The following are excerpts from the show notes of Episode 101 GI Bleed Emergencies Part 1 [link is to the podcast and show notes] from Emergency Medicine Cases:
This is EM Cases Episode 101 GI Bleed Emergencies Part 1
Join Anand Swaminathan, Salim Rezaie and Jeannie Callum to discuss the management of some of our most challenging GI bleed emergencies. In this Part 1 of our two part podcast on GI bleed emergencies we answer questions such as: How do you distinguish between an upper vs lower GI bleed when it’s not so obvious clinically? What alterations to airway management are necessary for the GI bleed patient? What do we need to know about the value of fecal occult blood in determining whether or not a patient has a GI bleed? Which patients require red cell transfusions? Massive transfusion? Why is it important to get a fibrinogen level in the sick GI bleed patient? What are the goals of resuscitation in a massive GI bleed? What’s the evidence for using an NG tube for diagnosis and management of upper GI bleeds? In which patients should we give tranexamic acid and which patients should we avoid it in? How are the indications for massive transfusion in GI bleed different to the trauma patient? What are your options if the bleeding can’t be stopped on endoscopy? and many more…
Be sure and review the complete show notes and podcast because these are just excerpts for my quick review–there is much more information that needs to be reviewed:
How to distinguish LGIB from UGIB
Distinguishing LGIB from UBIB is not always obvious clinically.
STEP 1: Is the patient hemodynamically unstable?
As a general rule, if a patient is hemodynamically unstable, assume UGIB because UGIB is more prevalent and is associated with a higher mortality.
STEP 2: Is there bright red blood per rectum (BRBPR) with clots or hematemesis?
BRBPR with clots can be considered almost pathognomonic for a LBIB while hematemesis can be for an UGIB source.
Note that LGIB can manifest as melena* and conversely, brisk upper GI bleed can manifest as hematochezia (without clots) in about 15% of cases. Melena on history was found to have an 80% sensitivity for UBIB with a +LR = 5.9 in a large systematic review in JAMA 2012 [1].
*melena – Melena or melæna refers to the dark black, tarry feces that are associated with upper gastrointestinal bleeding. The black color and characteristic strong odor are caused by hemoglobin in the blood being altered by digestive enzymes and intestinal bacteria. From Wikipedia
**hematochezia – Hematochezia is the passage of fresh blood through the anus, usually in or with stools (contrast with melena). From Wikipedia.
STEP 3:Calculate the BUN: Creatinine Ratio and consider the patient’s age.
The same JAMA systematic review found that a BUN:Cr ratio >30 is 93% specific for UGIB, with a +LR = 7.5. Note the units are mg/dL as used in the U.S. For other countries first divide the Creatinine by 88.42 (or roughly 100) before calculating the ratio.
Age less than 50 years has a specificity of 92% and +LR = 2.5 for UGIB source.
A study examining ED predictors of UGIB without hematemesis in 2006 found that 3 factors independently predict an UGIB source [2]:
- Melena
- BUN:creatinine ratio >30
- Age < 50 years
Imitators of melena
Remember the imitators of melena such as iron, bismuth and black foods like black licorice. While many patients describe their stool as black, true melena is pitch black against white paper, is of tarry consistency and has a certain putrid odour.
Airway Pearls & Pitfalls in GI bleed emergencies
Securing the airway in patients actively hemorrhaging from an UGIB is both a priority and a challenge. You may need to alter your standard approach.
- Direct laryngoscopy might give the best view. Video devices are easily obstructed by blood. Consider a video device equipped with a standard direct blade in case blood obstructs the camera.
- Empty the stomach prior to intubation with an NG tube and prokinetic agents (metoclopramide, erythromycin).
- Lower on the induction dose to avoid hypotension( eg 50% ketamine), don’t skimp on the paralytic (to avoid vomiting with aspiration).
- Pre-oxygenate during setup without bagging. Bagging these patients may cause further vomiting and aspiration.
- Decontaminate the airway by placing the patient in Trendelenburg if they vomit and using a double suction setup including a meconium aspirator if available.
- Consider SALAD (Suction Assisted Laryngoscopy, Airway Decontamination) as described on LITFL and EMCrit.
- Have “push dose pressors” ready in the event of sudden deterioration
Upper GI Bleed
Peptic Ulcer Disease (PUD) is the most common UGIB in all comers is from PUD in up to 67% of cases.
Varices should be assumed the cause of UGIB in those with evidence of liver disease. These are high pressure systems that can bleed quickly. These patients often have co-morbidities that reduce their physiologic reserve.
Aorto-enteric fistulae cause rapid and severe bleeding that is rarely indolent. Look for surgical scars. These patients die quickly.
Timing and location of endoscopy
Based on a 2016 systematic review of 12,000 patients [11] endoscopy within 6-24 hours of presentation has a lower in-hospital mortality compared with endoscopy outside this time frame for all patients except those that are stable with an American Society of Anesthesiologist (ASA) score of 1-2.
For unstable patients, the sooner the better, but don’t forget to “resuscitate before you endoscopate” as patients who are not fully resuscitated prior to endoscopy are at high risk of crashing during endoscopy.
The location of endoscopy depends on several factors. Hemodynamically unstable patients, those with active hematemesis and those with ongoing resuscitation should be scoped in the ED.
What is the next step if the culprit lesion cannot be found on endoscopy?
The next step after a failed endoscopy depends on how stable the patient is. For unstable patients a rapid surgical and interventional radiology consult is paramount. For stable patients, CT angiography can be valuable in locating the source of bleeding.
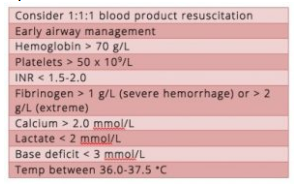
Goals of resuscitation for massive GI bleed
There is little data to guide our resuscitation in this patient population. Extrapolating from trauma literature, there are a few goals recommended by Dr. Callum:
Balloon Tamponade
Balloon tamponade is generally only indicated in the crashing, GI bleed patient in whom endoscopy is not immediately available. Familiarize yourself with the procedure and where the gear is kept in your ED.
EM Curious has a nice review here
Fist10EM runs through the procedure here
EMcrit excellent videos and cheat sheet on Blakemore tube placement