In Resources at the end of this post, be sure and review Resources (2) and (3) for details on how to use point of care ultrasound (POCUS) for the diagnosis of acute dyspnea.
The following are excerpts from Resource (1) below:
Epidemiology
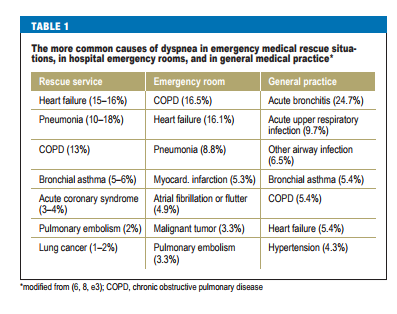
Dyspnea is a common symptom both in general practice and in hospital emergency rooms. It has been reported that 7.4% of patients presenting to emergency rooms complain of dyspnea (4); among patients in general practice, 10% complain of dyspnea when walking on flat ground and 25% complain of dyspnea on more intense exertion, e.g., climbing stairs (5). For 1–4% of patients, dyspnea is their main reason for consulting a doctor (6, 7). In specialty practice, patients with chronic dyspnea account for 15–50% of those seen by cardiologists and just under 60% of those seen by pneumonologists (2). 12% of patients seen by emergency medical rescue teams have dyspnea, and half of them need to be hospitalized; those who are hospitalized have an in-hospital mortality of ca. 10% (8). The distribution of underlying diagnoses varies from one care situation to another, as shown in Table 1. A more
Acute dyspnea
Dyspnea of acute onset may be a manifestation of avlife-threatening condition. Alarm signs include confusion, marked cyanosis (as a new finding), dyspnea while speaking, and insufficient respiratory effort or respiratory exhaustion. The potential threat to life should be assessed at once. Measurement of the vital signs (heart reate, blood pressure, oxygen saturation
of the blood) is obligatory for timely decision-making about what to do next, in particular whether the patient acutely needs to be treated in an intensive care unit or to receive invasive assisted ventilation. The respiratory rate is a further important criterion for the acuity and severity of the condition. An elevated
respiratory rate on admission to the hospital indicates a worse outcome (higher likelihood of treatment in an intensive care unit, higher mortality) (10, 11) and is an independent parameter in many score systems in emergency medicine and intensive care (e.g., the Emergency Severity Index and the APACHE II).
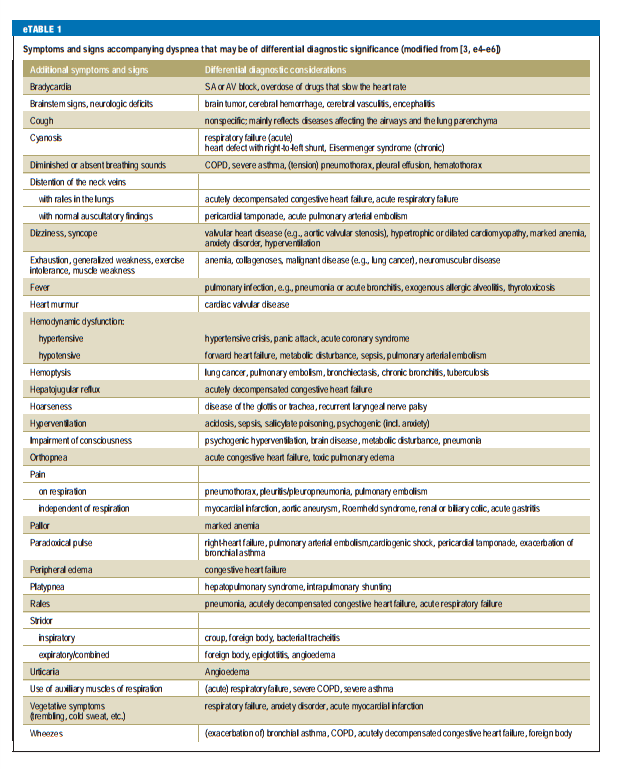
Initial misdiagnoses lead to prolonged hospitalization and are associated with higher mortality (12). Most persons who suddenly develop dyspnea feel themselves to be in grave danger. Often, emotional factors such as panic, anxiety, and frustration additionally worsen the patient’s subjective distress. Further clues to the underlying disease can be derived from the patient’s past medical history (including diagnoses, interventions, and operations) and from symptoms and signs other than dyspnea that point toward particular diagnoses (Table 2, eTable 1). The
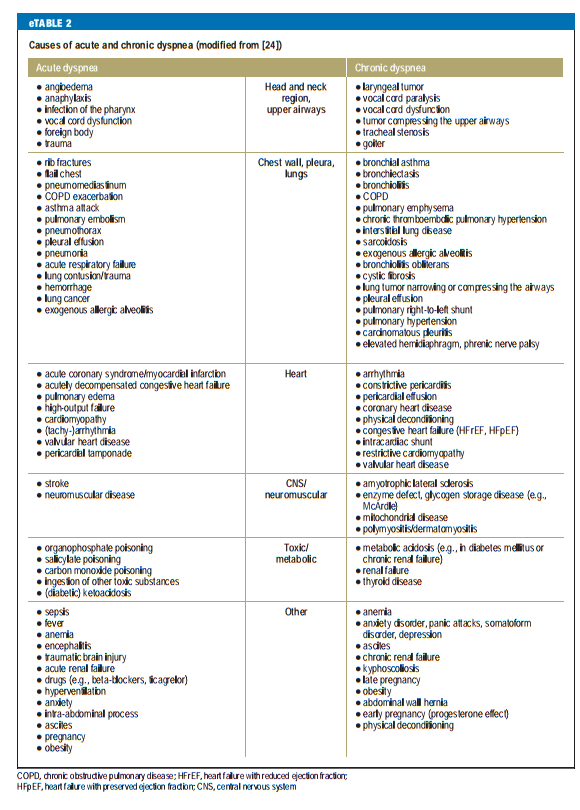
possible causes of acute dyspnea are listed in eTable 2.
The following is from the show notes of the Acute Pulmonary Edema post from Core EM:
Point of Care Ultrasound (POCUS)
- POCUS is an important diagnostic modality in patients with suspected APE
- In patients with APE, POCUS will demonstrate the presence of “B-lines”
- The presence of > 3 B-lines per rib space suggests the presence of interstitial pulmonary fluid.
- Read More: Lichtenstein’s BLUE Protocol
For more on the Blue Protocol in Point of Care Ultrasound (POCUS) for the evaluation of acute dyspnea and acute respiratory failure please see Resources (2) and (3) below.
The role of biomarkers
An acute myocardial infarction or cardiac arrhythmia can be detected with an ECG. A plain chest x-ray can reveal pulmonary congestion, pneumothorax, or pneumonia.* Specific blood tests called biomarkers also play an important role in the differential diagnosis of acute dyspnea.
[Note that currently point of care ultrasound (POCUS) can rapidly and reliably detect pulmonary congestion and pneumothorax and often pneumonia. See Resources (2) and (3) in the Resources section at the end of the post].
Natriuretic peptides
The natriuretic peptides, brain natriuretic peptide (BNP) and N-terminal prohormone brain natriuretic peptide (NT-proBNP), are useful for the exclusion of clinically relevant congestive heart failure (13–16). In its guidelines, the European Society of Cardiology (ESC) recommends threshold values of <100 pg/mL for BNP and <300 pg/mL for NT-proBNP to rule out acute congestive heart failure (17). Note that the thresholds for patients with symptomatic chronic congestive heart failure are markedly lower (<35 pg/ mL and <125 pg/mL, respectively). The negative predictive value of the natriuretic peptides for the exclusion of congestive heart failure is reportedly 94% to 98% (17)
Troponins
If the clinical evidence points to an acute coronary syndrome as the cause of dyspnea, serial deter – mination of cardiac troponin (troponin I or troponin T) is helpful. This can be used to rule out acute myo – cardial ischemia with a high degree of certainty (18); the threshold value (or threshold rise in values) for a positive test result depends on the particular test used. The positive predictive value of repeated troponin measurement for acute myocardial ischemia is 75% to 80% (18).
D-dimers
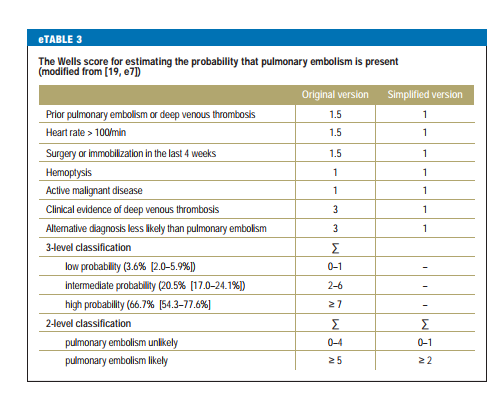
D-dimers are fibrin degradation products generated by fibrinolysis; they are found in higher concentrations after thrombotic events. They have a high negative predictive value in the diagnostic evaluation of pulmonary embolism but are not useful as a screening test for it, as an elevated D-dimer concentration is not specific. In routine practice, before D-dimers are measured, the probability of an acute pulmonary embolism should be assessed by other means first, e.g., with risk scores such as the Geneva Score or the somewhat more commonly used Wells Score (eTable 3).* If the likelihood of pulmonary embolism is low (or, in some cases, intermediate), a normal D-dimer concentration rules out pulmonary embolism with high probability. On the other hand, if the Wells Score is high, indicating that pulmonary embolism is very likely, the next step in the diagnostic evaluation is an imaging study. Moreover, it is emphasized in the current guidelines for the diagnosis and treatment of pulmonary embolism that the use of age-adjusted threshold values (age × 10 µg/L for patients over age 50) markedly improves the specificity of the D-dimer test, while keeping its sensitivity above 97% (19, 20).
[*For an excellent discussion of Pulmonary Embolism Clinical Scoring Systems Overview updated July 14, 2017 from emedicine.medscape.com. See also Modified Wells Scoring System, Revised Geneva Scoring System, Simplified Revised Geneva Score, Gestalt, PERC Rule all from the emedicine article. You can see the whole article on one page at Show All.]
Cardiac troponins and natriuretic peptides can also be elevated in patients with an acute pulmonary embolism leading to clinically relevant right-heart strain (19). Troponin can, in fact, be elevated in any acute pulmonary disease. If there is any evidence of clinically relevant right-heart strain, the patient should be evaluated in a timely fashion by transthoracic echocardiography. [Emphasis Added]
Chronic dyspnea
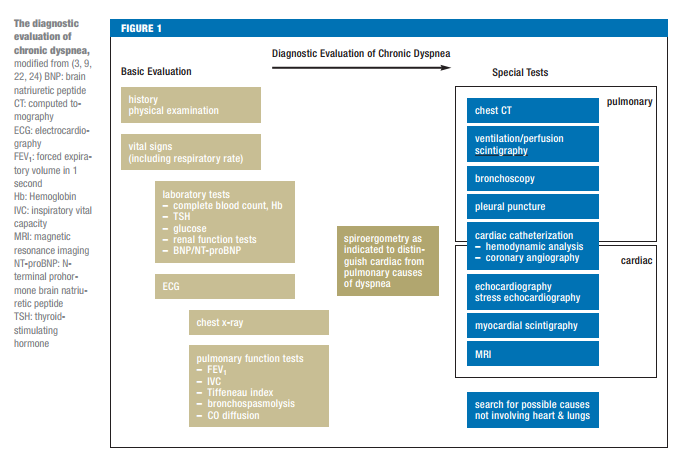
Chronic dyspnea is usually due to one of a small number of causes: bronchial asthma, COPD, congestive heart failure, interstitial lung disease, pneumonia, and mental disorders (e.g., anxiety disorders, panic disorders, somatization disorders) (3, 12). Further causes are given in eTable 2. In older, multimorbid patients, however, it is often difficult to ascribe dyspnea to a single cause. Here, too, the clinical history (including risk factors, exposures, and prior illnesses [Table 2, eTable 1]) often points toward the correct diagnosis or at least narrows down the differential diagnosis. However, a correct diagnosis is made on the basis of the history alone in only one-half to two-thirds of cases (21–23). Along with auscultation (revealing, e.g., evidence of pulmonary congestion, or absent or enhanced breathing sounds), observation of the patient’s breathing pattern often yields further clues to the probable underlying illness. Rapid, shallow breathing reflects the diminished pulmonary compliance of interstitial lung disease, while deep, slow breathing is typical of COPD (24).
Every dyspneic patient requires an oxygen saturation (oximetry) in addition to the tests in the following table.
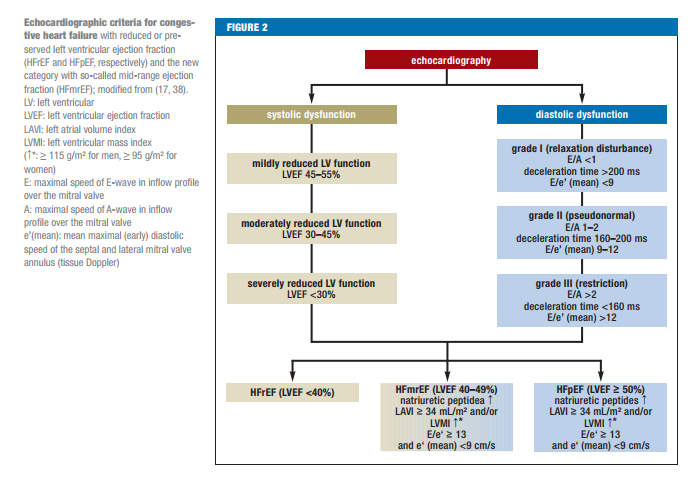
The chart below gives information on the use of echocardiogram in the diagnosis of congestive heart failure:
A fundamental consideration in the evaluation of dyspnea
Heart and lung diseases are often present in the same patient at the same time. If a cause for dyspnea is found in one of these two organ systems, the search must continue for a possible additional cause in the other organ system, as comorbidity is very common.
Dyspnea due to diseases outside the respiratory and cardiovascular systems
The World Health Organization (WHO) defines anemia as a hemoglobin (Hb) value below 8.06 mmoL/L (13 g/dL) in men or 7.44 mmoL/L (12 g/dL) in women. There is no sharp threshold value of Hb below which anemic patients become dyspneic. Anemia calls for further diagnostic evaluation in all cases, particularly if the Hb concentration is below 11 g/dL or has fallen for unclear reasons.
Diseases of the ears, nose, and throat that affect the airways can also cause dyspnea. In disturbances of the upper airways, the main symptom other than dyspnea is stridor (expiratory in bronchopulmonary airway compromise, inspiratory in supraglottic airway compromise, biphasic in airway compromise at or just below the glottis). A rule of thumb states that dyspnea arises when the tidal volume is reduced by 30% (e1). Possible causes include congenital malformations, infections, trauma, neoplasia, and neurogenic disturbances.
Neuromuscular diseases that can cause dyspnea include muscle diseases such as Duchenne muscular dystrophy, myasthenia, motor neuron diseases such as amyotrophic lateral sclerosis, and neuropathies such as Guillain-Barré syndrome (e1). In most cases, these diseases have other neurological manifestations aside from dyspnea.
Mental illnesses such as anxiety disorders, panic disorders, somatization disorders, or “functional complaints” should be regarded as diagnoses of exclusion after an extensive somatic work-up has been performed. Improvement of dyspnea with distraction or physical exercise may be a clue to a disturbance of this type.
Finally, iatrogenic (pharmacological) causes of dyspnea deserve mention as well. Non-selective betablockers can cause bronchospasm via their β2-blocking effect and thereby precipitate attacks of dyspnea. Nonsteroidal anti-inflammatory drugs that inhibit cyclo-oxygenase 1 lead to increased conversion of arachidonic acid to leukotrienes through the activity of lipo-oxygenases; leukotrienes, in turn, can cause bronchoconstriction. Moreover, acetylsalicylic acid (a member of this group of drugs), if given in high doses, can also induce dyspnea via central receptors. Dyspnea due to the platelet aggregation inhibitor ticagrelor is surely a rare event in routine practice, although the initial PLATO study (e2) revealed that it arose in 13.8% of patients. The effect is probably mediated by adenosine receptors.
Resources:
(1) The Differential Diagnosis of Dyspnea [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Dtsch Arztebl Int. 2016 Dec 9;113(49):834-845. doi: 10.3238/arztebl.2016.0834.
(2) Lung Ultrasound Signs From “BLUE-Protocol and FALLS-Protocol: Two Applications of Lung Ultrasound in the Critically Ill”
Posted on September 9, 2016 by Tom Wade MD.
This post covers the ten lung ultrasound signs that you need to master to diagnose the causes of acute respiratory failure with lung point of care ultrasound.
(3) Lung Ultrasound Profiles From the BLUE Protocol – “BLUE-Protocol and FALLS-Protocol: Two Applications of Lung Ultrasound in the Critically Ill”
Posted on September 13, 2016 by Tom Wade MD.
This post discusses the [Eight] Lung Ultrasound Profiles of the BLUE protocol [decision tree] from BLUE-protocol and FALLS-protocol: two applications of lung ultrasound in the critically ill[PubMed Abstract] [Full Text HTML] [Full Text PDF]. Chest. 2015 Jun;147(6):1659-70. doi: 10.1378/chest.14-1313.