All of what follows are figures, tables, and quotes from the 2009 European Society of Cardiology (ESC) Syncope Guidelines*:
“The initial evaluation of a patient presenting with T-LOC consists of careful history, physical examination, including orthostatic BP measurements, and electrocardiogram (ECG). Based on these findings, additional examinations may be performed:
-
CSM in patients >40 years.
-
Echocardiogram when there is previous known heart disease or data suggestive of structural heart disease or syncope secondary to cardiovascular cause.
-
Immediate ECG monitoring when there is a suspicion of arrhythmic syncope.
-
Orthostatic challenge (lying-to-standing orthostatic test and/or head-up tilt testing) when syncope is related to the standing position or there is a suspicion of a reflex mechanism.
-
Other less specific tests such as neurological evaluation or blood tests are only indicated when there is suspicion of non-syncopal T-LOC.”
“The initial evaluation should answer three key questions:
-
Is it a syncopal episode or not?
-
Has the aetiological diagnosis been determined?
-
Are there data suggestive of a high risk of cardiovascular events or death?”
2.1.1 Diagnosis of syncope
“The differentiation between syncope and non-syncopal conditions with real or apparent LOC can be achieved in most cases with a detailed clinical history,66–68 but sometimes can be extremely difficult.”
“The following questions should be answered:
-
Was LOC complete?
-
Was LOC transient with rapid onset and short duration?
-
Did the patient recover spontaneously, completely and without sequelae?
-
Did the patient lose postural tone?”
“If the answers to these questions are positive, the episode has a high likelihood of being syncope. If the answer to one or more of these questions is negative, exclude other forms of LOC before proceeding with syncope evaluation.”
2.1.2 Aetiological diagnosis
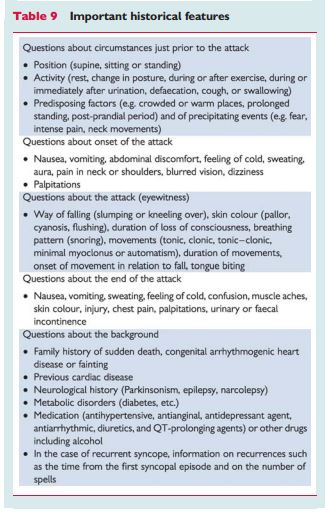
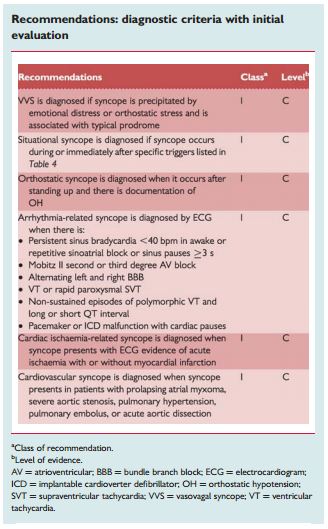
“Initial evaluation is able to define the cause of syncope in 23–50% of patients.33,69 Table 9 lists some of the most important questions that must be answered by the clinical history. There are some findings in the clinical history, physical examination, or ECG that can be considered diagnostic of the cause of syncope, permiting [I think the authors mean requiring] no further evaluation and [permitting the immediate] institution of treatment.”
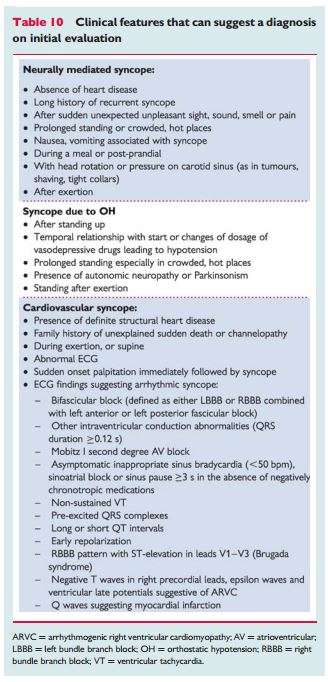
“In many other situations, the findings of initial evaluation do not permit a definite diagnosis to be made, but suggest some causes (Table 10). In these cases, additional testing is usually needed.”
2.1.3 Risk stratification
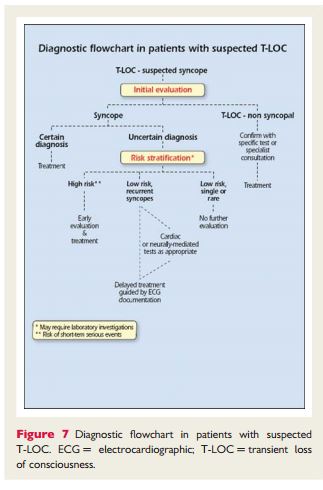
“When the cause of syncope remains uncertain after initial evaluation the next step is to assess the risk of major cardiovascular events or SCD.Figure 7 shows the diagnostic flow chart to be followed in these patients.”
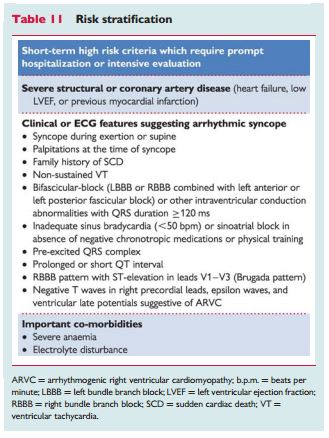
“The main high risk features, in accordance with recent guidelines on SCD and cardiac pacing,70–73 are listed in Table 11.”
2.2 Diagnostic tests
2.2.1 Carotid sinus massage
“It has long been observed that pressure at the site where the common carotid artery bifurcates produces a slowing in HR and fall in BP. In some individuals, this reflex initiated by CSM results in an abnormal response. A ventricular pause lasting >3 s and/or a fall in systolic BP of >50 mmHg defines carotid sinus hypersensitivity (CSH). When associated with spontaneous syncope, CSH defines CSS. Precise methodology and results of CSM are reported in the previous guidelines on syncope.1 Diagnosis of CSS requires the reproduction of spontaneous symptoms during 10 s sequential right and left CSM performed supine and erect, under continuous monitoring of HR and periodic measurement of BP, permitting better evaluation of the vasodepressor component.74 In up to 30% of patients, an abnormal reflex is present only in the upright position. It should be stressed that CSH is a common finding in older male individuals,8 but patients with CSS are more unusual.75 CSS is exceptional in patients <40 years old.74 ”
“The relationship between abnormal response to CSM and syncope is a crucial point that has been studied by two different methods. The first was a pre–post comparison of the recurrence rate of syncope after pacing. Non-randomized studies demonstrated fewer recurrences at follow-up in patients implanted than in patients without pacing, and these results were confirmed by two randomized trials.76,77 The second method was to analyse the occurrence of asystolic episodes registered in patients with cardioinhibitory response to CSM by an implanted device. In the two trials that employed this methodology, recordings of long pauses were very common.78,79 These results suggest that a positive response to CSM in patients with syncope is highly predictive of the occurrence of spontaneous asystolic episodes.”
“The main complications of CSM are neurological. Pooling the data of three studies74,80,81 in which 7319 patients were analysed, neurological complications were observed in 21 (0.29%). CSM should be avoided in patients with previous TIA, stroke within the past 3 months, or with carotid bruits, except if carotid Doppler studies excluded significant stenosis.80“
2.2.2 Orthostatic challenge
“Changing from supine to upright position produces a displacement of blood from the thorax to the lower limbs that leads to a decrease in venous return and CO. In the absence of compensatory mechanisms, a fall in BP may lead to syncope.82“
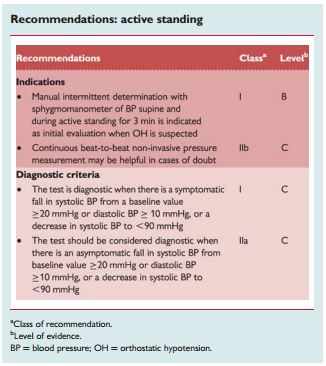
“Currently, there are two different methods for assessing the response to change in posture from supine to erect11 (Table 5).”
“One is ‘active standing’, in which patients arise actively from supine to erect, and the other is head up tilt at 60 or 70°.”
2.2.2.1 Active standing
“This test is used to diagnose different types of orthostatic intolerance; see section 1.2.2.2 and Table 5.”
“The sphygmomanometer is adequate for routine clinical testing because of its ubiquity and simplicity. Automatic arm-cuff devices, as they are programmed to repeat and confirm measurements when discrepant values are recorded, may be a disadvantage due to the rapidly falling BP during OH. With a sphygmomanometer more than four measurements per minute cannot be obtained without venous obstruction in the arm. When more frequent values are required continuous beat-to-beat non-invasive BP measurement can be used.”
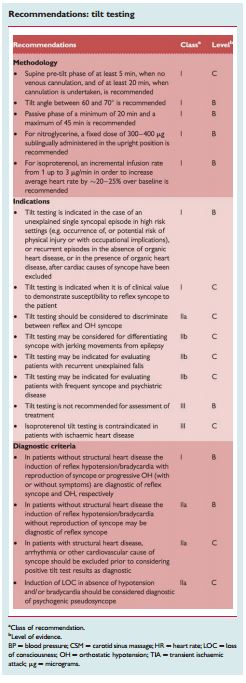
2.2.2.2 Tilt testing
Background
“Tilt testing enables the reproduction of a neurally mediated reflex in laboratory settings. Blood pooling and decrease in venous return due to orthostatic stress and immobilization trigger the reflex. The final effect, hypotension and usually concomitant HR slowing, is related to impaired vasoconstrictor capability followed by sympathetic withdrawal and vagal overactivity.”
“The clinical situation corresponding to tilt testing is reflex syncope triggered by prolonged standing. However, this test can also be positive in patients with other forms of reflex syncope83 and in patients with sick sinus syndrome.84“
Methodology
“Tilt testing was introduced into clinical evaluation of patients with syncope of unknown origin by Kenny et al. in 1986.85 Since then, many protocols have been reported with variations in the initial stabilization phase, duration, tilt angle, type of support, and different pharmacological provocation. The sensitivity and specificity of different protocols are described in detail in different reviews.1,86“
“The most commonly used protocols are the low-dose intravenous isoproterenol test, which uses incremental doses in order to increase average HR by ∼20–25% over baseline (usually ≤3 µg/min)87 and the protocol using 300–400 µg of sublingual nitroglycerine after a 20 min unmedicated phase.88 In older patients omission of the passive phase and commencing the test with nitroglycerine may be effective and improve compliance.89 Both protocols have a similar rate of positive responses (61–69%), with a high specificity (92–94%). Patients should be fasted for 4 h prior to the test. Due to the need for venous cannulation in the isoproterenol protocol a pre-tilt phase of stabilization of 20 min is required, whereas with sublingual nitroglycerine the pre-tilt phase can be shortened to 5 min.”
Indications
“In most studies the main indication for tilt testing has been to confirm a diagnosis of reflex syncope in patients in whom this diagnosis was suspected but not confirmed by initial evaluation.85–89“
“Tilt testing is not usually needed in patients whose reflex syncope is already diagnosed by clinical history and in patients with single or rare syncope unless special situations (e.g. injury, anxiety, occupational implications such as aircraft pilots, etc.). In patients with a high risk profile for cardiovascular events or with data suggestive of arrhythmic syncope, tilt testing has been reported to be useful when a cardiovascular cause has been reasonably excluded by a comprehensive evaluation. In patients with T-LOC associated with jerking movements tilt testing has been demonstrated to be helpful in discriminating syncope from epilepsy.90 Tilt testing has been used in patients with frequent episodes of T-LOC and suspicion of psychiatric problems, even with traumatic injury, to investigate the reflex nature of the syncope.91 Similarly, tilt testing has been used in the elderly in order to distinguish syncope from falls.92”
“The pattern of response to tilt testing has recently been used to discriminate pure reflex syncope from non-classical forms of delayed OH (see Table 5).14”
“Tilt testing has no value in assessing the treatment efficacy.93 However tilt table testing is widely accepted as a useful tool to demonstrate susceptibility of the patient to reflex syncope, and thereby to initiate treatment (e.g. physical manoeuvres, see Part 3).94–96”
Responses to tilt testing
“The endpoint of tilt testing is the induction of either reflex hypotension/bradycardia or delayed OH associated with syncope or pre-syncope. When a reflex is induced, according to the predominance of vasodepressor or cardioinhibitory components, the responses have been classified as cardioinhibitory, vasodepressor, or mixed.97 A negative tilt table response does not exclude the diagnosis of reflex syncope. The clinical significance of the type of response to tilt testing in predicting the behaviour of BP and HR during spontaneous syncope has recently been questioned.98,99 Some studies have compared the response to tilt testing with spontaneous syncope recorded by implantable loop recorder (ILR). While a positive cardioinhibitory response to tilt testing predicts with a high probability an asystolic spontaneous syncope, the presence of a positive vasodepressor or mixed response or even a negative response does not exclude the presence of asystole during spontaneous syncope.98,99“
Complications and contraindications
“Tilt testing is safe. There have been no reported deaths during the test. However, some rare life-threatening ventricular arrhythmias with isoproterenol in the presence of ischaemic heart disease100 or sick sinus syndrome101 have been reported. No complications have been published with the use of nitroglycerine. Minor side effects are common and include palpitations with isoproterenol and headache with nitroglycerine. Atrial fibrillation can be induced during or after a positive tilt test and is usually self-limited.102 Despite the low risk, it is recommended that resuscitation equipment should available.”
“Contraindications to the administration of isoproterenol include ischaemic heart disease, uncontrolled hypertension, left ventricular outflow tract obstruction, and significant aortic stenosis. Caution should be used in patients with known arrhythmias.”
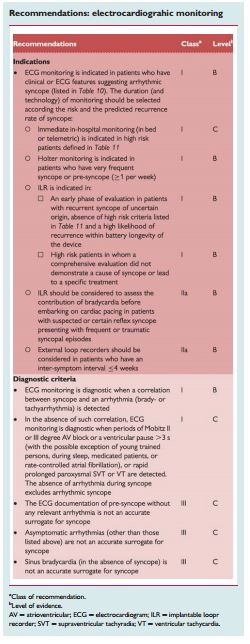
2.2.3 Electrocardiographic monitoring (non-invasive and invasive)
“ECG monitoring is a procedure for diagnosing intermittent brady- and tachyarrhythmias. Currently several systems of ECG ambulatory monitoring are available: conventional ambulatory Holter monitoring, in-hospital monitoring, event recorders, external or implantable loop recorders, and remote (at home) telemetry.”
“The gold standard for the diagnosis of syncope is when a correlation between the symptoms and a documented arrhythmia is recorded.103,104The presence of some asymptomatic significant arrhythmias, defined by prolonged asystole (≥3 s), rapid supraventricular tachycardias (SVTs) (i.e. ≥160 b.p.m. for >32 beats), or VTs, has been considered by several authors as a diagnostic finding.105–107 On the other hand, although the absence of documentation of an arrhythmia during a syncopal episode cannot be considered a specific diagnosis, it allows exclusion of an arrhythmia as the mechanism of the syncope.”
“As a general rule, ECG monitoring is indicated only when there is a high pre-test probability of identifying an arrhythmia associated with syncope (see Table 11). However, it has been observed that in patients >40 years, with recurrent syncope, without significant structural heart disease, and a normal ECG, an arrhythmia, usually asystole, is present during syncope in up to 50%.108–111 “ [Emphasis added]
2.2.3.1 In-hospital monitoring
“In-hospital monitoring (in bed or telemetry) is warranted only when the patient is at high risk for a life-threatening arrhythmia. A few days of ECG monitoring may be of value in patients with clinical features or ECG abnormalities suggesting arrhythmic syncope such as those listed inTable 11, especially if the monitoring is applied immediately after syncope. Although in such circumstances the diagnostic yield of ECG monitoring may be only as high as 16%,69 it is justified by the need to avoid immediate risk to the patient.”
2.2.3.2 Holter monitoring
“In current practice ECG monitoring is usually undertaken with conventional 24–48 h, or even 7 day, Holter recorders. However, since in most of the patients symptoms do not recur during the monitoring period, the true yield of Holter in syncope may be as low as 1–2% in an unselected population. In 15% of patients, symptoms were not associated with arrhythmia.112 Thus, in these patients, a rhythm disturbance could potentially be excluded as a cause of syncope. Holter monitoring in syncope is inexpensive in terms of set-up costs, but expensive in terms of cost per diagnosis. Holter monitoring in syncope may be of more value if symptoms are very frequent. Daily single or multiple episodes of LOC might increase the potential for symptom–ECG correlation. Experience in patients with very frequent symptoms suggests that many have psychogenic pseudosyncope. Undoubtedly, in such patients, true negative findings of Holter monitoring may be useful in confirming the underlying cause.”
2.2.3.3 Prospective external event recorders
“Event recorders are external devices which are applied by the patient when symptoms occur. Whereas these types of recorders can be useful in the investigation of patients with palpitations,113 they have no role in the evaluation of syncope.”
2.2.3.4 External loop recorders
“These devices have a loop memory that continuously records and deletes ECG. When activated by the patient, typically after a symptom has occurred, 5–15 min of pre-activation ECG is stored and can be retrieved for analysis. They are connected to the patient through cutaneous patch electrodes. Previous studies gave conflicting results about the usefulness of external loop recorders: one study showed that external retrospective loop recorders allowed ECG documentation of syncope in up to 25% of enrolled patients114 monitored for 1 month, whereas in another115external loop recorders were not useful. A recent study found that external loop recorders had an increased diagnostic yield, when compared with Holter monitoring.116 However, since patients usually do not comply for more than a few weeks, symptom–ECG correlation cannot be achieved when syncope recurrence is infrequent.”
“ILRs are implanted subcutaneously under local anaesthesia and have a battery life of up to 36 months. These devices have a solid-state loop memory that stores retrospective ECG recordings, when activated either by the patient or a bystander, usually after a syncopal episode,103,104 or automatically activated in the case of occurrence of predefined arrhythmias.105–107 Some of these devices have the capability of transmitting the signals transtelephonically. Advantages of ILRs include continuous loop high-fidelity ECG recording. Disadvantages include: the need for a minor surgical procedure, the fact that sometimes it can be difficult to differentiate between supraventricular or ventricular arrhythmias, the presence of under- or oversensing that may fill the memory, and the high cost of the implantable device. The ILR has a high initial cost. However, if symptom–ECG correlation can be achieved in a substantial number of patients during the active life of the device, then analysis of the cost per symptom–ECG yield has shown than the implanted device may be more cost-effective than a strategy using conventional investigation.117,118 In the initial experience, ILRs were used for diagnosis in patients with unexplained syncope at the end of complete negative work-up. In a small series of highly selected patients, symptom–ECG correlation was achieved in 88% of patients within a mean of 5 months of implantation.103 Pooled data from nine studies,103,104,108,119–124 including 506 patients with unexplained syncope at the end of a complete conventional investigation, show that a correlation between syncope and ECG was found in 176 patients (35%); of these, 56% had asystole (or bradycardia in a few cases) at the time of the recorded event, 11% had tachycardia and 33% had no arrhythmia. In pooled data from seven studies104,108,119–123 pre-syncope was much less likely to be associated with an arrhythmia than syncope. These data suggest that in the absence of a documented arrhythmia pre-syncope cannot be considered a surrogate for syncope; in contrast, the documentation of a significant arrhythmia at the time of pre-syncope can be considered a diagnostic finding.”
“There are several areas of interest other than unexplained syncope in which ILRs have been investigated:
-
Patients in whom epilepsy was suspected but the treatment has proven ineffective.90
-
Patients who have suspected recurrent neurally mediated syncope when the understanding of the mechanism of spontaneous syncope may alter the therapeutic approach.110
-
Patients with bundle branch block (BBB) in whom paroxysmal AV block is likely despite negative complete electrophysiological evaluation.120
-
Patients with definite structural heart disease and/or non-sustained ventricular tachyarrhythmia in whom a ventricular tachyarrhythmia is likely despite a negative complete electrophysiological study (EPS).119
-
Patients with unexplained falls.125
2.2.3.6 Remote (at home) telemetry
“Most recently, external and implantable device systems that are able to provide continuous ECG recording or 24 h loop memory, with wireless transmission (real time) to a service centre, have been developed. Daily and warning reports for predefined events are sent from the centre to the physician. Initial data showed that a mobile cardiac outpatient telemetry system had a higher diagnostic yield than a patient-activated external looping event monitor in patients with syncope or pre-syncope.126 The potential role of these systems in the diagnostic work-up of patients with syncope needs to be further evaluated.”
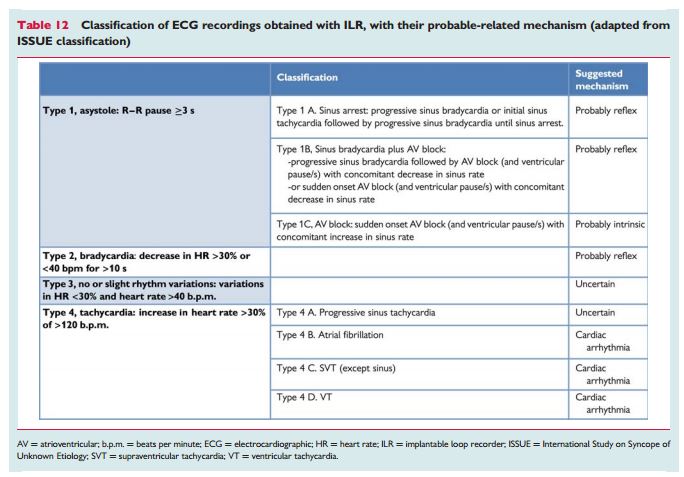
2.2.3.7 Classification of electrocardiographic recordings
“Because of the heterogeneity of findings and the wide variety of rhythm disturbances recorded with an ILR at the time of syncope, the International Study on Syncope of Unknown Etiology (ISSUE) investigators have proposed a classification aimed to group the observations into homogeneous patterns in order to define an acceptable standard useful for future studies and clinical practice.127 This classification divided ECG recordings into four groups according to the main rhythm change and the suggested mechanism of syncope (Table 12).”
2.2.3.8 Electrocardiographic monitoring in syncope—where in the work-up?
“The role of ECG monitoring cannot be defined in isolation. Physicians will be guided by the results of initial evaluation. In some situations, where the clinical evidence strongly suggests a diagnosis of reflex syncope, and especially when syncope occurs occasionally, ECG monitoring may be deemed unnecessary. In those patients with frequent symptoms or in those in whom arrhythmic syncope is suspected, but who are not at high risk, an ILR can be useful. In the initial experience, ILRs were used as last resort in the evaluation of syncope after all investigations were negative. In one study,128 60 patients with unexplained syncope were randomized to ‘conventional’ strategy consisting of an external loop recorder, tilt testing, and EPS or to prolonged monitoring with an ILR. The results were that a strategy of implantation of an ILR initially in the work-up was more likely to provide a diagnosis than the conventional strategy (52 vs. 20%). However, patients at high risk of life-threatening arrhythmias, as well as those with a left ventricular ejection fraction (LVEF) <35%, were excluded. According to these data and due to the limited diagnostic value of tilt testing,98,99 adenosine triphosphate (ATP) test,99,129 EPS,119,120 and short-term ECG monitoring (Holter, external loop recorder), it appears that early use of an ILR in the diagnostic work-up might become the reference standard to be adopted when an arrhythmic cause of syncope is suspected but not sufficiently proven to allow treatment based on aetiology.”
“Future technology may allow recording of multiple signals in addition to the ECG and will place emphasis on the features occurring during spontaneous syncope, rather than provoked syncope. For this reason it is likely that implantable monitors will become increasingly emphasized in syncope and that their use will be anticipated in the diagnostic work-up instead or before many other conventional investigations. However, in patients with important structural heart disease that expose them to a high risk of life-threatening arrhythmias, the implantation of an implantable cardioverter defibrillator (ICD) or an EPS preceding the use of ECG monitoring systems should be performed. Although the documentation of a bradyarrhythmia concurrent with syncope is considered diagnostic, further evaluation may sometimes be necessary in order to discriminate between an intrinsic cardiac abnormality and a reflex mechanism, the latter being the most frequent cause of paroxysmal bradyarrhythmia in patients without structural heart disease and normal ECG.”
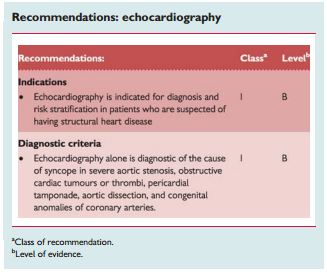
2.2.6 Echocardiography and other imaging techniques
“Echocardiography including evaluation of structural and functional haemodynamic data is a key technique to diagnose the presence of structural cardiac disease. Echocardiography plays an important role in risk stratification on the basis of LVEF. In the presence of structural heart disease, other tests to evaluate a cardiac cause of syncope should be performed. Echocardiography identifies the cause of syncope in very few patients when no more tests are needed (e.g. aortic stenosis, atrial myxoma, tamponade, etc.).”
“Transoesophageal echocardiography, computed tomography (CT), and magnetic resonance imaging (MRI) may be performed in selected cases (e.g. aortic dissection and haematoma, pulmonary embolism, cardiac masses, pericardial and myocardial diseases, congenital anomalies of coronary arteries).”
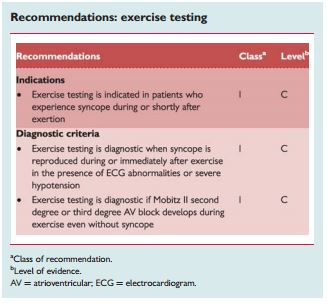
2.2.7 Exercise stress testing
“Exercise-induced syncope is infrequent. Exercise testing should be performed in patients who have experienced episodes of syncope during or shortly after exertion. Careful ECG and BP monitoring should be performed during both the test and the recovery phase as syncope can occur during or immediately after exercise. These two situations should be considered separately. Indeed, syncope occurring during exercise may be due to cardiac causes (even if some case reports showed that it might be a manifestation of an exaggerated reflex vasodilatation), whereas syncope occurring after exercise is almost invariably due to a reflex mechanism. Tachycardia-related exercise-induced second and third degree AV block has been shown to be located distal to the AV node and predicts progression to permanent AV block. Resting ECG frequently shows intraventricular conduction abnormalities.141 There are no data supporting an indication for exercise testing in a general population with syncope.”
2.2.8 Cardiac catheterization
“Cardiac catheterization techniques (e.g. coronary angiogram) should be carried out in suspected myocardial ischaemia or infarction and to rule out ischaemia-driven arrhythmias.”
2.2.9 Psychiatric evaluation
“Syncope and psychiatry interact in two ways. Various psychiatric drugs can contribute to syncope through OH and prolonged QT intervals. Disruption of a psychiatric drug regimen may have severe psychiatric consequences and should not be undertaken without relevant expertise.”
“The second interaction concerns ‘functional’ attacks. ‘Functional’ is used for conditions that resemble known somatic conditions without a somatic explanation being found, and with a presumed psychological mechanism. Two types of patients have to be included in the differential diagnosis of T-LOC. In both, patients are non-responsive and do not show normal motor control, implying that falls are common. In one type gross movements resemble epileptic seizures; these attacks have been described as ‘pseudoepilepsy’, ‘non-epileptic seizures’, ‘psychogenic non-epileptic seizures’, and ‘non-epileptic attack disorder’. In the other type there are no gross movements, so the attacks resemble syncope or longer lasting LOC. These attacks have been described as ‘psychogenic syncope’, ‘pseudosyncope’, ‘syncope of psychiatric origin’, and ‘medically unexplained syncope’. Note that the latter two terms are inconsistent with the definition of syncope because there is no cerebral hypoperfusion in functional T-LOC.”
“The basic difference between functional T-LOC and what it resembles is the absence of a somatic mechanism: in pseudoepilepsy there is no epileptiform brain activity, and in pseudosyncope BP and HR are not low, and the electroencephalogram (EEG) does not show delta activity or flattening during the attack.”
“The frequency of such attacks is not known, as they vary with the setting. Functional T-LOC mimicking epilepsy occurs in 15–20% of cases in specialized epilepsy clinics and in up to 6% in syncope clinics.142“
Diagnosis
“Pseudosyncope usually lasts longer than syncope: patients may lie on the floor for many minutes; 15 min is not exceptional. Other clues are a high frequency including numerous attacks in a day, and lack of a recognizable trigger. Injury does not exclude functional T-LOC: trauma occurred in >50% in pseudoseizures. The eyes are usually open in epileptic seizures and syncope but are usually closed in functional T-LOC. Documenting attacks is very helpful; parameters to assess are posture and muscle tone (video recording or neurological investigation), BP, HR, and EEG. The latter is feasible as functional disorders are prone to suggestion, allowing a near certain diagnosis.142 During tilt testing, the combination of apparent unconsciousness with loss of motor control, normal BP, HR, and EEG rules out syncope and most forms of epilepsy.”
“Proving the nature of attacks is useful in confirming the diagnosis. Announcing a ‘psychogenic’ diagnosis to patients may be difficult, but, without it, referral may be impossible. A psychological explanation may imply to patients that they are personally responsible or that they fake attacks on purpose. Patients see their attacks as involuntary, as they probably are. Stressing that attacks are as involuntary as syncope or an epileptic seizure avoids stigmatization, avoids counterproductive clashes, and provides a therapeutic opening.”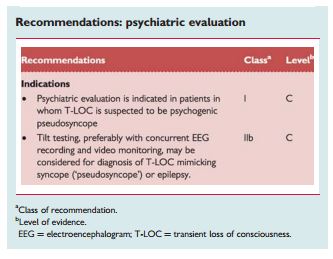
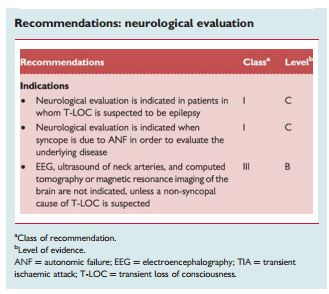
2.2.10 Neurological evaluation
“This section discusses neurological disorders causing syncope or resembling it, and neurological tests in syncope.”
2.2.10.1 Clinical conditions
Autonomic failure
“In ANF the ANS cannot cope with physiological demands, which is expressed as OH. Post-exercise hypotension, a related condition, concerns hypotension directly following the cessation of physical exercise. There are three categories of ANF.”
“Primary ANF comprises degenerative neurological disease such as pure ANF, multiple system atrophy, Parkinson’s disease, and Lewy body dementia.143
Secondary ANF involves autonomic damage by other diseases, such as diabetes mellitus, amyloidosis, and various polyneuropathies.143“
“Drug-induced OH is the most frequent cause of OH; drugs commonly causing OH are antihypertensives, diuretics, tricyclic antidepressives, phenothiazines, and alcohol. While in primary and secondary ANF the dysfunction is due to structural damage to the ANS system (either central or peripheral), in drug-induced OH the failure is functional.”
“Neurological evaluation should be considered in primary ANF. Warning signs are early impotence and disturbed micturition, and later Parkinsonism and ataxia. Referral in secondary ANF and in drug-induced OH depends on which physician treats the underlying disease.”
Cerebrovascular disorders
“Subclavian steal’ refers to rerouting of blood flow to the arm through the vertebral artery due to stenosis or occlusion of the subclavian artery. TIA may occur when flow through the vertebral artery cannot supply both the arm and part of the brain, during forceful use of the arm. Steal most often affects the left side. When detected with ultrasound, ‘steal’ is asymptomatic in 64%.144 A TIA is only likely to be due to steal when it is vertebrobasilar (see below) and associated with exercise of one arm. There are no reliable reports of isolated LOC without focal neurological symptoms and signs in subclavian steal.”
“TIA related to a carotid artery does not cause T-LOC. When almost all cerebral arteries are occluded, transient obstruction of the remaining vessel subtending a large portion of the brain may extremely rarely affect consciousness only in the standing position. Moreover, focal neurological signs are much more prevalent.”
“TIA of the vertebrobasilar system can cause LOC, but there are always focal signs, usually limb weakness, gait and limb ataxia, oculomotor palsies, and oropharyngeal dysfunction. For all practical purposes a TIA concerns a focal deficit without LOC, and syncope the opposite.”
Migraine
“Syncope occurs more often in patients with migraine, who have a higher lifetime prevalence of syncope and often frequent syncope.145 Syncopal and migraine attacks do not usually occur together in these patients.”
Epilepsy
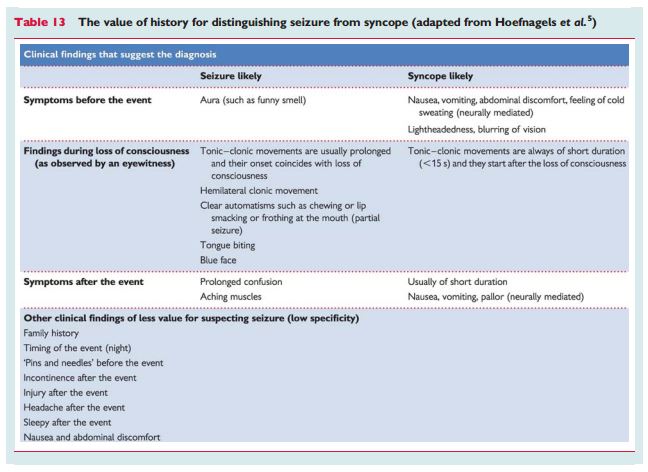
“Epilepsy can cause T-LOC: patients are non-responsive, fall, and later have amnesia. This only occurs in tonic, clonic, tonic–clonic, and atonic generalized seizures. In absence epilepsy in children and partial complex epilepsy in adults consciousness is altered, not lost; these patients remain upright during attacks, in contrast to T-LOC.”
“Complete flaccidity during unconsciousness argues against epilepsy. The only exception is ‘atonic seizure’, but it is rare, and occurs without a trigger in children with pre-existing neurological problems. Movements can be present in both epilepsy and syncope. In epilepsy movements last ∼1 min and, in syncope, seconds. The jerks in epilepsy are coarse, rhythmic, and usually synchronous, whereas those in syncope are usually asynchronous, small, and non-rhythmic. However, synchronous jerks may occur in syncope,146 and eyewitnesses may incorrectly report movements.147 In syncope movements only occur after the onset of unconsciousness and after the fall; this is not the case in epilepsy.”
“Syncope is usually triggered; epilepsy rarely is. The triggers in reflex epilepsy such as flashing lights differ from those in syncope. A typical aura consists of a rising sensation in the abdomen (epigastric aura) and/or an unusual unpleasant smell. A rising sensation may rarely occur in syncope. Sweating and pallor are uncommon in epilepsy. A tongue bite occurs much more often in epilepsy and is on the side of the tongue whereas it is the tip in syncope.5,147 Urinary incontinence occurs in both. Patients may be confused post-ictally a long time in epilepsy, whereas in syncope clearheadedness is usually immediate (Table 13). Headache, muscle pain, and elevation of creatinine kinase and prolactin are more frequent after epilepsy.”
“Cataplexy concerns paresis or paralysis triggered by emotions, usually laughter. Patients are conscious, so there is no amnesia. Together with daytime sleepiness cataplexy ensures a diagnosis of narcolepsy.”
“Falls may be due to syncope; elderly subjects may not be aware of having lost consciousness. In some subjects disorders of posture, gait, and equilibrium may mimic falls in syncope.”
“The term ‘drop attacks’ is variably used for Menière’s disease, atonic epileptic seizures, and unexplained falls. The clearest use of the term concerns middle-aged women (rarely men) who suddenly find themselves falling.148 They remember hitting the floor. Unexplained falls deserve medical attention.148“
2.2.10.2 Neurological tests
Electroencephalography
“Interictal EEGs are normal in syncope.5,149 An interictal normal EEG cannot rule out epilepsy, but must always be interpreted in a clinical context. When uncertain it is better to postpone the diagnosis of epilepsy than falsely diagnose it.”
“An EEG is not recommended when syncope is the most likely cause of T-LOC, but it is when epilepsy is the likely cause or when clinical data are equivocal. The EEG may be useful to establish psychogenic pseudosyncope, if recorded during a provoked attack.”
Computed tomography and magnetic resonance imaging
“No studies evaluated the use of brain imaging for syncope. CT or MRI in uncomplicated syncope should be avoided. Imaging may be needed based on a neurological evaluation.”
Neurovascular studies
“No studies suggest that carotid Doppler ultrasonography is valuable in patients with typical syncope.”
The treatment of syncope from the 2009 ESC Syncope Guidelines is covered an upcoming post.
______________________________________________________________
Resources
*Guidelines for the diagnosis and management of syncope (version 2009) (PDF) The Task Force for the Diagnosis and Management of Syncope of the European Society of Cardiology (ESC)
AHA/ACCF Scientific Statement on the Evaluation of Syncope AHA Scientific Statements. Circulation 2006; 113: 316-327.
ACCA Clinical Decision-Making Toolkit
A key instrument for quality improvement and clinical training. Acute Cardiovascular Care Association: a community of the European Society of Cardiology for all clinicians involved in the acute care of cardiovascular patients.
CRITICAL CONCERNS IN SPORTS MEDICINE
Audio-Digest Family Practice
Volume 62, Issue 12
March 28, 2014
Screening Young Athletes for Heart Conditions (Summary) – John R. Dylewski, MD
Postconcussion Syndrome: A Clinical Update – Chantel Debert, MD
Resources for Non-invasive Hemodynamic Monitoring
Real-time Continuous Beat-to-Beat Noninvasive Blood Pressure (NIBP100D). This is a commercially available system and on the company’s website is a PDF article, Continuous non-invasive arterial pressure shows high accuracy in comparison to invasive intra-arterial blood pressure measurement. Unfortunately, it’s usefulness is seriously compromised because it is undated and apparently not published in any journal.
Noninvasive continuous hemodynamic monitoring J Clin Monit Comput. Aug 2012; 26(4): 267–278. Published online Jun 14, 2012. doi: 10.1007/s10877-012-9375-8. The above link is to the free full-text article archived in PubMed Central (PMC) [PMC has a number of unique advantages for researcher and clinician].
Resources for the Prevention of Sudden Death
Guidelines for Risks and Prevention of Sudden Cardiac Death (JCS 2010) –Digest Version – JCS Joint Working Group. Circulation Journal, Official Journal of the Japanese Circulation Society.
American Heart Association/American College of Cardiology Foundation/Heart Rhythm Society scientific statement on noninvasive risk stratification techniques for identifying patients at risk for sudden cardiac death: a scientific statement from the American Heart Association Council on Clinical Cardiology Committee on Electrocardiography and Arrhythmias and Council on Epidemiology and Prevention. Circulation. 2008 Sep 30;118(14):1497-1518. (Full Text HTML) (Full Text PDF).
ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death–executive summary. Eur Heart J. 2006 Sep;27(17):2099-140.
ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death). European Heart Journal (2006) 8, 746-837.