Here is a link to 33 review articles on tranexamic acid compiled by PubMed.
What follows are excerpts from Tranexamic acid for treatment and prophylaxis of bleeding and hyperfibrinolysis [PubMed Abstract] [Full Text HTML] [Full Text PDF]:
Summary Uncontrolled massive bleeding with subsequent
derangement of the coagulation system is
a major challenge in the management of both surgical
and seriously injured patients. Under physiological
conditions activators and inhibitors of coagulation
regulate the sensitive balance between clot formation
and fibrinolysis. In some cases, excessive and diffuse
bleeding is caused by systemic activation of fibrinolysis,
i. e. hyperfibrinolysis (HF). Uncontrolled HF is
associated with a high mortality. Polytrauma patients
and those undergoing surgical procedures involving
organs rich in plasminogen proactivators (e. g. liver,
kidney, pancreas, uterus and prostate gland) are at
a high risk for HF. Antifibrinolytics, such as tranexamic
acid (TXA) are used for prophylaxis and treatment of
bleeding caused by a local or generalized HF as well as
other hemorrhagic conditions. TXA is a synthetic lysine
analogue that has been available in Austria since 1966. TXA is of utmost importance in the prevention and treatment of traumatic and perioperative bleeding due to the resulting reduction in perioperative blood loss and blood transfusion requirements. The following article presents the different fields of application
of TXA with particular respect to indications and dosages, based on a literature search and on current guidelines.Diagnosis
Diagnosing HF often proves difficult, since no specific tests that would allow prompt therapeutic decisions are currently available. . . .
Mode of action of tranexamic acid
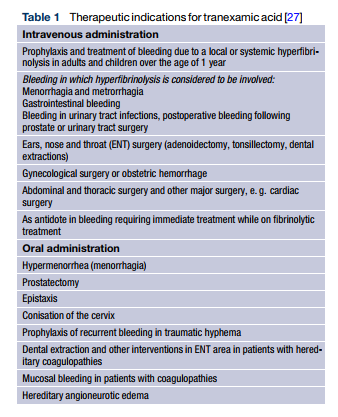
TXA is a synthetic lysine analogue that inhibits conversion of plasminogen to plasmin by preventing plasminogen from binding to the fibrin molecule. TXA also inhibits plasmin activity directly, although only at higher doses [24]. TXA inhibits fibrin cleavage, thus reducing the risk of hemorrhage. It also blocks binding of α2-antiplasmin and inhibits inflammatory reactions. Compared with epsilon-aminocaproic acid (EACA), TXA is more potent by a factor of 10 [25]. The substance can be administered orally or intravenously (Table 1), its oral bioavailability ranging from 30–50%. With a plasma protein binding of 3% it can completely cross the placenta. Metabolism of TXA in the liver is low, renal clearance amounts to 95% [26], and the halflife in adults is approximately 2.3 h [27].
TXA not recommended by the authors
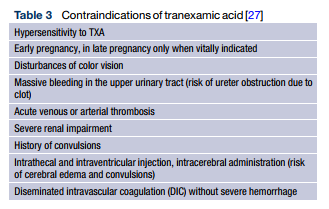
According to expert opinion, administration of TXA is not recommended in the following cases:
- Renal failure
- Epilepsy
- Benign gynecological interventions (e. g. myomectomy)
- In combination with activated factor concentrate (FEIBA, factor VIII inhibitor bypass activity; 1 ml = 25 E* factor VIII inhibitor bypass activity; see footnote 3)
- Fibrinolysis due to disseminated intravascular coagulation without any significant bleeding
If TXA were still to be administered, this should only be done in patients in whom an activation of the fibrinolytic system preponderates and in the presence of severe bleeding.
Resources:
(1) Tranexamic acid for treatment and prophylaxis of bleeding and hyperfibrinolysis [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Wien Klin Wochenschr. 2017; 129(9): 303–316. Published online 2017 Apr 21. doi: 10.1007/s00508-017-1194-y
PMCID: PMC5429347