial manifestations of nongastrointestinal illnesses, including meningitis, bacterial sepsis, pneumonia, otitis media, and urinary tract infection. Vomiting alone can be the first symptom of metabolic disorders [like diabetic ketoacidosis], congestive heart failure, toxic ingestions, or trauma [or other serious diseases such as meningitis, brain tumor, urinary tract infection, and surgical emergencies (pyloric stenosis, intussception, malrotation, inguinal hernia)]. To rule out other serious illnesses, a detailed history and physical examination should be performed as part of the evaluation of all children with acute gastroenteritis.”
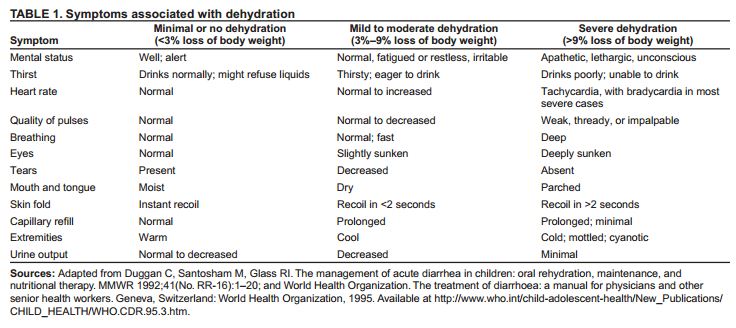
“. . . , distinguishing between mild and moderate dehydration on the basis of clinical signs alone may be difficult. Therefore, these updated recommendations group together patientswith mild to moderate dehydration and specify that the signs of dehydration and specifythat might be apparent over a relatively wide range of fluid loss (i.e., from 3%-9%) (Table1). The goal of assessment is to provide a starting point for treatment and to conservatively determine which patients can be sent home for therapy, which ones should remain for observation during therapy, and which ones should immediately receive more intensive therapy.”
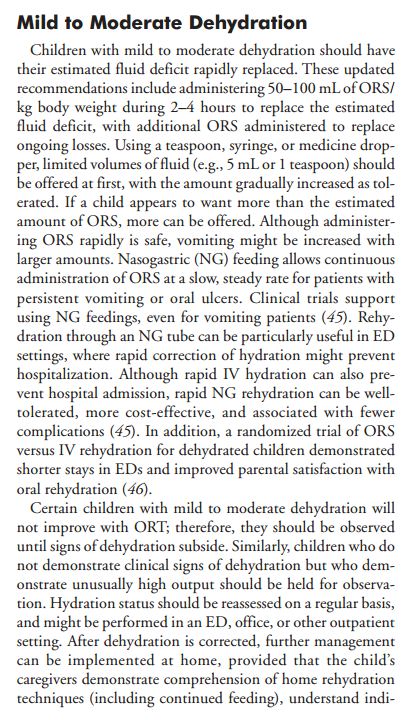
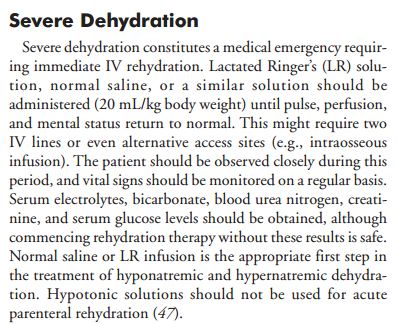 “With frail or malnourished infants, smaller amounts (10 mL/kg body weight) are recommended because of the reduced ability of these infants to increase cardiac output and because distinguishing dehydration from sepsis in these patients.”
“With frail or malnourished infants, smaller amounts (10 mL/kg body weight) are recommended because of the reduced ability of these infants to increase cardiac output and because distinguishing dehydration from sepsis in these patients.”
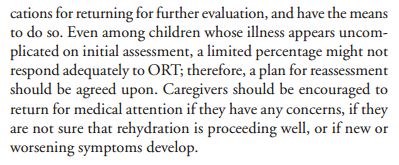
“A lack of response to fluid administration should raise the suspicion of alternative or concurrent diagnoses, including septic shock and metabolic, cardiac, or neurologic disorders.”
“As soon as the severely dehydrated patient’s level of consciousness returns to normal, therapy can usually be changed to the oral route, with the patient taking by mouth the remaining deficit.”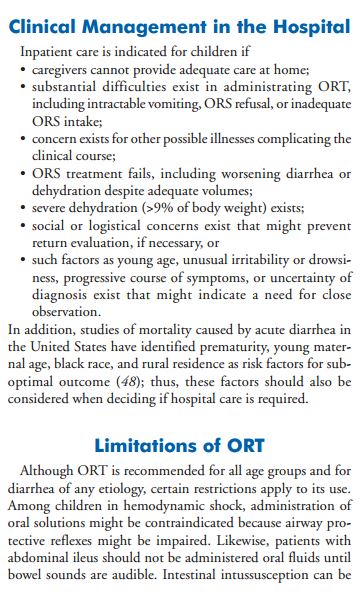
 Source:
Source:
*MMWR, Managing Acute Gastroenteritis Among Children. Nov. 21, 2003, Vol. 52